Infection due to Aspergillus flavus and Rhizopus oryzae complex in a patient with diabetes mellitus
Abstract
Fungal sinusitis is a pathology that can occur in patients with diabetes mellitus and be associated with a hyperglycemic crisis. It is an aggressive entity with local complications that include involvement of the orbit or the central nervous system, and vascular involvement. Despite surgical and antifungal treatment, mortality raises up to 75%.
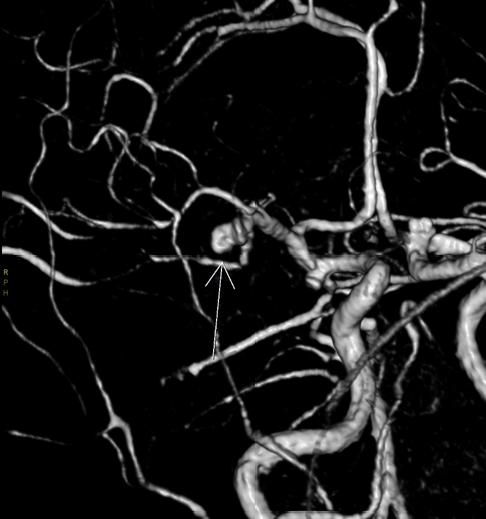
We report the case of a female patient with a diagnosis of diabetic ketoacidosis and signs of unilateral ophthalmoplegia, which led to the study with magnetic resonance imaging of the central nervous system, finding signs of sinusitis, meningitis, and cerebritis. Initial microbiological studies were negative, and biomarkers such as serum galactomannan and Cryptococcus antigen were also negative. After surgical management and the identification of Aspergillus flavus and Rhizopus spp. in sinus tissue, the patient received treatment with posaconazole and after two months of follow-up she presented clinical improvement. Dual fungal infection and infection by A. flavus are uncommon and clinically relevant entities, with no cases previously reported in our country, therefore this corresponds to a case of clinical interest.
Downloads
References
Trief D, Gray ST, Jakobiec FA, Durand ML, Fay A, Freitag SK, et al. Invasive fungal disease of the sinus and orbit: A comparison between mucormycosis and Aspergillus. Br J Ophthalmol. 2016;100:184-8. https://doi.org/10.1136/bjophthalmol-2015-306945
Casqueiro J, Casqueiro J, Alves C. Infections in patients with diabetes mellitus: A review of pathogenesis. Indian J Endocrinol Metab. 2012;16(Suppl.1):S27-36. https://doi.org/10.4103/2230-8210.94253
Borjian Boroujeni Z, Shamsaei S, Yarahmadi M, Getso MI, Salimi Khorashad A, Haghighi L, et al. Distribution of invasive fungal infections: Molecular epidemiology, etiology, clinical conditions, diagnosis, and risk factors: A 3-year experience with 490 patients under intensive care. Microb Pathog. 2020;104616. https://doi.org/10.1016/j.micpath.2020.104616
Jeong W, Keighley C, Wolfe R, Lee WL, Slavin MA, Kong DCM, et al. The epidemiology and clinical manifestations of mucormycosis: A systematic review and meta-analysis of case reports. Clin Microbiol Infect. 2019;25:26-3. https://doi.org/10.1016/j.cmi.2018.07.011
Saud B, Bajgain P, Paudel G, Shrestha V, Bajracharya D, Adhikari S, et al. Fungal infection among diabetic and nondiabetic individuals in Nepal. Interdiscip Perspect Infect Dis. 2020;2020:7949868. https://doi.org/10.1155/2020/7949868
Lao M, Li C, Li J, Chen D, Ding M, Gong Y. Opportunistic invasive fungal disease in patients with type 2 diabetes mellitus from Southern China: Clinical features and associated factors. J Diabetes Investig. 2020;11:731-44. https://doi.org/10.1111/jdi.13183
Adulkar NG, Radhakrishnan S, Vidhya N, Kim U. Invasive sino-orbital fungal infections in immunocompetent patients: A clinico-pathological study. Eye (Lond). 2019;33:988-94. https://doi.org/10.1038/s41433-019-0358-6
Deutsch PG, Whittaker J, Prasad S. Invasive and non-invasive fungal rhinosinusitis-a review and update of the evidence. Medicina (Kaunas). 2019;55. https://doi.org/0.3390/medicina55070319
Lagos A, Ferrada S, Muñoz T, Maul X, Finkelstein A, González C, et al. 10-year experience in patients operated for acute invasive fungal rhinosinusitis. Acta Otorrinolaringol Esp. 2020;71:303-8. https://doi.org/10.3390/medicina55070319
Cornely OA, Alastruey-Izquierdo A, Arenz D, Chen SCA, Dannaoui E, Hochhegger B, et al. Global guideline for the diagnosis and management of mucormycosis: An initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019;19:e405-21. https://doi.org/10.1016/S1473-3099(19)30312-3
Chakrabarti A, Denning DW, Ferguson BJ, Ponikau J, Buzina W, Kita H, et al. Fungal rhinosinusitis: A categorization and definitional schema addressing current controversies. Laryngoscope. 2009;119:1809-18. https://doi.org/10.1002/lary.20520
Choi YR, Kim JH, Min HS, Won JK, Kim HJ, Yoo RE, et al. Acute invasive fungal rhinosinusitis: MR imaging features and their impact on prognosis. Neuroradiology. 2018;60:715-23. https://doi.org/10.1007/s00234-018-2034-0
