Oral mucormycosis associated with COVID-19 and diabetes mellitus: Case report and literature review
Abstract
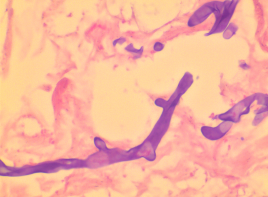
Mucormycosis is an invasive opportunistic fungal infection with high mortality, mainly detected in people with COVID-19, especially those with underlying diseases such as diabetes mellitus. Mucormycosis prevalence is 0.005 to 1.7 cases per million inhabitants, and it has been increasing in countries like India and Pakistan. This mycosis can affect different organs, and clinical manifestations reflect the transmission mechanism. Frequent forms are rhino-orbital-cerebral and pulmonary. This disease should be suspected in patients with necrotic injuries on mucous membranes or skin.
We present a case of a patient with diabetes mellitus and diagnosed with oral mucormycosis associated with COVID-19.
Downloads
References
Quiroz N, Villanueva JP, Lozano EA. Mucormicosis. Rev Asoc Colomb Dermatol Cir Dermatol. 2019;25:284-93. https://doi.org/10.29176/2590843X.302
Fernández NB. Las infecciones fúngicas en la pandemia de COVID-19, el caso de la mucormicosis. Rev Argent Microbiol. 2021;53:181-2. https://doi.org/10.1016/j.ram.2021.09.001
Muñoz-Estrada VF, Ylé-Arámburo EL, Piña-Lugo F. Mucormicosis: “el hongo negro” asociado a COVID-19. Rev Med UAS. 2021;11:386.
Ponce-Rosas L, Gonzales-Zamora J, Diaz-Reyes N, Alarco-Cadillo O, AlaveRosas J. Rhinoorbital-cerebral mucormycosis in a post-covid-19 patient from Perú. Case Rep Infect Dis. 2022;2022:2537186. https://doi.org/10.1155/2022/2537186
Instituto Nacional de Salud. Lineamientos mucormicosis asociada con la COVID19 (CAM). Colombia. 2021. Fecha de consulta: 6 de octubre de 2023. Disponible en: https://www.ins.gov.co/BibliotecaDigital/comunicado-lineamiento-mucormicosis-asociada-con-la-covid-19-cam.pdf
Instituto Nacional de Salud. Mucormicosis: generalidades sobre una micosis en tiempos de la COVID-19. Colombia. 2021. Fecha de consulta: 6 de octubre de 2023. Disponible en: https://www.ins.gov.co/BibliotecaDigital/mucormicosis-generalidades-sobre-una-micosis-entiempos-de-la-covid-19.pdf
Instituto Nacional de Salud. Vigilancia por laboratorio de mucormicosis asociada con la COVID-19. Colombia. 2021. Fecha de consulta: 6 de octubre de 2023. Disponible en: https://www.ins.gov.co/BibliotecaDigital/vigilancia-por-laboratorio-de-mucormicosisasociada-a-la-covid-19-cam-colombia-2021.pdf
Palou EY, Ramos MA, Cherenfant E, Duarte A, Fuentes-Barahona IC, Zambrano LI, et al. COVID-19 Associated rhino-orbital mucormycosis complicated by gangrenous and bone necrosis - A case report from Honduras. Vaccines (Basel). 2021;9:826. https://doi.org/10.3390/vaccines9080826
Yadav S, Sharma A, Kothari N, Bhatia PK, Goyal S, Goyal A. Mucormycosis: A case series of patients admitted in non-COVID-19 intensive care unit of a tertiary care center during the second wave. Indian J Crit Care Med. 2021;25:1193-6. https://doi.org/10.5005/jp-journals-10071-23986
Singh AK, Singh R, Joshi SR, Misra A. Mucormycosis in COVID-19: A systematic review of cases reported worldwide and in India. Diabetes Metab Syndr. 2021;15:102146. https://doi.org/10.1016/j.dsx.2021.05.019
Prakash H, Ghosh AK, Rudramurthy SM, Singh P, Xess I, Savio J, et al. A prospective multicenter study on mucormycosis in India: Epidemiology, diagnosis, and treatment. Med Mycol. 2019;57:395-02. https://doi.org/10.1093/mmy/myy060
Kulkarni MD, Gulati S, Gupta S, Sabharwal R, Rajguru JP, Baneerjee A. Oral Mucormycosis: An inevitable complication of COVID-19. J Family Med Prim Care. 2022;11:1672-6. https://doi.org/10.4103/jfmpc.jfmpc_1599_21
Rodríguez-Morales AJ, Mamani-García CS, Núñez-Lupaca JN, León-Figueroa DA, Olarte-Durand M, Yrene-Cubas RA, et al. COVID-19 and mucormycosis in Latin America - An emerging concern. Travel Med Infect Dis. 2021;44:102156. https://doi.org/10.1016/j.tmaid.2021.102156
Edeas M, Saleh J, Peyssonnaux C. Iron: Innocent bystander or vicious culprit in COVID-19 pathogenesis? Int J Infect Dis. 2020;97:303-5. https://doi.org/10.1016/j.ijid.2020.05.110
Perricone C, Bartoloni E, Bursi R, Cafaro G, Guidelli GM, Shoenfeld Y, et al. COVID-19 as part of the hyperferritinemic syndromes: The role of iron depletion therapy. Immunol Res. 2020;68:213-24. https://doi.org/10.1007/s12026-020-09145-5
Garg D, Muthu V, Sehgal IS, Ramachandran R, Kaur H, Bhalla A, et al. Coronavirus disease (COVID-19) associated mucormycosis (CAM): Case report and systematic review of literature. Mycopathologia. 2021;186:289-98. https://doi.org/10.1007/s11046-021-00528-2
John TM, Jacob CN, Kontoyiannis DP. When uncontrolled diabetes mellitus and severe COVID-19 converge: The perfect storm for mucormycosis. J Fungi (Basel). 2021;7:298. https://doi.org/10.3390/jof7040298
Castrejón-Pérez AD, Welsh EC, Miranda I, Ocampo-Candiani J, Welsh O. Cutaneous mucormycosis. An Bras Dermatol. 2017;92:304-11. https://doi.org/10.1590/abd1806-4841.20176614
Sahota R, Gambhir R, Anand S, Dixit A. Rhinocerebral mucormycosis: Report of a rare case. Ethiop J Health Sci. 2017;27:85-90. https://doi.org/10.4314/ejhs.v27i1.11
Farmakiotis D, Kontoyiannis DP. Mucormycoses. Infect Dis Clin North Am. 2016;30:143-63. https://doi.org/10.1016/j.idc.2015.10.011
Cornely OA, Alastruey-Izquierdo A, Arenz D, Chen SCA, Dannaoui E, Hochhegger B, et al. Mucormycosis ECMM MSG Global Guideline Writing Group. Global guideline for the diagnosis and management of mucormycosis: An initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019;19:405-21. https://doi.org/10.1016/S1473-3099(19)30312-3
Copyright (c) 2024 Biomedica

This work is licensed under a Creative Commons Attribution 4.0 International License.
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























