Chagas disease reactivation after autologous stem cell transplant. Case report and literature review
Abstract
Introduction: Chagas disease is an endemic parasitic infection in Latin America transmitted by triatomines. It is associated with risk factors such as poverty and rurality. After acute infection, a third of patients will present target organ involvement (heart, digestive tract, central nervous system). The remaining two thirds remain asymptomatic throughout their life. Pharmacological immunosuppression breaks the balance between the immune system and the parasite, favoring its reactivation.
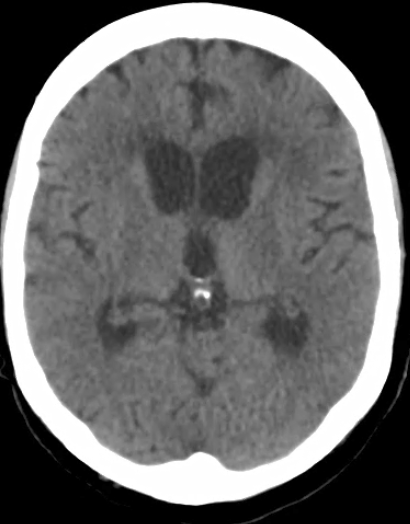
Clinical case: We present the case of a 58-year-old man from a Colombian rural area with a diagnosis of multiple myeloma refractory to the first line of treatment who required a new chemotherapy scheme and consolidation with autologous stem cell transplant. During the post-transplant period, he suffered from febrile neutropenia. Initial microbiological studies were negative but the peripheral blood smear evidenced trypomastigotes in blood. With a diagnosis of acute Chagas disease in a post-transplant patient, benznidazole was started. The evolution of the patient was satisfactory.
Conclusions: Positive serology prior to transplantation makes it necessary to rule out reactivation of the pathology in the setting of febrile neutropenia. More studies are required to determine tools for estimating the probability of reactivation of the disease and defining the best cost-risk-benefit relation for the prophylactic therapy.
Downloads
References
Rueda K, Trujillo JE, Carranza JC, Vallejo GA. Transmisión oral de Trypanosoma cruzi: una nueva situación epidemiológica de la enfermedad de Chagas en Colombia y otros países suramericanos. Biomédica. 2014;34:631-72. https://doi.org/10.7705/biomedica.v34i4.2204
World Health Organization. Chagas disease in Latin America: An epidemiological update based on 2010 estimates. Fecha de consulta: 5 de julio de 2021. Disponible en: https://www.who.int/wer/2015/wer9006.pdf?ua=1
Pereiro AC. Guidelines for the diagnosis and treatment of Chagas disease. Lancet. 2019;393:1486-7. https://doi.org/10.1016/S0140-6736(19)30288-0
Pierrotti LC, Carvalho NB, Amorin JP, Pascual J, Kotton CN, López-Vélez R. Chagas disease recommendations for solid-organ transplant recipients and donors. Transplantation 2018;102:S1-7. https://doi.org/10.1097/TP.0000000000002019
Rajkumar SV. Multiple myeloma: 2020 update on diagnosis, risk-stratification and management. Am J Hematol 2020;95:548-67. https://doi.org/10.1002/ajh.25791
Perrot A, Lauwers-Cances V, Cazaubiel T, Facon T, Caillot D, Clement-Filliatre L, et al. Early versus late autologous stem cell transplant in newly diagnosed multiple myeloma: Long-term follow-up analysis of the IFM 2009 Trial. Blood. 2020;136:39. https://doi.org/10.1182/blood-2020-134538
Pérez CJ, Lymbery AJ, Thompson RCA. Reactivation of Chagas disease: Implications for global health. Trends Parasitol. 2015;31:595-603. https://doi.org/10.1016/j.pt.2015.06.006
Jarque I, Salavert M, Pemán J. Parasitic infections in hematopoietic stem cell transplantation. Mediterr J Hematol Infect Dis. 2016;8:e2016035. https://doi.org/10.4084/MJHID.2016.035
Pinazo MJ, Espinosa G, Cortés-Lletget C, Posada EJ, Aldasoro E, Oliveira I, et al. Immunosuppression and Chagas disease: A management challenge. PLoS Negl Trop Dis 2013;7;e1965. https://doi.org/10.1371/journal.pntd.0001965
Riganti J, Maqueda MG, Piñero MCB, Volonteri VI, Galimberti RL. Reactivation of Chagas’ disease: Cutaneous manifestations in two immunosuppressed patients. Int J Dermatol. 2012;51:829-34. https://doi.org/10.1111/j.1365-4632.2011.05224.x
Pan American Health Organization. Guidelines for the diagnosis and treatment of Chagas disease. Fecha de consulta: 5 de julio de 2021. Disponible en: https://iris.paho.org/bitstream/handle/10665.2/49653/9789275120439_eng.pdf
Tomblyn M, Chiller T, Einsele H, Gress R, Sepkowitz K, Storek J, et al. Guidelines for preventing infectious complications among hematopoietic cell transplantation recipients: A global perspective. Biol Blood Marrow Transplant. 2009;15:1143-238. https://doi.org/10.1016/j.bbmt.2009.06.019
