The conventional diagnosis challenge: Real-time PCR and nested PCR correlation with the scoring system for individuals at high-risk of Pneumocystis jirovecii pneumonia
Abstract
Introduction. Pneumocystis jirovecii is an opportunistic fungus that affects mainly people living with HIV (CD4 cell count lower than 200 cells/ml) and other immunosuppressed patients. Since P. jirovecii does not grow on routine mycological media, diagnosis of P. jirovecii pneumonia relies on indirect evidence of its presence in respiratory samples.
Objectives. To associate the results of direct immunofluorescence and two molecular methods with a score to predict P. jirovecii pneumonia in patients with AIDS.
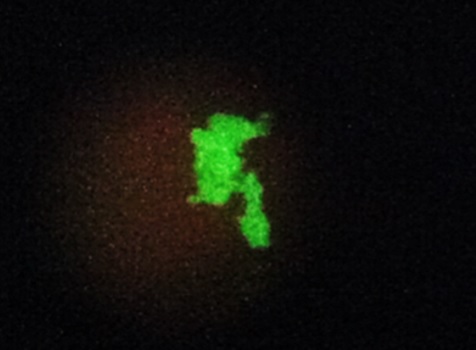
Materials and methods. A prospective study was conducted with 40 patients. A respiratory sample collected before treatment was subjected to direct immunofluorescence using the Merifluor kit, to nested PCR targeting the mitochondrial large subunit ribosomal RNA, and to the VIASURE real-time PCR kit.
Results. These three techniques revealed P. jirovecii in 6, 12, and 15 samples, respectively. All positive samples by direct immunofluorescence were positive by nested PCR, and all positive samples by nested PCR amplified by real-time PCR. There was a statistically significant association between the P. jirovecii pneumonia score and the molecular methods. Two patients were early diagnosed and responded well to treatment.
Conclusion. Molecular methods, especially real-time PCR, are recommended for early diagnosis of P. jirovecii pneumonia in AIDS patients.
Downloads
References
Hoving JC, Brown GD, Gómez BL, Govender NP, Limper AH, May RC, et al. AIDS-related mycoses: Updated progress and future priorities. Trends Microbiol. 2020;28:425-8. https://doi.org/10.1016/j.tim.2020.01.009
Limper AH, Adenis A, Le T, Harrison TS. Fungal infections in HIV/AIDS. Lancet Infect Dis. 2017;17:e334-43. https://doi.org/10.1016/S1473-3099(17)30303-1
Meléndez-Rivera JG, Ciofoaia GA. Pneumocystis jirovecii prophylaxis. Treasure Island: StatPearls; 2021.
Thomas CF Jr., Limper AH. Pneumocystis pneumonia. N Engl J Med. 2004;350:2487-98. https://doi.org/10.1056/NEJMra032588
Peters SE, Wakefield AE, Sinclair K, Millard PR, Hopkin JM. A search for Pneumocystis carinii in post-mortem lungs by DNA amplification. J Pathol. 1992;166:195-8. https://doi.org/10.1002/path.1711660217
Truong J, Ashurst JV. Pneumocystis jirovecii pneumonia. Treasure Island: StatPearls; 2021.
Phair J, Muñoz A, Detels R, Kaslow R, Rinaldo C, Saah A. The risk of Pneumocystis carinii pneumonia among men infected with human immunodeficiency virus type 1. Multicenter AIDS Cohort Study Group. N Engl J Med. 1990;322:161-5. https://doi.org/10.1056/NEJM199001183220304
White PL, Price JS, Backx M. Pneumocystis jirovecii pneumonia: epidemiology, clinical manifestation and diagnosis. Curr Fungal Infect R. 2019;13:260‑73. https://doi.org/10.1007/s12281-019-00349-3
Schildgen V, Mai S, Khalfaoui S, Lusebrink J, Pieper M, Tillmann RL, et al. Pneumocystis jirovecii can be productively cultured in differentiated CuFi-8 airway cells. mBio. 2014;5:e01186-14. https://doi.org/10.1128/mBio.01186-14
Carmona EM, Limper AH. Update on the diagnosis and treatment of Pneumocystis pneumonia. Ther Adv Respir Dis. 2011;5:41-59. https://doi.org/10.1177/1753465810380102
Guarner J, Brandt ME. Histopathologic diagnosis of fungal infections in the 21st century. Clin Microbiol Rev. 2011;24:247-80. https://doi.org/10.1128/CMR.00053-10
Gingerich AD, Norris KA, Mousa JJ. Pneumocystis pneumonia: immunity, vaccines, and treatments. Pathogens. 2021;10. https://doi.org/10.3390/pathogens10020236
Daly K, Koch J, Respaldiza N, de la Horra C, Montes-Cano MA, Medrano FJ, et al. Geographical variation in serological responses to recombinant Pneumocystis jirovecii major surface glycoprotein antigens. Clin Microbiol Infect. 2009;15:937-42. https://doi.org/10.1111/j.1469-0691.2009.02716.x
