Relación entre la calidad del aire y el asma en habitantes de grandes altitudes, La Paz, Bolivia (3.600 m.s.n.m.)
Resumen
Introducción. El asma es una enfermedad crónica que afecta a millones de personas en todo el mundo. La calidad del aire es uno de los factores clave que puede desencadenar los síntomas del asma.
Objetivo. Analizar la calidad del aire y su relación con el asma en habitantes de grandes altitudes en La Paz (Bolivia).
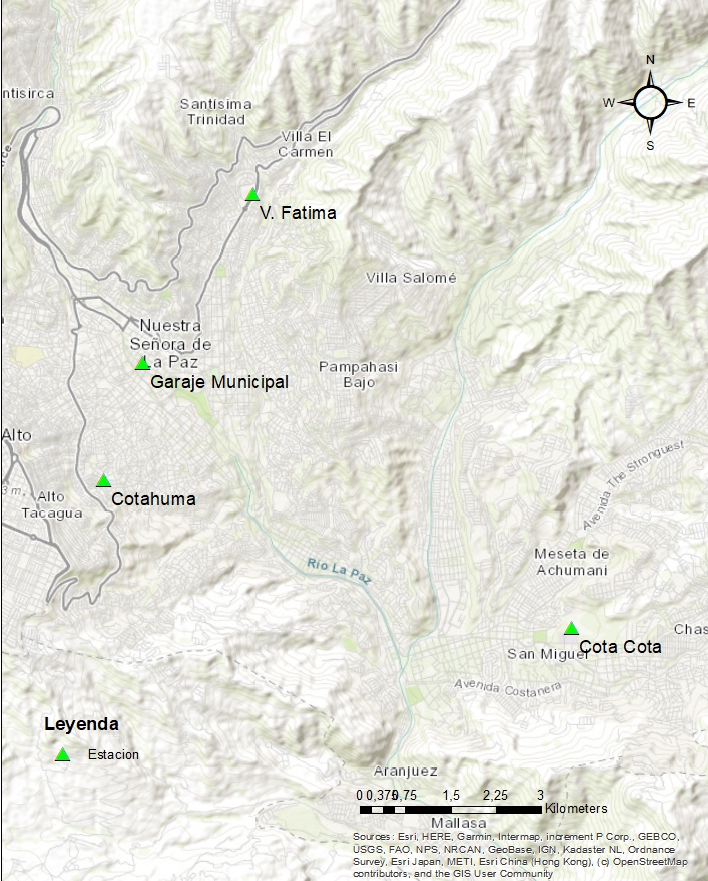
Materiales y métodos. Se desarrolló un estudio analítico, descriptivo y retrospectivo. Se recolectaron datos de pacientes con diagnóstico de asma en el Instituto Nacional del Tórax y en el Instituto Boliviano de Biología de Altura. Además, se monitoreó la calidad del aire y su material particulado en las estaciones de la “Red de monitoreo de la calidad del aire”.
Resultados. El 56,9 % de los casos fueron mujeres del Instituto Nacional del Tórax y el 45,7 % del Instituto Boliviano de Biología de Altura. En ambas instituciones, la media de edad fue de 47 años y los pacientes presentaban sobrepeso u obesidad. Se registraron incrementos de material particulado fino (PM2,5) en otoño, invierno y primavera, en 2014, 2016-2019 y en las cuatro estaciones del 2015. El material particulado inhalable grueso (PM10) se incrementó en otoño e invierno del 2014 al 2020, dentro de los límites establecidos. Se observó una asociación positiva y significativa entre la concentración de material particulado PM2,5 y los parámetros espirométricos de capacidad vital forzada, flujo espiratorio máximo y el porcentaje de reversión. La relación de partículas PM10 y los parámetros espirométricos de capacidad vital forzada, volumen espiratorio máximo en el primer segundo y flujo espiratorio máximo, también fue estadísticamente significativa.
Conclusión. Los casos de asma se presentaron en promedio a los 47 años y en personas con sobrepeso u obesidad. Se observó una asociación positiva entre el material particulado, PM2,5 y PM10, con los parámetros espirométricos, la cual fue más marcada con las partículas PM2,5.
