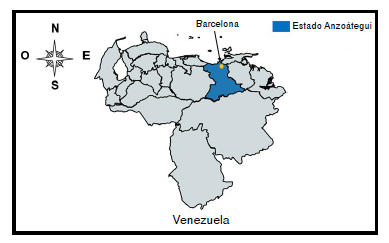
Infección por Trypanosoma cruzi en mujeres puérperas y sus neonatos en Barcelona, estado Anzoátegui, Venezuela
Resumen
Introducción. Trypanosoma cruzi se transmite principalmente por vía vectorial, sin embargo, las rutas oral y congénita han tomado relevancia.
Objetivo. Evaluar la infección por T. cruzi en mujeres puérperas y sus neonatos en el Hospital Universitario Dr. Luis Razetti de Barcelona, estado Anzoátegui, Venezuela.
Materiales y métodos. Se hizo un estudio prospectivo de corte transversal, de mayo de 2015 a agosto de 2016, en el que se evaluaron 1.200 mujeres para determinar la infección mediante las pruebas ELISA, MABA e IFI. Los neonatos de las madres seropositivas se evaluaron con la prueba de PCR y por serología a los nueve meses de edad. Se estimó la prevalencia de la infección por T. cruzi en mujeres puérperas y sus neonatos. Para establecer los factores de riesgo asociados a la infección, se usó la prueba de ji al cuadrado (c2) y la razón de probabilidad (OR).
Resultados. En total, 78 (6,50 %) mujeres resultaron positivas (IC95% 5,10-7,89 %). En seis (9,09 %) recién nacidos de madres seropositivas, se detectó ADN parasitario. Tras nueve meses de nacidos, once lactantes evaluados resultaron serológicamente negativos. La infección estuvo asociada con la duración del embarazo (OR=0,36; IC95% 0,15-0,84), origen del domicilio actual (OR=0,34; IC95% 0,24-0,62) o previo (OR=2,50; IC95% 1,38-4,52) y el tener familiares con la enfermedad de Chagas (OR=1,75; IC95% 1,02-3,01).
Conclusiones. La seroprevalencia para la infección por T. cruzi en mujeres puérperas del medio rural, fue elevada. La detección de ADN parasitario al momento del nacimiento no es indicativa de enfermedad de Chagas congénita.
Descargas
Referencias bibliográficas
World Health Organization. Chagas disease in Latin America: An epidemiological update based on 2010 estimates. Wkly Epidemiol Rec. 2015;90:33-43.
Molina I, Salvador F, Sánchez A. Update Chagas disease. Enferm Infecc Microbiol Clin. 2016;34:132-8. https://doi.org/10.1016/j.eimc.2015.12.008
Carlier Y, Sosa S, Luquetti A, Buekens P. Congenital Chagas disease: An update. Mem Inst Oswaldo Cruz. 2015;110:363-8. https://doi.org/10.1590/0074-02760140405
Colimon KM. Fundamentos de epidemiología. Tercera edición. Medellín: Coorporación para Investigaciones Biológicas; 2010. p. 551.
Bezares B, Sanz O, Jiménez I. Puerperal pathology. An Sist Sanit Navar. 2009;32:169-75. https://doi.org/10.23938/ASSN.0184
Berrizbeitia M, Seijas N, Rodríguez J, Jorquera A, Romero L. Estandarización, validación de la prueba de inmunofluorescencia indirecta y su uso en un estudio epidemiológico de la infección por Trypanosoma cruzi, en una comunidad rural del estado Sucre, Venezuela. Revista de la Sociedad Venezolana de Microbiología. 2015;35:53-9.
Ndao M, Kelly N, Normandin D, Maclean J, Whiteman A, Kokoskin E, et al. Trypanosoma cruzi infection of squirrel monkeys: Comparison of blood smear examination, commercial enzyme-linked immunosorbent assay, and polymerase chain reaction analysis as screening tests for evaluation of monkey-related injuries. Comp Med. 2000;50:658-65.
