Cost-effectiveness of diagnostic strategies of severe bacterial infection in infants with fever without a source
Abstract
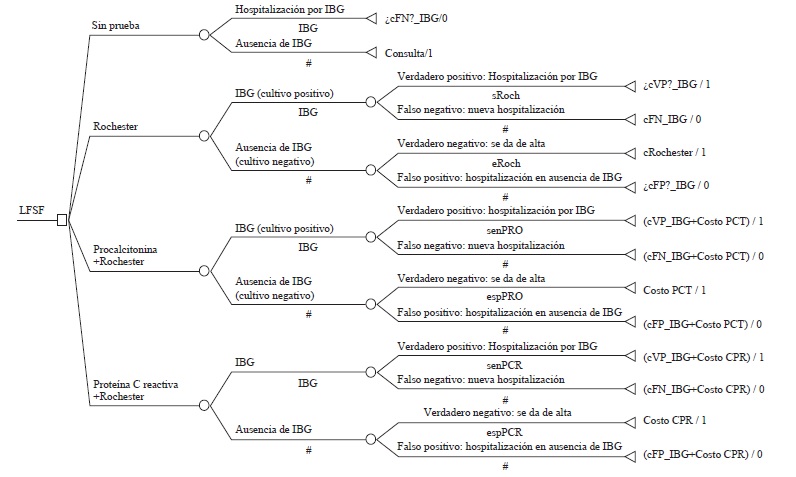
Introduction: Serious bacterial infections in infants under 2-years-of-age with fever without a source remains, despite advances in vaccination, a matter of concern for both physicians and parents. Having cost-effectiveness information is relevant to guide decision making in clinical practice in this scenario. Objective: To determine the cost-effectiveness of four different strategies of screening in Argentina for serious bacterial infection in children presenting with fever without a source. Materials and methods: We designed a decision tree to model a hypothetical cohort of 10,000 children with fever without a source. We compared the incremental cost-effectiveness of four strategies to detect serious bacterial infection: Rochester criteria + C reactive protein test, Rochester criteria + procalcitonin test, Rochester criteria, and expectant observation. Results: Rochester criteria + C reactive protein test was the most cost-effective strategy with USD$ 784 for each correctly diagnosed case versus USD$ 839 of Rochester criteria + procalcitonin test, USD$ 1,116 of expectant observation or USD$ 1,193 of Rochester criteria. When the probability of serious bacterial infections was equal or less than 14%, the strategy of choice was expectant observation. Conclusions: The Rochester criteria + C reactive protein test was the most cost-effective strategy to detect serious bacterial infection in one to three months old children with fever without a source. However, in low risk settings for such infection, the strategy of choice is expectant observation.
Downloads
References
Torregrosa C, García C, Sciarotta J, Vay C, Caíno S, Ellis A. Associated risk factors for serious bacterial illness in children less than 24 months, admitted with fever without source. Rev Chilena Infectol. 2010;27:308-14.
Watt K, Waddle E, Jhaveri R. Changing epidemiology of serious bacterial infections in febrile infants without localizing signs. PLoS One. 2010;5:e12448. http://dx.doi.org/10.1371/journal.pone.0012448
Monsma J, Richerson J, Sloand E. Empowering parents for evidence-based fever management: An integrative review. J Am Assoc Nurse Pract. 2015;27:222-9. http://dx. doi.org/10.1002/2327-6924.12152
Lacroix L, Manzano S, Vandertuin L, Hugon F, Galetto-Lacour A, Gervaix A. Impact of the lab-score on antibiotic prescription rate in children with fever without source: A randomized controlled trial. PLoS One. 2014;9:e115061. http://dx.doi.org/10.1371/journal.pone.0115061
Buendía JA, Colantonio L. Costo-efectividad de la proteína C reactiva, procalcitonina y escala de Rochester: tres estrategias diagnósticas para la identificación de infección bacteriana severa en lactantes febriles sin foco. Value Health Reg Issues. 2013;2:375-80.
National Institute for Health and Care Excellence. Feverish illness in children: Assessment and initial management in children younger than 5 years. London: NICE; 2013.
Baraff LJ. Management of infants and young children with fever without source. Pediatr Ann. 2008;37:673-9.
