Factores asociados con el deterioro funcional en adultos mayores mexicanos
Resumen
Introducción. El deterioro funcional está relacionado con muchos resultados adversos.
Objetivo. Explorar la relación de los factores sociodemográficos, médicos y psicológicos con la incidencia del deterioro funcional en los adultos mayores mexicanos.
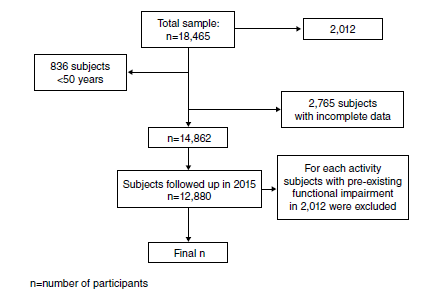
Materiales y métodos. Se analizaron los datos de las cohortes de 2012 y 2015 de la encuesta del Estudio Mexicano de Salud y Envejecimiento. Se excluyeron los participantes con discapacidad funcional en el período de referencia (2012). Se evaluó de forma individual el deterioro funcional en las actividades básicas de la vida diaria (AVD) y en las instrumentales (AIVD).
Resultados. Se encontró que el dolor, las comorbilidades, el nivel educativo, el estatus socioeconómico y la depresión se asociaban independientemente con el deterioro de las AVD. El deterioro de las AIVD se asoció con la edad, la educación deficiente, las comorbilidades, la depresión y el deterioro cognitivo.
Conclusiones. La edad, el sexo, el estado financiero, el nivel educativo, el dolor y el número de comorbilidades se asociaron con la incidencia del deterioro funcional. El dolor tuvo una mayor asociación con la incidencia del deterioro funcional en las AVD a los tres años, en comparación con el deterioro cognitivo. El estudio del deterioro funcional por dominios permitió recabar información más detallada para determinar los factores que pueden intervenirse con el objetivo de reducir la incidencia del deterioro funcional y la dependencia.
Descargas
Referencias bibliográficas
Lee R. The demographic transition: Three centuries of fundamental change. J Econ Perspect 2003;17:167-90. https://doi.org/10.1257/089533003772034943
Wong R, Palloni A. Aging in Mexico and Latin America. International Handbook of Population Aging. Dordrecht: Springer Netherlands; 2009. p. 231-52.
Chatterji S, Byles J, Cutler D, Seeman T, Verdes E. Health, functioning, and disability in older adults - Present status and future implications. Lancet. 2015;385:563-75. https://doi.org/10.1016/S0140-6736(14)61462-84
Gómez F, Curcio C. Geriatrics In Latin America. En: Fillit HM, Rockwood K, Your J, editors. Brocklehurst’s Textbook of Geriatric Medicine and Gerontology. 8th edition. Philadelphia: Elsevier; 2017. p. 1017-22.
Gutiérrez-Robledo LM, García-Peña M del C, Arango-Lopera VE, Pérez-Zepeda MU. Geriatría para el médico familiar. Ciudad de México: Manual Moderno; 2012. p.1-20.
Stuck AE, Walthert JM, Nikolaus T, Büla CJ, Hohmann C, Beck JC. Risk factors for functional status decline in community-living elderly people: A systematic literature review. Soc Sci Med. 1999;48:445-69. https://doi.org/10.1002/art.20968
van Der Vorst A, Zijlstra GA, De Witte N, Duppen D, Stuck AE, Kempen GIJM, et al. Limitations in activities of daily living in community-dwelling people aged 75 and over: A systematic literature review of risk and protective factors. PLOS ONE. 2016;11:1-18. https://doi.org/10.1371/journal.pone.0165127
Storeng SH, Sund ER, Krokstad S. Factors associated with basic and instrumental activities of daily living in elderly participants of a population-based survey: The Nord-Trøndelag Health Study, Norway. BMJ Open. 2018;8:1-10. https://doi.org/10.1136/bmjopen-2017-018942
Spillman BC. Changes in elderly disability rates and the implications for health care utilization and cost. Milbank Q. 2004;82:157-94. https://doi.org/10.1111/j.0887-378x.2004.00305.x
World Health Organization. World report on disability. Geneva: World Health Organization; 2011. Accessed: October 27, 2019. Available at: http://www.who.int/disabilities/world_report/2011/report/en/
United Nations, Department of Economic and Social Affairs. Ageing and disability. Accessed: October 27, 2019. Available at: https://www.un.org/development/desa/disabilities/disabilityand-ageing.html
Fried TR, Bradley EH, Williams CS, Tinetti ME. Functional disability and health care expenditures for older persons. Arch Intern Med. 2001;161:2602. https://doi.org/10.1001/archinte.161.21.2602
Saunders P. The costs of disability and the incidence of poverty. Aust J Soc Issues. 2007;42:461-80. https://doi.org/10.1002/j.1839-4655.2007.tb00072.x
Desforges JF, Applegate WB, Blass JP, Williams TF. Instruments for the functional assessment of older patients. N Engl J Med.1990;322:1207-14. https://doi.org/10.1056/NEJM199004263221707
Wang L, van Belle G, Kukull WB, Larson EB. Predictors of functional change: A longitudinal study of nondemented people aged 65 and older. J Am Geriatr Soc. 2002;50:1525-34. https://doi.org/10.1046/j.1532-5415.2002.50408.x
Reyes-Ortiz CA, Ostir G V, Peláez M, Ottenbacher KJ. Cross-national comparison of disability in Latin American and Caribbean persons aged 75 and older. Arch Gerontol Geriatr. 2006;42:21-33. https://doi.org/10.1016/j.archger.2005.06.006
Fuentes-García A, Sánchez H, Lera L, Cea X, Albala C. Desigualdades socioeconómicas en el proceso de discapacidad en una cohorte de adultos mayores de Santiago de Chile. Gac Sanit. 2013;27:226-32. https://doi.org/10.1016/j.gaceta.2012.11.005
Wong R, Michaels-Obregon A, Palloni A. Cohort profile: The Mexican Health and Aging Study (MHAS). Int J Epidemiol. 2017;46:e-2. https://doi.org/10.1093/ije/dyu263
Katz S, FORD AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. JAMA. 1963;185:914. https://doi.org/10.1001/jama.1963.03060120024016
Trigás-Ferrín M, Ferreira-González L. Escalas de valoración funcional en ancionos. Galicia Clin. 2011;72:11-6.