Berrizbeitia M, Ndao M, Bubis J, Gottschalk M, Aché A, Lacouture S, et al. Field evaluation of four novel enzyme immunoassays for Chagas’ disease in Venezuela blood banks: Comparison of assays using fixed-epimastigotes, fixed-trypomastigotes or trypomastigote excreted-secreted antigens from two Trypanosoma cruzi strains. Transfus Med. 2006;16:419-31. https://doi.org/10.1111/j.1365-3148.2006.00703.x
Noya O, Alarcón de Noya B. The multiple antigen blot assay (MABA): A simple immunoenzimatic technique for simultaneous screening of multiple antigens. Immunol Lett. 1998;63:53-6. https://doi.org/10.1016/S0165-2478(98)00055-8
Berrizbeitia M, Estaba A, Pozo A, Jorquera A, Rodulfo H. Comparación entre dos pruebas de reacción en cadena de la polimerasa (PCR satélite y PCR kinetoplasto) para la detección de ADN de Trypanosoma cruzi en heces de triatominos. Saber. 2017;29:767-74.
Mendoza C, Córdova E, Juárez J, Saldaña J, Torres A, Velásquez R, et al. The prevalence of Chagas’ disease in puerperal women and congenital transmission in an endemic area of Perú. Rev Panam Salud Pública. 2005;17:147-53.
Cardoso E, Valdez G, Campos AC, De la Luz-Sánchez R, Mendoza CR, Hernández AP, et al. Maternal fetal transmission of Trypanosoma cruzi: A problem of public health little studied in México. Exp Parasitol. 2012;131:425-32. https://doi.org/10.1016/j.exppara.2012.05.013
Castellanos-Domínguez Y, Cucunubá ZM, Orozco LC, Valencia-Hernández CA, León CM, Flórez AC, et al. Risk factors associated with Chagas disease in pregnant women in Santander, a highly endemic Colombian area. Trop Med Int Health. 2016;21:140-8. https://doi.org/10.1111/tmi.12634
Carrera C, Narváez AO, Muzzio J, Shiguango G, Robles LM, Herrera C, et al. Seroprevalence of Trypanosoma cruzi infection in schoolchildren and in pregnant women from an Amazonian Region in Orellana Province, Ecuador. Am J Trop Med Hyg. 2015;93:774-8. https://doi.org/10.4269/ajtmh. 14-0807
Brutus L, Castillo H, Bernal C, Salas NA, Schneider D, Santalla JA, et al. Detectable Trypanosoma cruzi parasitemia during pregnancy and delivery as a risk factor for congenital Chagas disease. Am J Trop Med Hyg. 2010;83:1044-7. https://doi.org/10.4269/ajtmh .2010.10-0326
Kaplinski M, Jois M, Galdós-Cárdenas G, Rendell VR, Shah V, Do RQ, et al. Sustained domestic vector exposure is associated with increased Chagas cardiomyopathy risk but decreased parasitemia and congenital transmission risk among young women in Bolivia. Clin Infect Dis. 2015;61:918-26. https://doi.org/10.1093/cid/civ446
Sosa-Estani S, Dri L, Touris C, Abalde S, Dell’arciprete A, Braunstein J. Vectorial and congenital transmission of Trypanosoma cruzi in Las Lomitas, Formosa. Medicina (B. Aires). 2009;69:424-30.
Mastrolonardo V, Ramos D, Paravisini I, Morales J. Tripanosomiasis en el embarazo. Rev Obstet Ginecol Venez. 2013;73:149-56.