Sabbagh W, Darwich NS. Pneumocystis jirovecii pneumonia and newly diagnosed human immunodeficiency virus (AIDS) in a 63-year-old woman. Am J Case Rep. 2018;19:927-31. https://doi.org/10.12659/AJCR.909612
Langevin B, Saleh M. Radiological presentation of Pneumocystis jirovecii pneumonia mimicking bacterial pneumonia. BMJ Case Rep. 2016;2016:bcr2016215207. https://doi.org/10.1136/bcr-2016-215207
Waks AG, Tolaney SM, Galar A, Arnaout A, Porter JB, Marty FM, et al. Pneumocystis jirovecii pneumonia (PCP) in patients receiving neoadjuvant and adjuvant anthracyclinebased chemotherapy for breast cancer: incidence and risk factors. Breast Cancer Res Treat. 2015;154:359-67. https://doi.org/10.1007/s10549-015-3573-2
Pandey S, Ghosh S, Halder P, Pal D, Modak DC, Guha SK. Pulmonary tuberculosis and Pneumocystis jirovecii concurrent pneumonia in HIV infected patients at a resource limited setting in Eastern India: A case series. Indian J Tuberc. 2020;67:378-82. https://doi.org/10.1016/j.ijtb.2019.08.003
Wahab A, Chaudhary S, Khan M, Smith SJ. Concurrent Pneumocystis jirovecii and pulmonary histoplasmosis in an undiagnosed HIV patient. BMJ Case Rep. 2018;2018:bcr2017223422. https://doi.org/10.1136/bcr-2017-223422
Obmann VC, Bickel F, Hosek N, Ebner L, Huber AT, Damonti L, et al. Radiological CT patterns and distribution of invasive pulmonary Aspergillus, non-Aspergillus, Cryptococcus and Pneumocystis jirovecii mold infections - A multicenter study. Rofo. 2021;193:1304-14. https://doi.org/10.1055/a-1482-8336
Nambu A, Ozawa K, Kobayashi N, Tago M. Imaging of community-acquired pneumonia: Roles of imaging examinations, imaging diagnosis of specific pathogens and discrimination from noninfectious diseases. World J Radiol. 2014;6:779‑93. https://doi.org/10.4329/wjr.v6.i10.779
Szydlowicz M, Matos O. Pneumocystis pneumonia in the COVID-19 pandemic era: Similarities and challenges. Trends Parasitol. 2021;37:859-62. https://doi.org/10.1016/j.pt.2021.07.010
Muñoz C, Zuluaga A, Restrepo A, Tobón A, Cano LE, González A. Molecular diagnosis and detection of Pneumocystis jirovecii DHPS and DHFR genotypes in respiratory specimens from Colombian patients. Diagn Microbiol Infect Dis. 2012;72:204-13. https://doi.org/10.1016/j.diagmicrobio.2011.11.015
Chotiprasitsakul D, Pewloungsawat P, Setthaudom C, Santanirand P, Pornsuriyasak P. Performance of real-time PCR and immunofluorescence assay for diagnosis of Pneumocystis pneumonia in real-world clinical practice. PLoS ONE. 2020;15:e0244023. https://doi.org/10.1371/journal.pone.0244023
Bateman M, Oladele R, Kolls JK. Diagnosing Pneumocystis jirovecii pneumonia: A review of current methods and novel approaches. Med Mycol. 2020;58:1015-28. https://doi.org/10.1093/mmy/myaa024
Perret T, Kritikos A, Hauser PM, Guiver M, Coste AT, Jaton K, et al. Ability of quantitative PCR to discriminate Pneumocystis jirovecii pneumonia from colonization. J Med Microbiol. 2020;69:705-11. https://doi.org/10.1099/jmm.0.001190
Gupta R, Mirdha BR, Guleria R, Kumar L, Samantaray JC, Agarwal SK, et al. Diagnostic significance of nested polymerase chain reaction for sensitive detection of Pneumocystis jirovecii in respiratory clinical specimens. Diagn Microbiol Infect Dis. 2009;64:381-8. https://doi.org/10.1016/j.diagmicrobio.2009.04.008
Robert-Gangneux F, Belaz S, Revest M, Tattevin P, Jouneau S, Decaux O, et al. Diagnosis of Pneumocystis jirovecii pneumonia in immunocompromised patients by real-time PCR: A 4-year prospective study. J Clin Microbiol. 2014;52:3370-6. https://doi.org/10.1128/JCM.01480-14
Smith D, Forbes A, Gazzard B. A simple scoring system to diagnose Pneumocystis carinii pneumonia in high-risk individuals. AIDS. 1992;6:337-8.
