Pulmonary and central nervous system nocardiosis: Alcoholism as an immunocompromising factor
Abstract
Nocardiosis is a disease with worldwide distribution. It is usually found in tropical areas and mainly affects immunocompromised patients, however, there are also cases where its infection has been reported in immunocompetent patients. This pathology is caused by bacteria known as Nocardia spp., which are gram-positive microorganisms and environmental saprophytes, and although exposure to Nocardia spp. is almost universal, only a small fraction of exposed people develops the disease.
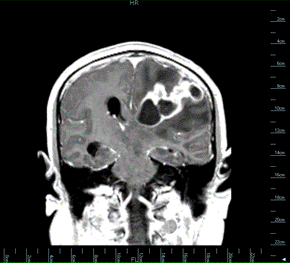
We present the case of a 47-year-old man, with no evidence of immunosuppression, from a rural area of Boyacá, who was admitted due to intense and intermittent headache accompanied by paresthesia and, finally, a decrease in consciousness. A brain magnetic resonance was performed and evidenced a fronto-temporo- occipital space-occupying lesion in the cortico-subcortical region with a compressive effect and displacement of the ventricular system cavities. It was suspected at first a neoplastic lesion or a brain abscess.
The lesion was surgically resected, and its culture showed Nocardia africana/nova. In later studies a possible primary pulmonary focus was evidenced. Alcoholism was the only risk factor documented. The patient completed 6 weeks of hospital antibiotic treatment with favorable clinical and radiological evolution and was discharged with a 1-year plan of outpatient antibiotic therapy. Although Nocardia spp. mainly affects immunocompromised patients, evidence shows that this microorganism can also be a threat to individuals without traditional immunosuppression risk factors.
Downloads
References
Conville PS, Brown-Elliott BA, Smith T, Zelazny AM. The complexities of nocardia taxonomy and identification. J Clin Microbiol. 2018;56:1-10. https://doi.org/10.1128/JCM.01419-17
Martínez-Barricarte R. Isolated nocardiosis, an unrecognized primary immunodeficiency? Front Immunol. 2020;11:1-17. https://doi.org/10.3389/fimmu.2020.590239
Ercibengoa M, Càmara J, Tubau F, García-Somoza D, Galar A, Martín-Rabadán P, et al. A multicentre analysis of Nocardia pneumonia in Spain: 2010-2016. Int J Infect Dis. 2020;90:161-6. https://doi.org/10.1016/j.ijid.2019.10.032
Mehta HH, Shamoo Y. Pathogenic nocardia: A diverse genus of emerging pathogens or just poorly recognized? PLoS Pathog. 2020;16:1-7. https://doi.org/10.1371/journal.ppat.1008280
Lederman ER, Crum NF. A case series and focused review of nocardiosis: Clinical and microbiologic aspects. Medicine. 2004;83:300-13. https://doi.org/10.1097/01.md.0000141100.30871.39
Ambrosioni J, Lew D, Garbino J. Nocardiosis: Updated clinical review and experience at a tertiary center. Infection. 2010;38:89-97. https://doi.org/10.1007/s15010-009-9193-9
Hamdi AM, Fida M, Deml SM, Abu Saleh OM, Wengenack NL. Retrospective analysis of antimicrobial susceptibility profiles of nocardia species from a tertiary hospital and reference laboratory, 2011 to 2017. Antimicrob Agents Chemother. 2020;64:1-7. https://doi.org/10.1128/AAC.01868-19
Huang L, Sun L, Yan Y. Characteristics of nocardiosis patients with different immune status from a Chinese tertiary general hospital during 8-year period: A STROBE-compliment observational study. Medicine. 2019;98:e17913. https://doi.org/10.1097/MD.0000000000017913
Hauser N, Luethy PM, Rapaka RR. An immunocompromised woman with a brain lesion. Am J Med. 2020;133:e516-7. https://doi.org/10.1016/j.amjmed.2020.02.021
Trujillo DE, Ortiz S, Pérez O, Cortés CA, Carrillo JA. Abscesos cerebrales por Nocardia spp. en una paciente inmunocompetente. Biomédica. 2020;40:27-33. https://doi.org/10.7705/biomedica.4925
Martínez-Tomás R, Menéndez-Villanueva R, Reyes-Calzada S, Santos-Durantez M, Vallés-Tarazona JM, Modesto -Alapont M, et al. Pulmonary nocardiosis: Risk factors and outcomes. Respirology. 2007;12:394-400. https://doi.org/10.1111/j.1440-1843.2007.01078.x
Szabo G, Saha B. Alcohol’s effect on host defense. Alcohol Res. 2015;37:159-70.
Kaphalla L, Calhoun W. Alcoholic lung injury: metabolic, biochemical, and immunological aspects. Toxicol Lett. 2013;222:171-9. https://doi.org/10.1016/j.toxlet.2013.07.016
Liang Y, Yeligar SM, Brown LAS. Chronic-alcohol-abuse-induced oxidative stress in the development of acute respiratory distress syndrome. Sci World J. 2012;2012:740308. https://doi.org/10.1100/2012/740308
Ministerio de Justicia y del Derecho - Observatorio Nacional de Drogas de Colombia. Estudio Nacional de Consumo de Sustancias Psicoactivas. Colombia, 2019. Fecha de consulta: 2 de abril de 2022. Disponible en: https://www.odc.gov.co/Portals/1/publicaciones/pdf/estudio Nacional de consumo 2019.pdf
Bautista H, Lizarazo J. Nocardiosis diseminada en una paciente VIH negativa. A propósito de un caso de difícil tratamiento. Acta Neurológica Colombiana. 2015;31:267-75. https://doi.org/10.22379/2422402240
Duque AIA, Salas PAO, Oviedo JMP, Mora A, Ruales F. Meningoencefalitis por Nocardia spp.: reporte de un caso y revisión de la literatura. Infectio. 2014;18:109-15. https://doi.org/10.1016/j.infect.2014.02.005
Cercenado E, Marín M, Sánchez M, Cuevas O, Martínez J, Bouza E. In vitro activities of tigecycline and eight other antimicrobials against different Nocardia species identified by molecular methods. Antimicrob Agents Chemother. 2007;51:1102-4. https://doi.org/10.1128/AAC.01102-06
Zhu JW, Zhou H, Jia WQ, You J, Xu RX. A clinical case report of brain abscess caused by Nocardia brasiliensis in a non-immunocompromised patient and a relevant literature review. BMC Infect Dis. 2020;20:1-8. https://doi.org/10.1186/s12879-020-05052-0
Some similar items:
- Danilo E. Trujillo, Stephanie Ortiz , Oscar Pérez, Camilo A. Cortés, Jorge A. Carrillo, Multiple brain abscesses due to Nocardia spp. in an immunocompetent patient , Biomedica: Vol. 40 No. 1 (2020)
- Fabio Samir Vargas-Cely, Andrés F. Zea-Vera, Danilo Eduardo Trujillo-González, Multiple brain abscesses due to Nocardia spp. in an immunocompetent patient , Biomedica: Vol. 40 No. 2 (2020)
Copyright (c) 2023 Biomedica

This work is licensed under a Creative Commons Attribution 4.0 International License.
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