Alarcón de Noya B, Pérez G, Díaz Z, Dickson S, Muñoz A, Hernández C, et al. Description of an oral Chagas disease outbreak in Venezuela, including a vertically transmitted case. Mem Inst Oswaldo Cruz. 2017;112:569-71. https://doi.org/10.1590/0074-027601700 09
Carlier Y, Truyens C. Congenital Chagas disease as an ecological model of interactions between Trypanosoma cruzi parasites, pregnant women, placenta and fetuses. Acta Trop. 2015;151:103-15. https://doi.org/10.1016/j.actatropica.2015.07.016
Zingales B, Miles M, Campbell DA, Tibayrenc M, Macedo AM, Teixeira MM, et al. The revised Trypanosoma cruzi subspecific nomenclature: Rationale, epidemiological relevance and research applications. Infect Genet Evol. 2012;12:240-53. https://doi.org/10.1016/j.meegid.2011.12.00
Gomes Y, Lorena V, Luquetti A. Diagnosis of Chagas disease: What has been achieved? What remains to be done with regard to diagnosis and follow up studies? Mem Inst Oswaldo Cruz. 2009;104:115-21. https://doi.org/10.1590/S0074-02762009000900017
Apt W, Zulantay I, Arnello M, Oddó D, González S, Rodríguez J, et al. Congenital infection by Trypanosoma cruzi in an endemic area of Chile: A multidisciplinary study. Trans R Soc Trop Med Hyg. 2013;107:98-104. https://doi.org/10.1093/trstmh/trs013
Carlier Y, Torrico F. Congenital infection with Trypanosoma cruzi: From mechanisms of transmission to strategies for diagnosis and control. Rev Soc Bras Med Trop. 2003;36:767-71.
Campos G, Canseco L, González F, Alfaro O, Nava I, Jiménez E. Transmisión materno-fetal de Trypanosoma cruzi, un problema de salud poco estudiado en México: caso Chiapas. Salud Pública Mex. 2016;58:378-84.
Brasil P, De Castro L, Hasslocher A, Sangenis L, Braga J. ELISA versus PCR for diagnosis of chronic Chagas disease: Systematic review and meta-analysis. BMC Infect Dis. 2010;10:337. https://doi.org/10.1186/1471-2334-10-337
Castro AM, Luquetti AO, Rassi A, Rassi GG, Chiari E, Galvão LM. Blood culture and polymerase chain reaction for the diagnosis of the chronic phase of human infection with Trypanosoma cruzi. Parasitol Res. 2002;88:894-900. https://doi.org/10.1007/s00436-002-0679-3
Bern C, Verastegui M, Gilman R, La Fuente C, Galdós-Cárdenas G, Calderón M, et al. Congenital Trypanosoma cruzi transmission in Santa Cruz, Bolivia. Clin Infect Dis. 2009;49:1667-74. https://doi.org/10.1086/648070
De Rissio AM, Riarte AR, García M, Esteva M, Quaglino M, Ruiz A. Congenital Trypanosoma cruzi infection. Efficacy of its monitoring in an urban reference health center in a non-endemic area of Argentina. Am J Trop Med Hyg. 2010;82:838-45. https://doi.org/10.4269/ajtmh.2010.08-0383
Ortí R, Parada M. Prevalencia de tripanosomiasis americana en mujeres gestantes de un área de salud. Valencia, 2005-2007. Rev Esp Salud Pública. 2009;83:543-55.
Cucunubá Z, Valencia C, Flórez C, León Y, Castellanos A, Cárdenas P, et al. Pilot program for surveillance of congenital Chagas disease in Colombia 2010-2011. Int J Infect Dis. 2012;16:e343.
Cucunubá Z, Florez A, Cárdenas A, Pavía P, Montilla M, Aldana R, et al. Prevalence and risk factors for Chagas disease in pregnant women in Casanare, Colombia. Am J Trop Med Hyg. 2012;87:837-42. https://doi.org/10.4269/ajtmh.2012.12-0086
Cevallos AM, Hernández R. Chagas’ disease: Pregnancy and congenital transmission. Biomed Res Int. 2014;2014:401864. https://doi.org/10.1155/2014/401864
Ávila O, Liendo P, Martínez L, Martínez T, Pocheville MI, Egurbide MV. Prevalence of Trypanosoma cruzi infection and vertical transmission in Latin-American pregnant women in a health area of Biscay. Enferm Infecc Microbiol Clin. 2013;31:210-6. https://doi.org/10.1016/j.eimc.2012.01.029
Torrico F, Alonso-Vega C, Suárez E, Rodríguez P, Torrico MC, Dramaix M, et al. Maternal Trypanosoma cruzi infection, pregnancy outcome, morbidity, and mortality of congenitally infected and non-infected newborns in Bolivia. Am J Trop Med Hyg. 2004;70:201-9.