Craig JC, Williams GJ, Jones M, Codarini M, Macaskill P, Hayen A, et al. The accuracy of clinical symptoms and signs for the diagnosis of serious bacterial infection in young febrile children: Prospective cohort study of 15,781 febrile illnesses. BMJ. 2010;340:c1594. http://dx.doi.org/10.1136/bmj.c1594
Baraff LJ. Management of fever without source in infants and children. Ann Emerg Med. 2000;36:602-14. http://dx.doi.org/10.1067/mem.2000.110820
Davis T. NICE guideline: Feverish illness in children--assessment and initial management in children younger than 5 years. Arch Dis Child Educ Pract Ed. 2013;98:232-5. http://dx.doi.org/10.1136/archdischild-2013-304792
Barboza BG, Contte PF, Rodríguez MA, Fernández NF. Fiebre sin foco en niños de 0-36 meses. Revista de Posgrado de la VI Cátedra de Medicina. 2007;173:14-21.
Montero D, Miron L, Cheistwer A. Medicina interna para pediatras. Guía práctica. Hospital de Niños Ricardo Gutiérrez. Buenos Aires: Pzier; 2010. p. 299.
Oyamada H, Nakagomi O, Uesugi S. Quantitative assays for C-reactive protein: A review. Rinsho byori. The Japanese journal of clinical pathology. 1992;40:9-15.
Marín P, Ruiz I, Vidal S, López-Prats JL, Modesto V. Accuracy of the procalcitonin test in the diagnosis of occult bacteremia in paediatrics: A systematic review and meta-analysis. An Pediatr (Barc). 2010;72:403-12. http://dx.doi.org/10.1016/j.anpedi.2010.03.004
Manzano S, Bailey B, Gervaix A, Cousineau J, Delvin E, Girodias JB. Markers for bacterial infection in children with fever without source. Arch Dis Child. 2011;96:440-6. http://dx.doi.org/10.1136/adc.2010.203760
Anbar RD, Richardson-de Corral V, O’Malley PJ. Difficulties in universal application of criteria identifying infants at low risk for serious bacterial infection. J Pediatr. 1986;109:483-5.
Galetto-Lacour A, Gervaix A. Identifying severe bacterial infection in children with fever without source. Expert Rev Anti Infect Ther. 2010;8:1231-7. http://dx.doi.org/10.1586/eri.10.118
Lee GM, Fleisher GR, Harper MB. Management of febrile children in the age of the conjugate pneumococcal vaccine: A cost-effectiveness analysis. Pediatrics. 2001;108:835-44. http://dx.doi.org/10.1542/peds.108.4.835
Huppler AR, Eickhoff JC, Wald ER. Performance of low-risk criteria in the evaluation of young infants with fever: Review of the literature. Pediatrics. 2010;125:228-33. http://dx.doi.org/10.1542/peds.2009-1070
Thompson M, van den Bruel A, Verbakel J, Lakhanpaul M, Haj-Hassan T, Stevens R, et al. Systematic review and validation of prediction rules for identifying children with serious infections in emergency departments and urgent-access primary care. Health Technol Assess. 2012;16:1-100. http://dx.doi.org/10.3310/hta16150
Cartwright WS. Methods for the economic evaluation of health care programmes, second edition. Book review. J Ment Health Policy Econ. 1999;2:43.
Siegel C, Laska E, Meisner M. Statistical methods for cost-effectiveness analyses. Control Clin Trials. 1996;17:387-406. http://dx.doi.org/10.1016/S0197-2456(95)00259-6
Briggs A, Gray A. The distribution of health care costs and their statistical analysis for economic evaluation. J Health Serv Res Policy. 1998;3:233-45.
Elshout G, Monteny M, van der Wouden JC, Koes BW, Berger MY. Duration of fever and serious bacterial infections in children: A systematic review. BMC Fam Pract. 2011;12:33. http://dx.doi.org/10.1186/1471-2296-12-33
Andreola B, Bressan S, Callegaro S, Liverani A, Plebani M, Da Dalt L. Procalcitonin and C-reactive protein as diagnostic markers of severe bacterial infections in febrile infants and children in the emergency department. Pediatr Infect Dis J. 2007;26:672-7. http://dx.doi.org/10.1097/INF.0b013e31806215e3
Gálvez GF, Silvana A, Heavey G. Estudio descriptivo de la población atentida en consultorios externos de pediatría. Arch Argent Pediatr. 2001;99:309-16.
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