Reid G, Lynch JP 3rd, Fishbein MC, Clark NM. Mucormycosis. Semin Respir Crit Care Med. 2020;41:99-114. https://doi.org/10.1055/s-0039-3401992
Craig JR. Updates in management of acute invasive fungal rhinosinusitis. Curr Opin Otolaryngol Head Neck Surg. 2019;27:29-36. https://doi.org/10.1097/MOO.0000000000000507
Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, et al. Epidemiology and outcome of zygomycosis: A review of 929 reported cases. Clin Infect Dis. 2005;41:634-53. https://doi.org/10.1086/432579
Chakrabarti A, Das A, Mandal J, Shivaprakash MR, George VK, Tarai B, et al. The rising trend of invasive zygomycosis in patients with uncontrolled diabetes mellitus. Med Mycol. 2006;44:335-42. https://doi.org/10.1080/13693780500464930
Manesh A, Rupali P, Sullivan MO, Mohanraj P, Rupa V, George B, et al. Mucormycosis -A clinico epidemiological review of cases over 10 years. Mycoses. 2019;62:391-8. https://doi.org/10.1111/myc.12897
Gupta S, Goyal R, Kaore NM. Rhino-orbital-cerebral mucormycosis: Battle with the deadly enemy. Indian J Otolaryngol Head Neck Surg. 2020;72:104-11. https://doi.org/ 10.1007/s12070-019-01774-z
Cornely OA, Arikan-Akdagli S, Dannaoui E, Groll AH, Lagrou K, Chakrabarti A, et al. ESCMID and ECMM joint clinical guidelines for the diagnosis and management of mucormycosis 2013. Clin Microbiol Infect. 2014;20(Suppl.3):5-26. https://doi.org/10.1111/1469-0691.12371
Brunet K, Rammaert B. Mucormycosis treatment: Recommendations, latest advances, and perspectives. J Mycol Med. 2020;30:101007. https://doi.org/10.1016/j.mycmed.2020.101007
Krishnan S, Manavathu EK, Chandrasekar PH. Aspergillus flavus: An emerging nonfumigatus Aspergillus species of significance. Mycoses. 2009;52:206-22. https://doi.org/10.1111/j.1439-0507.2008.01642.x
Denning DW, Chakrabarti A. Pulmonary and sinus fungal diseases in nonimmunocompromised patients. Lancet Infect Dis. 2017;17:e357-66. https://doi.org/10.1016/S1473-3099(17)30309-2
GarcÍa-Giraldo AM, Mora BL, Loaiza-Castaño JM, Cedano JA, Rosso F. Invasive fungal infection by Aspergillus flavus in immunocompetent hosts: A case series and literature review. Med Mycol Case Rep. 2018;23:12-5. https://doi.org/10.1016/j.mmcr.2018.10.006
Singh AK, Gupta P, Verma N, Khare V, Ahamad A, Verma V, et al. Fungal rhinosinusitis: Microbiological and histopathological perspective. J Clin Diagn Res. 2017;11:DC10-2. https://doi.org/10.7860/JCDR/2017/25842.10167
Krishnan KU, Agatha D, Selvi R. Fungal rhinosinusitis: A clinicomycological perspective. Indian J Med Microbiol. 2015;33:120-4. https://doi.org/10.4103/0255-0857.148407
Morales-López S, Ceballos-Garzón A, Parra-Giraldo CM. Zygomycete fungi infection in Colombia: Literature review. Curr Fungal Infect Rep. 2018;12:149-54. https://doi.org/10.1007/s12281-018-0326-9
Allen LM, Fowler AM, Walker C, Derdeyn CP, Nguyen BV, Hasso AN, et al. Retrospective review of cerebral mycotic aneurysms in 26 patients: Focus on treatment in strongly immunocompromised patients with a brief literature review. AJNR Am J Neuroradiol. 2013;34:823-7. https://doi.org/10.3174/ajnr.A3302
Marzolf G, Sabou M, Lannes B, Cotton F, Meyronet D, Galanaud D, et al. Magnetic resonance imaging of cerebral aspergillosis: Imaging and pathological correlations. PLoS ONE. 2016;11:e0152475. https://doi.org/10.1371/journal.pone.0152475
Kannoth S, Thomas SV. Intracranial microbial aneurysm (infectious aneurysm): Current options for diagnosis and management. Neurocrit Care. 2009;11:120-9. https://doi.org/10.1007/s12028-009-9208-x
Ma Y, Li W, Ao R, Lan X, Li Y, Zhang J, et al. Central nervous system aspergillosis in immunocompetent patients: Case series and literature review. Medicine (Baltimore). 2020;99:e22911. https://doi.org/10.1097/MD.0000000000022911
Lionakis MS. Primary immunodeficiencies and invasive fungal infection: When to suspect and how to diagnose and manage. Curr Opin Infect Dis. 2019;32:531-7. https://doi.org/10.1097/QCO.0000000000000593
Some similar items:
- Ricardo Cardona, Ruth Helena Ramírez, Zulma Reina, Mauricio Fernando Escobar, Edison Morales, Allergy and intolerance to nonsteroidal antinflammatory drugs: successful desensitization in three cases , Biomedica: Vol. 29 No. 2 (2009)
Copyright (c) 2023 Biomedica

This work is licensed under a Creative Commons Attribution 4.0 International License.
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