Sanmartino M, Crocco CL. Conocimientos sobre la enfermedad de Chagas y factores de riesgo en comunidades epidemiológicamente diferentes de Argentina. Rev Panam Salud Pública. 2000;7:173-8.
Sasagawa E, Aiga H, Corado EY, Cuyuch BL, Hernández MA, Guevara AV, et al. Risk factors for Chagas disease among pregnant women in El Salvador. Trop Med Int Health. 2015;20:268-76. http://doi.org/10.1111/tmi.12440
Algunos artículos similares:
- Noris García-Jordán, Mariolga Berrizbeitia, Juan Luis Concepción, Elis Aldana, Ana Cáceres, Wilfredo Quiñones, Estudio entomológico de vectores transmisores de la infección por Trypanosoma cruzi en la población rural del estado Sucre, Venezuela , Biomédica: Vol. 35 Núm. 2 (2015)
- Idialis Hernández , Milenen Hernández, Jeny González, Ivonne Gómez, Orlando Zulueta, Grisell Ramos, Darien Ortega, Dunia Clara Bequer, Giosvany Ernesto Martínez, Aurora Delahanty, Evaluación del UMELISA CHAGAS® con la incorporación de nuevos péptidos monoméricos y quiméricos representativos de diferentes regiones de Trypanosoma cruzi , Biomédica: Vol. 41 Núm. Supl. 1 (2021): Mayo, Parasitología médica
- Ángela Liliana Monroy, Adriana María Pedraza, Carlos Fernando Prada, Prevalencia de anticuerpos anti-Trypanosoma cruzi en mujeres en edad fértil en Socotá, Boyacá, 2014 , Biomédica: Vol. 36 (2016): Suplemento 1, Microbiología médica
- Mónica Llano, Paula Pavía, Astrid Carolina Flórez, Adriana Cuéllar, John Mario González, Concepción Judith Puerta, Evaluación preliminar de la prueba comercial Chagas (Trypanosoma cruzi) IgG-ELISA® en individuos colombianos , Biomédica: Vol. 34 Núm. 2 (2014)
- Olga Serrano, Florencio Mendoza, Benny Suárez, Ana Soto, Seroepidemiología de la enfermedad de Chagas en dos localidades del municipio Costa de Oro, estado Aragua, Venezuela , Biomédica: Vol. 28 Núm. 1 (2008)
- Laura Mayela Montes-Rincón, Lucio Galaviz-Silva, Zinnia Judith Molina-Garza, Anticuerpos anti-Trypanosoma cruzi en migrantes latinoamericanos en tránsito por el cruce fronterizo entre México y los Estados Unidos , Biomédica: Vol. 38 Núm. 1 (2018)
- Héctor de Lima, José Carrero, Armando Rodríguez, Zoraya de Guglielmo, Noris Rodríguez, Trypanosomatidae de importancia en salud pública en animales silvestres y sinantrópicos en un area rural del municipio Tovar del estado Mérida, Venezuela. , Biomédica: Vol. 26 Núm. 1 (2006)
- Mariolga Berrizbeitia, Juan Luis Concepcion, Valentina Carzola, Jessicca Rodríguez, Ana Cáceres, Wilfredo Quiñones, Seroprevalence of T. cruzi infection in Canis familiaris, state of Sucre, Venezuela , Biomédica: Vol. 33 Núm. 2 (2013)
- María Clara Echeverry, Nubia Catalina Tovar, Guillermo Mora, Presencia de anticuerpos contra neurorreceptores cardiacos de acetilcolina muscarínicos tipo II en pacientes con enfermedad de Chagas e implantación de marcapasos , Biomédica: Vol. 29 Núm. 3 (2009)
- Elsa Nieves, Néstor Villarreal, Maritza Rondón, Mireya Sánchez, José Carrero, Evaluación de conocimientos y prácticas sobre la leishmaniasis tegumentaria en un área endémica de Venezuela , Biomédica: Vol. 28 Núm. 3 (2008)
| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |

