Descargas
Referencias bibliográficas
Atkinson RW, Anderson HR, Strachan DP, Bland JM, Bremner SA, Ponce de León A. Short-term associations between outdoor air pollution and visits to accident and emergency departments in London for respiratory complaints. Eur Respir J. 1999;13:257-65. https://doi.org/10.1183/09031936.99.13225799
Anderson HR, Ponce de León A, Bland JM, Bower JS, Emberlin J, Strachan DP. Air pollution, pollens, and daily admissions for asthma in London 1987-1992. Thorax. 1998;53:842-8. https://doi.org/10.1136/thx.53.10.842
Jameson JL, Fauci AS, Kasper DL, Hauser SL, Longo DL, Loscalzo J, et al., editores. Harrison’s Principles of Internal Medicine. 20th edition. New York: McGraw-Hill Education; 2018.
Fiore AM, Naik V, Leibensperger EM. Air quality and climate connections. J Air Waste Manag Assoc. 2015;65:645-85. https://doi.org/10.1080/10962247.2015.1040526. Erratum in: J Air Waste Manag Assoc. 2015;65:1159.
Piekarska B, Stankiewicz-Choroszucha BL, Sybilski AJ, Furmańczyk K, Jaworski S, Białoszewski AZ, et al. Effect of indoor air quality on the natural history of asthma in an urban population in Poland. Allergy Asthma Proc. 2018;39:e64-70. https://doi.org/10.2500/aap.2018.39.4176
Su JG, Barrett MA, Combs V, Henderson K, van Sickle D, Hogg C, et al. Identifying impacts of air pollution on subacute asthma symptoms using digital medication sensors. Int J Epidemiol. 2022;51:213-24. https://doi.org/10.1093/ije/dyab187
Eguiluz-Gracia I, Mathioudakis AG, Bartel S, Vijverberg SJ, Fuertes E, Comberiati P, et al. The need for clean air: The way air pollution and climate change affect allergic rhinitis and asthma. Allergy. 2020;75:2170-84. https://doi.org/10.1111/all.14177
Del Giacco SR, Bakirtas A, Bel E, Custovic A, Diamant Z, Hamelmann E, et al. Allergy in severe asthma. Allergy. 2017;72:207-20. https://doi.org/10.1111/all.13072
Paciência I, Cavaleiro Rufo J, Moreira A. Environmental inequality: Air pollution and asthma in children. Pediatr Allergy Immunol. 2022;33. https://doi.org/10.1111/pai.13818
Cincinelli A, Martellini T. Indoor air quality and health. Int J Environ Res Public Health. 2017;14:1286. https://doi.org/10.3390/ijerph14111286
Chen YY, Sung FC, Chen ML, Mao IF, Lu CY. Indoor air quality in the metro system in north Taiwan. Int J Environ Res Public Health. 201;13:1200. https://doi.org/10.3390/ijerph13121200
Agencia de Protección Ambiental de los Estados Unidos. Conceptos básicos sobre el material particulado (PM, por sus siglas en inglés). Fecha de consulta: 12 de diciembre de 2023. Disponible en: https://espanol.epa.gov/espanol/conceptos-basicos-sobre-el-materialparticulado-pm-por-sus-siglas-en-ingles
Wolkoff P. Indoor air humidity, air quality, and health - An overview. Int J Hyg Environ Health. 2018;221:376-90. https://doi.org/10.1016/j.ijheh.2018.01.015
Ather B, Mirza TM, Edemekong PF. Airborne precautions. Treasure Island (FL): StatPearls Publishing; 2023.
Organización Panamericana de la Salud. Calidad del aire. Washington, D.C.: OPS. Fecha de consulta: 12 de diciembre de 2023. Disponible en: https://www.paho.org/es/temas/calidad-aire
Murillo-Jáuregui C, García MA, López JJ. Manual de espirometría y gasometría arterial en la altitud. Primera edición. La Paz: Sociedad Boliviana de Neumología; 2018. p. 1-73.