Dictar M, Sinagra A, Verón MT, Luna C, Dengra C, De Rissio A, et al. Recipients and donors of bone marrow transplants suffering from Chagas’ disease: Management and preemptive therapy of parasitemia. Bone Marrow Transplant. 1998;21:391-3. https://doi.org/10.1038/sj.bmt.1701107
Altclas J, Sinagra A, Jaimovich G, Salgueira C, Luna C, Requejo A, et al. Reactivation of chronic Chagas’ disease following allogeneic bone marrow transplantation and successful pre-emptive therapy with benznidazole. Transpl Infect Dis. 1999;1:135-7. https://doi.org/10.1034/j.1399-3062.1999.010207.x
Altclas J, Sinagra A, Dictar M, Luna C, Verón MT, De Rissio AM, et al. Chagas disease in bone marrow transplantation: An approach to preemptive therapy. Bone Marrow Transplant. 2005;36:123-9. https://doi.org/10.1038/sj.bmt.1705006
Chalela CM, Peña AM, Roa AM, Reyes DL, Rueda JP, Salazar LA, et al. Reactivation of chagas disease after autologous hematopoietic stem cell transplantation. Rev Soc Bras Med Trop. 2021;54:1-4. https://doi.org/10.1590/0037-8682-0143-2020
Diazgranados CA, Saavedra-Trujillo CH, Mantilla M, Valderrama SL, Alquichire C, Franco-Paredes C. Chagasic encephalitis in HIV patients: Common presentation of an evolving epidemiological and clinical association. Lancet Infect Dis. 2009;9:324-30. https://10.1016/S1473-3099(09)70088-X
Some similar items:
- Patricia Escobar, Katherine Paola Luna, Indira Paola Hernández, César Mauricio Rueda, María Magdalena Zorro, Simon L. Croft, In vitro susceptibility of Trypanosoma cruzi strains from Santander, Colombia, to hexadecylphosphocholine (miltefosine), nifurtimox and benznidazole , Biomedica: Vol. 29 No. 3 (2009)
- María Clara Echeverry, Nubia Catalina Tovar, Guillermo Mora, Presence of antibodies to cardiac neuroreceptors in patients with Chagas disease , Biomedica: Vol. 29 No. 3 (2009)
- Dairo Alonso Rendón, Carlos M. Genes, Omar Triana, Myocardial cellular damage and the activity of the mitochondrial ATP synthase in rats infected with a Colombian strain of Trypanosoma cruzi , Biomedica: Vol. 27 No. 1esp (2007): Enfermedad de Chagas
- Concepción Judith Puerta, Johana María Guevara, Paula Ximena Pavía, Marleny Montilla, Rubén Santiago Nicholls, Edgar Parra, Yuli Katherine Barrera, Evaluation of TcH2AF-R and S35-S36 primers in PCR tests for the detection of Trypanosoma cruzi in mouse cardiac tissue , Biomedica: Vol. 28 No. 4 (2008)
- Paula Ximena Pavía, Nubia Lucía Roa, Ana María Uribe, Concepción Judith Puerta, Using S35-S36 and TcH2AF-R primer-based PCR tests to follow-up a Chagas’ disease patient who had undergone a heart transplant , Biomedica: Vol. 31 No. 2 (2011)
- Richard Hoyos, Lisandro Pacheco, Luz Adriana Agudelo, German Zafra, Pedro Blanco, Omar Triana, Seroprevalence of Chagas disease and associated risk factors in a population of Morroa, Sucre , Biomedica: Vol. 27 No. 1esp (2007): Enfermedad de Chagas
- Concepción Judith Puerta, Paula Ximena Pavia, Marleny Montilla, Carolina Flórez, Giomar Herrera, Juan Manuel Ospina, Fred Manrique, Rubén Santiago Nicholls, The first case of congenital Chagas’ disease analyzed by AP-PCR in Colombia , Biomedica: Vol. 29 No. 4 (2009)
- Luz Adriana Botero, Ana María Mejía, Omar Triana, Biological and genetic characterization of two Colombian clones of Trypanosoma cruzi groups I and II , Biomedica: Vol. 27 No. 1esp (2007): Enfermedad de Chagas
- Sandra Paola Santander, Adriana Cuéllar, María del Carmen Thomas, Fanny Guzmán, Alberto Gómez, Manuel Carlos López, Concepción Puerta, Expression of markers on dendritic cells from chronic chagasic patients stimulated with the KMP-11 protein and the K1 peptide from Trypanosoma cruzi , Biomedica: Vol. 27 No. 1esp (2007): Enfermedad de Chagas
- Rubén Santiago Nicholls, Zulma Milena Cucunubá, Angélica Knudson, Astrid Carolina Flórez, Marleny Montilla, Concepción Judith Puerta, Paula Ximena Pavía, Acute Chagas disease in Colombia: a rarely suspected disease. Report of 10 cases presented during the 2002-2005 period , Biomedica: Vol. 27 No. 1esp (2007): Enfermedad de Chagas
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























