Vagino-rectal colonization prevalence by Streptococcus agalactiae and its susceptibility profile in pregnant women attending a third-level hospital
Abstract
Introduction: Streptococcus agalactiae is the main etiological agent causing invasive infection of the newborn with symptoms that may be associated with septicemia, pneumonia or meningitis and prevalences up to 50% worldwide where there is an increase in antibiotic resistance.
Objective: To estimate the prevalence of vagino-rectal colonization by S. agalactiae and its sensitivity profile in pregnant women attending a third-level hospital.
Materials and methods: One hundred and twenty one pregnant women were sampled by vaginal and rectal swabs. The cultures were carried out following the methodology recommended by the CDC, and chromID Strepto B agar was added. The suggestive colonies were identified biochemically and the sensitivity profiles according to CLSI were determined. As control, S. pneumoniae ATCC 49619 and S. agalactiae ATCC 12403 were used.
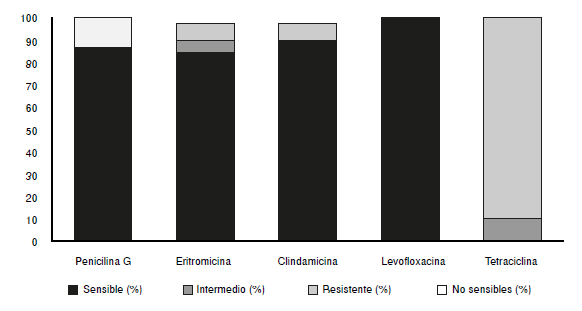
Results: Pregnant colonization prevalence by S. agalactiae was 20.66%, with a total of 40 isolates of which 12.5% were non-sensitivity to penicillin. Sensitivity to levofloxacin, clindamycin and erythromycin was 100%, 92.5% y 87.5%, respectively, with the phenotypes iMLSB (3/40) and M (2/40). No sensitivity to tetracycline was found.
Conclusions: The prevalence of vagino-rectal colonization by S. agalactiae in the study population was 20.66%, obtaining isolates not sensitive to penicillin and resistance to macrolides and lincosamidas by the Kirby-Bauer technique, so the importance of carrying out active active in pregnant women colonized by Streptococcus agalactiae and to perform constant epidemiological surveillance to detect changes in the sensitivity profiles of the isolates.
Downloads
References
Ceballos C, Loaíza N, Romero J, Ospina M, Vásquez EM. Caracterización de las gestantes tamizadas para Streptococcus agalactiae y su relación con sepsis neonatal temprana, en la Clínica del Prado de Medellín (Colombia), año 2010. Infectio. 2014;18:66-71. https://doi.org/10.1016/j.infect.2013.12.002
Duque CM, Gómez B, Uribe OI, Gutiérrez M, Ruiz E, Leudo GA, et al. Comparación de métodos para la recuperación y determinación de la prevalencia de Streptococcus agalactiae en mujeres gestantes de Medellín. Infectio. 2010;14:105-11. https://doi.org/10.1016/S0123-9392(10)70098-9
García DA, Mojica ME, Méndez IA, Pachón DP, Prieto AC, Santamaría EV, et al. Prevalencia del Streptococcus agalactiae en maternas usuarias del Hospital Militar Central, Bogotá (Colombia) año 2010. Rev Colomb Obstet Ginecol. 2011;62:302-7. https://doi.org/10.18597/issn.0034-7434
Verani JR, McGee L, Schrag SJ. Prevention of perinatal group B streptococcal Disease Revised Guidelines from CDC, 2010. MMWR Morb Mortal Wkly Rep. 2010;59:1-32.
Restrepo N, Alarcón C, Reveiz L, Morales O, Martínez O, Isaza M, et al. Prevalencia de la colonización vaginal y rectovaginal por estreptococo del grupo B en gestantes usuarias de la Clínica Universitaria Colombia, Bogotá, Colombia. Revista Médica Sanitas. 2009;12:8-15.
Alós JI, Domingo A, Arribas L, Cabero L, Cueto M, López J, et al. Prevención de la infección perinatal por estreptococo del grupo B. Recomendaciones españolas. Actualización 2012. Documento de consenso SEIMC/SEGO/SEN/SEQ/ SEMFYC. Enferm Infecc Microbiol Clin. 2013;31:159-72. https://doi.org/10.1016/j.eimc.2012.03.013
Restrepo A, Serna L, Vanegas C, Sarria C, Durango H, Zapata C, et al. Prevalencia de Streptococcus agalactiae en gestantes con factores de riesgo y sus recién nacidos. Hospital Universitario San Vicente de Paúl. 2002. Infectio. 2003;7:147-52.