Nascimento CR, Lima MA, de Andrada-Serpa MJ, Espindola O, Leite AC, Echevarria-Lima J. Monocytes from HTLV-1-infected patients are unable to fully mature into dendritic cells. Blood. 2011;117:489-99. https://doi.org/10.1182/blood-2010-03-272690
Wakefield AE, Pixley FJ, Banerji S, Sinclair K, Miller RF, Moxon ER, et al. Amplification of mitochondrial ribosomal RNA sequences from Pneumocystis carinii DNA of rat and human origin. Mol Biochem Parasitol. 1990;43:69-76. https://doi.org/10.1016/0166-6851(90)90131-5
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159-74.
Elvin K, Linder E. Application and staining patterns of commercial anti-Pneumocystis carinii monoclonal antibodies. J Clin Microbiol. 1993;31:2222-4. https://doi.org/10.1128/jcm.31.8.2222-2224.1993
El Hodaky ES, Ouda N, Meshref M, El Bassiouny S, El Masry M, Gamal El Din H. Comparison of different methods to diagnose Pneumocystis jirovecii pneumonia in children with haematological malignancies. Egypt J Med Microbiol. 2008;17:151-9.
Robberts FJ, Liebowitz LD, Chalkley LJ. Polymerase chain reaction detection of Pneumocystis jirovecii: Evaluation of 9 assays. Diagn Microbiol Infect Dis. 2007;58:385-92. https://doi.org/10.1016/j.diagmicrobio.2007.02.014
Beard CB, Carter JL, Keely SP, Huang L, Pieniazek NJ, Moura IN, et al. Genetic variation in Pneumocystis carinii isolates from different geographic regions: implications for transmission. Emerg Infect Dis. 2000;6:265-72. https://doi.org/10.3201/eid0603.000306
Sing A, Roggenkamp A, Autenrieth IB, Heesemann J. Pneumocystis carinii carriage in immunocompetent patients with primary pulmonary disorders as detected by single or nested PCR. J Clin Microbiol. 1999;37:3409-10. https://doi.org/10.1128/JCM.37.10.3409-3410.1999
Tang X, Bartlett MS, Smith JW, Lu JJ, Lee CH. Determination of copy number of rRNA genes in Pneumocystis carinii f. sp. hominis. J Clin Microbiol. 1998;36:2491-4. https://doi.org/10.1128/JCM.36.9.2491-2494.1998
Some similar items:
- Anna Carolina Ratto-Tespestini, Paula Juliana Pérez-Chaparro, Giuseppe Alexandre Romito, Luciene Cristina Figueiredo, Marcelo Faveri, Hilana Paula Carillo, Priscila Larcher, Magda Feres, Comparison of independent and dependent culture methods for the detection of transient bacteremia in diabetic subjects with chronic periodontitis , Biomedica: Vol. 36 No. 1 (2016)
- Rubén E. Varela-M, Jinney Stefany Arias, Luz Elena Velásquez, Standardization of a multiplex real-time PCR test for the identification of Angiostrongylus cantonensis, A. costaricensis and A. vasorum , Biomedica: Vol. 38 No. 1 (2018)
- Lina M. Osorio-Cock, Sandra Catalina Jaramillo-Pulgarín, Alba P. Ferrín-Bastidas, Diana Y. Molina-Colorado, Óscar M. Gómez-Guzmán, Alejandra Zuluaga, Juan G. McEwen-Ochoa, Martha E. Urán-Jiménez, María del Pilar Jiménez-Alzate, Pseudoepitheliomatous hyperplasia: Squamous cell carcinoma versus oral paracoccidioidomycosis, a case from a dermatological perspective , Biomedica: Vol. 43 No. Sp. 1 (2023): Agosto, Micología médica
Copyright (c) 2023 Biomedica

This work is licensed under a Creative Commons Attribution 4.0 International License.
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