Lawton MP, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179-86.
Cigolle CT, Langa KM, Kabeto MU, Tian Z, Blaum CS. Geriatric conditions and disability: The health and retirement study. Ann Intern Med. 2007;147:156. https://doi.org/10.7326/0003-4819-147-3-200708070-00004
Glosser G, Wolfe N, Albert ML, Lavine L, Steele JC, Calne DB, et al. Cross-cultural cognitive examination: Validation of a dementia screening instrument for neuroepidemiological research. J Am Geriatr Soc. 1993;41:931-9. https://doi.org/10.1111/j.1532-5415.1993.tb06758.x
Mejía-Arango S, Wong R, Michaels-Obregón A. Normative and standardized data for cognitive measures in the Mexican Health and Aging Study. Salud Pública Mex. 2015;57:90-6. https://doi.org/10.21149/spm.v57s1.7594
Mejía-Arango S, Gutiérrez LM. Prevalence and incidence rates of dementia and cognitive impairment no dementia in the Mexican population. J Aging Health. 2011;23:1050-74. https://doi.org/10.1177/0898264311421199
Aguilar-Navarro SG, Fuentes-Cantú A, Ávila-Funes JA, García-Mayo EJ. Validity and reliability of the screening questionnaire for geriatric depression used in the Mexican Health and Age Study. Salud Pública Mex. 2007;49:256-62. https://doi.org/10.1590/s0036-36342007000400005
Cano-Gutiérrez C, Borda MG, Reyes-Ortiz C, Arciniegas AJ, Samper-Ternent R. Assessment of factors associated with functionality in older adults over 60 years in Bogotá, Colombia. Biomédica. 2016;37:57-65. https://doi.org/10.7705/biomedica.v37i1.3197
Laan W, Bleijenberg N, Drubbel I, Numans ME, de Wit NJ, Schuurmans MJ. Factors associated with increasing functional decline in multimorbid independently living older people. Maturitas. 2013;75:276-81. https://doi.org/10.1016/j.maturitas.2013.04.005
Brito KQ, Menezes TN de, Olinda RA de, Brito KQ, Menezes TN de, Olinda RA. Functional disability and socioeconomic and demographic factors in elderly. Rev Bras Enferm. 2015;68:633-41. https://doi.org/10.1590/0034-7167.2015680409i
Dunlop DD, Semanik P, Song J, Manheim LM, Shih V, Chang RW. Risk factors for functional decline in older adults with arthritis. Arthritis Rheum. 2005;52:1274-82. https://doi.org/10.1002/art.20968
Hoogerduijn JG, Buurman BM, Korevaar JC, Grobbee DE, de Rooij SE, Schuurmans MJ. The prediction of functional decline in older hospitalised patients. Age Ageing. 2012;41:381-7. https://doi.org/10.1093/ageing/afs015
Gomes C dos S, Maciel ÁCC, Freire A do NF, Moreira M de A, Ribeiro M De O, Guerra RO. Depressive symptoms and functional decline in an elderly sample of urban center in northeastern Brazil. Arch Gerontol Geriatr. 2014;58:214-8. https://doi.org/10.1016/j.archger.2013.10.009
Landi F, Russo A, Liperoti R, Danese P, Maiorana E, Pahor M, et al. Daily pain and functional decline among old-old adults living in the community: Results from the ilSIRENTE Study. J Pain Symptom Manage. 2009;38:350-7. https://doi.org/10.1016/j.jpainsymman.2008.10.005
Astudillo CI. Depresión como predictor de discapacidad en adultos mayores. Salud UIS. 2007;49:438-49. https://doi.org/10.18273/revsal.v49n3-2017002
Barry LC, Murphy TE, Gill TM. Depressive symptoms and functional transitions over time in older persons. Am J Geriatr Psychiatry. 2011;19:783-91. https://doi.org/10.1097/JGP.0b013e3181ff6669
Liu-Seifert H, Siemers E, Sundell K, Price K, Han B, Selzler K, et al. Cognitive and functional decline and their relationship in patients with mild Alzheimer’s dementia. J Alzheimers Dis. 2014;43:949-55. https://doi.org/10.3233/JAD-140792
Díaz-Venegas C, De La Vega S, Wong R. Transitions in activities of daily living in Mexico, 2001-2012. Salud Pública Mex. 2015;57(Suppl.1):S54-61. https://doi.org/10.21149/spm.v57s1.7590
Díaz-Venegas C, Reistetter TA, Wang C-Y, Wong R. The progression of disability among older adults in Mexico. Disabil Rehabil. 2016;38:2016-27. https://doi.org/10.3109/09638288.2015.1111435
| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |

