Valdés E, Pastene C, Morales A, Gutiérrez B, Canales A, Martínez P, et al. Prevalencia de colonización por Streptococcus agalactiae (grupo B) durante el embarazo pesquisado en medio de cultivo selectivo. Rev Chil Obstet Ginecol. 2004;69:132-5. https://doi.org/10.4067/S0717-75262004000200008
Rojas JL, Pérez MP, Otálora EP. Prevalencia del Streptococcus B en el tracto genital inferior en embarazadas entre 35 y 37 semanas. Hospital San José. Repertorio de Medicina y Cirugía. 2010;19:141-6.
Amaya JP, Bello AM, Mendivil C, Correa O, Reyes N. Prevalencia de colonización vaginal y rectal por Streptococcus agalactiae en gestantes con trabajo de parto pretérmino en clínica maternidad Rafael calvo entre agosto 2011 y enero 2012. Revista de Ciencias Biomédicas. 2013;4:20-30.
Crespo MP, Henao EA, Espitia LM, Herrera MH. Colonización por Streptococcus agalactiae en mujeres gestantes de los centros de atención de la ESE Norte en Cali. Ciencia y Salud. 2012;1:23-31.
Beitune P, Duarte G, Leite CM. Colonization by Streptococcus agalactiae during pregnancy: Maternal and perinatal prognosis. Braz J Infect Dis. 2005;9:276-82. https://doi.org/10.1590/S1413-86702005000400002
Winn H. Group B Streptococcus infection in pregnancy. Clin Perinatol. 2007;34:387-92. https://doi.org/10.1016/j.clp.2007.03.012
Schrag SJ, Zell ER, Lynfield R, Roome A, Arnold KE, Craig AS, et al. A population-based comparison of strategies to prevent early-onset group B streptococcal disease in neonates. N Engl J Med. 2002;347:233-9. https://doi.org/10.1056/NEJMoa020205
Müller-Vranjes A, Puntarić D, Curzik D, Sijanović S, Topolovec Z, Kasac Z, et al. Prevalence and significance of vaginal group B streptococcus colonization in pregnant women from Osijek, Croatia. Coll Antropol. 2011;35:21-6.
Busetti M, D’Agaro P, Campello C. Group B streptococcus prevalence in pregnant women from North-Eastern Italy: Advantages of a screening strategy based on direct plating plus broth enrichment. J Clin Pathol. 2007;60:1140-3. https://doi.org/10.1136/jcp.2006.043489
Joachim A, Matee MI, Massawe FA, Lyamuya EF. Maternal and neonatal colonisation of group B streptococcus at Muhimbili National Hospital in Dar es Salaam, Tanzania: Prevalence, risk factors and antimicrobial resistance. BMC Public Health. 2009;9:437. https://doi.org/10.1186/1471-2458-9-437
Rausch A, Gross A, Droz S, Bodmer T, Surbek D. Group B Streptococcus colonization in pregnancy: Prevalence and prevention strategies of neonatal sepsis. J Perinat Med. 2009;37:124-9. https://doi.org/10.1515/JPM.2009.020
Nomura ML, Passini R, Moraes U, Calil R. Group B streptococcus maternal and neonatal colonization in preterm rupture of membranes and preterm labor. Rev Bras Ginecol Obstet. 2009;31:397-403. https://doi.org/10.1590/S0100-72032009000800005
Reyna J, Ortiz FJ, Arredondo JL, Beltrán M. Asociación entre la colonización materna de Streptococcus del grupo B serotipo III y la rotura prematura de membranas. Clin Invest Ginecol Obstet. 2006;33:140-5.
Abarzúa F, Argomedo C, Meissner A, Díaz T, Garrido P, Fariña S, et al. Prevalencia de portación vaginal-anal de Streptococcus agalactiae en el tercer trimestre de gestación y susceptibilidad a macrólidos y lincosamidas, en mujeres embarazadas de Clínica Alemana Temuco, Chile. Rev Chilena Infectol. 2014;31:305-8.
https://doi.org/10.4067/S0716-10182014000300009
Laufer J, Scasso S, Sosa C, Rodriguez-Cuns G, Justo A, Pons J. Group B streptococcus colonization among pregnant women in Uruguay. Int J Gynaecol Obstet. 2009;104:242-3. https://doi.org/10.1016/j.ijgo.2008.10.020
Larcher JS, Capellino F, Giusto R, Travella C, Gómez F, Kreiker G, et al. Colonización por estreptococo beta hemolítico del grupo B durante el embarazo y prevención de enfermedad neonatal. Medicina (Buenos Aires). 2005;65:201-6.