Observatorio del Derecho Humano a la Vivienda Adecuada en Bolivia. En Cochabamba da miedo respirar por su alta contaminación. Fecha de consulta: 12 de diciembre de 2023. Disponible en: https://renaseh-odhva.org/2019/10/04/en-cochabamba-da-miedo-respirarpor-su-alta-contaminacion/
Gudbjartsson T, Sigurdsson E, Gottfredsson M, Bjornsson OM, Gudmundsson G. High altitude illness and related diseases - A review. Laeknabladid. 2019;105:499-507. https://doi.org/10.17992/lbl.2019.11.257
Aldunate P, Paz O, Halvorsen K. Los efectos de la contaminación atmosférica por PM10 sobre la salud ciudad de La Paz - Bolivia (3.650 m.s.n.m.). RevActaNova. 2006;3:422-42.
Canseco A, Anze R, Franken M. Comunidades de líquenes: indicadores de la calidad del aire en la ciudad de La Paz, Bolivia. RevActaNova. 2006;3:286-307.
Guajardo N, Ramírez A, Díaz F, Castillo E, Otero A, Parra J. Concentración de las partículas totales suspendidas en la atmósfera de Caracas. Rev Fac Ing. 2010;25:73-80.
National Institute for Health and Care Excellence. Air pollution: Outdoor air quality and health. London: NICE; 2017. Fecha de consulta: 12 de diciembre de 2023. Disponible en: https://www.nice.org.uk/guidance/ng70/resources/air-pollution-outdoor-air-quality-andhealth-pdf-1837627509445
Yu S, Park S, Park CS, Kim S. Association between the ratio of FEV1 to FVC and the exposure level to air pollution in neversmoking adult refractory asthmatics using data clustered by patient in the Soonchunhyang asthma cohort database. Int J Environ Res Public Health. 2018;15:2349. https://doi.org/10.3390/ijerph15112349
Zheng XY, Ding H, Jiang LN, Chen SW, Zheng JP, Qiu M, et al. Association between air pollutants and asthma emergency room visits and hospital admissions in time series studies: A systematic review and meta-analysis. PLoS ONE. 2015;10:e0138146. https://doi.org/10.1371/journal.pone.0138146
Chanel O, Pérez L, Künzli N, Medina S; Aphekom group. The hidden economic burden of air pollution-related morbidity: Evidence from the Aphekom project. Eur J Health Econ. 2016;17:1101-15. https://doi.org/10.1007/s10198-015-0748-z
Gehring U, Wijga AH, Hoek G, Bellander T, Berdel D, Brüske I, et al. Exposure to air pollution and development of asthma and rhinoconjunctivitis throughout childhood and adolescence: A population-based birth cohort study. Lancet Respir Med. 2015;3:933-42. https://doi.org/10.1016/S2213-2600(15)00426-9
Wilson AM, Wake CP, Kelly T, Salloway JC. Air pollution, weather, and respiratory emergency room visits in two northern New England cities: An ecological time-series study. Environ Res. 2005;97:312-21. https://doi.org/10.1016/j.envres.2004.07.010
Rosenquist NA, Metcalf WJ, Ryu SY, Rutledge A, Coppes MJ, Grzymski JJ, et al. Acute associations between PM2,5 and ozone concentrations and asthma exacerbations among patients with and without allergic comorbidities. J Expo Sci Environ Epidemiol. 2020;30:795-804. https://doi.org/10.1038/s41370-020-0213-7
Swinnen K, Bijnens E, Casas L, Nawrot TS, Delcroix M, Quarck R, et al. Residential air pollution increases the risk for persistent pulmonary hypertension after pulmonary endarterectomy. Eur Respir J. 2021;57:2002680. https://doi.org/10.1183/13993003.02680-2020
James KA, Strand M, Hamer MK, Cicutto L. Health services utilization in asthma exacerbations and PM10 levels in rural Colorado. Ann Am Thorac Soc. 2018;15:947-54. https://doi.org/10.1513/AnnalsATS.201804-273OC
DuPont A. Improving and monitoring air quality. Environ Sci Pollut Res Int. 2018;25:15253-63. https://doi.org/10.1007/s11356-018-1897-2
Jiaxin C, Hui H, Feifei W, Mi Z, Ting Z, Shicheng Y, et al. Air quality characteristics in Wuhan (China) during the 2020 COVID-19 pandemic. Environ Res. 2021;195:110879. https://doi.org/10.1016/j.envres.2021.110879
Derechos de autor 2024 Biomédica

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.
| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |

