Marconi C, Rocchetti TT, Rall VL, Carvalho LR, Borges VT, Silva MG. Detection of Streptococcus agalactiae colonization in pregnant women by using combined swab cultures: Cross-sectional prevalence study. Sao Paulo Med J. 2010;128:60-2. https://doi.org/10.1590/S1516-31802010000200003
Costa A, Lamy F, Da Costa MB, Oliveira LM, Carvalho Z, Lima K. Prevalence of colonization by group B Streptococcus in pregnant women from a public maternity of Northwest region of Brazil. Rev Bras Ginecol Obstet. 2008;30:274-80. https://doi.org/10.1590/S0100-72032008000600002
Zusman A, Baltimore R, Fonseca S. Prevalence of maternal group B Streptococcal colonization and related risk factors in a Brazilian population. Braz J Infect Dis. 2006;10:242-6. https://doi.org/10.1590/S1413-86702006000400005
Tamariz JH, Obregón M, Jara JC, Díaz J, Cortez J, Guerra H. Vaginal and anorectal colonization by Streptococcus agalactiae among pregnant patients from Cayetano Heredia and Arzobispo Loayza Hospitals. Rev Medica Hered. 2004;15:144-50.
Díaz de R, Nieves B, Vegas L. Rectovaginal colonization by group B streptococcus in pregnant women with gynecobstetrics complications. Revista de la Sociedad Venezolana de Microbiología. 2002;22:12-17.
Amesty JG, Lares A, Sandrea L, Piña-Reyes E, Rojas P, Salas A, et al. Colonización de Streptococcus beta hemolítico del grupo B en gestantes en trabajo de parto y sus neonatos. Acta Cient Soc Venez Bioanalistas Esp. 2007;10:27-32.
Bosch-Mestres J, Martín-Fernández RM, Jiménez MT. Estudio comparativo de tres medios de cultivo para detectar la colonización por estreptococo del grupo B en la mujer embarazada. Enferm Infecc Microbiol Clin. 2003;21:346-9. https://doi.org/10.1016/S0213-005X(03)72961-9
Kimura K. Series of studies concerning group B streptococci with reduced penicillin susceptibility (PRGBS). Nihon Saikingaku Zasshi. 2014;69:547-55. https://doi.org/10.3412/jsb.69.547
Kimura K, Suzuki S, Wachino J, Kurokawa H, Yamane K, Shibata N, et al. First molecular characterization of group B streptococci with reduced penicillin susceptibility. Antimicrob Agents Chemother. 2008;52:2890-7. https://doi.org/10.1128/aac.00185-08
Betriu C, Gómez M, Sánchez A, Cruceyra A, Romero J, Picazo JJ. Antibiotic resistance and penicillin tolerance in clinical isolates of group B streptococci. Antimicrob Agents Chemother. 1994;38:2183-6. https://doi.org/10.1128/AAC.38.9.2183
Gizachew M, Tiruneh M, Moges F, Adefris M, Tigabu Z, Tessema B. Newborn colonization and antibiotic susceptibility patterns of Streptococcus agalactiae at the University of Gondar Referral Hospital, Northwest Ethiopia. BMC Pediatr. 2018;18:378. https://doi.org/10.1186/s12887-018-1350-1
Tamariz JH, Cruz J, Atencia Al, Figueroa J, Horna G, Guerra H. Resistencia a clindamicina inducida por eritromicina en Staphylococcus aureus aislados de tres hospitales de Lima, Perú. Acta Médica Peruana. 2009;26:12-6.
Leclercq R. Mechanisms of resistance to macrolides and lincosamides: Nature of the resistance elements and their clinical implications. Clin Infect Dis. 2002;34:482-92. https://doi.org/10.1086/324626
Ardanuy C, Cercenado E, Morosini MI, Torres C. Detección fenotípica de mecanismos de resistencia en grampositivos. Enferm Infecc Microbiol Clin. 2012;30:325-32. https://doi.org/10.1016/j.eimc.2011.09.009
Some similar items:
- Yeny Zulay Castellanos, Zulma Milena Cucunubá, Astrid Carolina Flórez, Luis Carlos Orozco-Vargas, Reproducibility of serological tests for the diagnosis of Trypanosoma cruzi infection in pregnant women in an endemic area of Santander, Colombia , Biomedica: Vol. 34 No. 2 (2014)
- Carmen Acosta, Xiomara Pérez, Regla Herrera, Raquel García, Presence of IgG antibodies for rubella, herpes simplex and cytomegalovirus in pregnant women living in Havana City , Biomedica: Vol. 21 No. 2 (2001)
- R. López, Xiomara Pérez, E. Guerra, R. Herrera, Carmen Acosta, Toxoplasmosis entre mujeres embarazadas en Ciudad de La Habana , Biomedica: Vol. 13 No. 4 (1993)
- Hernando Baquero, María Elena Venegas Martinez, Lorena Velandia Forero, Fredy Neira Safi, Edgar Navarro, Neonatal late-onset infection with SARS CoV-2 , Biomedica: Vol. 40 No. Supl. 2 (2020): SARS-CoV-2 y COVID-19
- Sergio Iván Agudelo, Carlos Federico Molina, Óscar Andrés Gamboa, Juan David Suárez, Direct costs of neonatal infection acquired in the community in full-term newborns and low risk at birth, Cundinamarca, Colombia , Biomedica: Vol. 41 No. 1 (2021)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























