Mielopatía por déficit de cobre: serie de casos y revisión de la literatura
Resumen
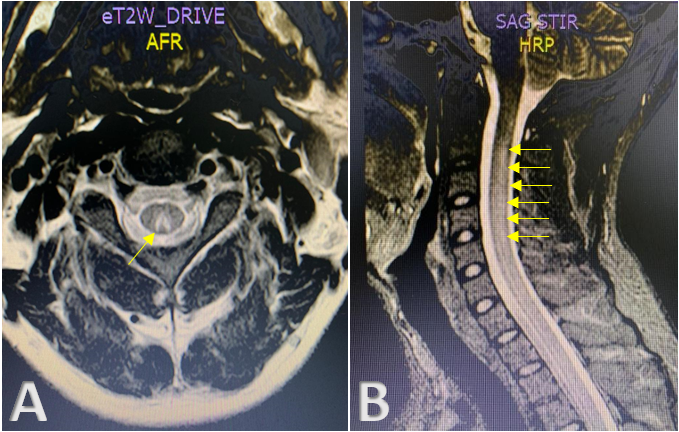
El déficit de cobre puede presentarse como una mielopatía y manifestarse como una ataxia sensorial secundaria a una desmielinización de los cordones posteriores de la médula espinal. Puede acompañarse de citopenias, principalmente anemia y leucopenia.
Se presenta una serie de casos de tres pacientes con mielopatía por déficit de cobre, diagnosticados y manejados desde el año 2020 al 2022 en un hospital universitario de alta complejidad en Colombia.
Dos de los casos eran mujeres. El rango de edad fue entre 57 y 68 años. En los tres casos, los niveles séricos de cobre estaban disminuidos y en dos de ellos, se descartaron diferentes causas de mielopatía que afectan los cordones posteriores de la médula espinal como el déficit de vitamina B12, vitamina E y ácido fólico, tabes dorsal, mielopatía por virus de la inmunodeficiencia humana, esclerosis múltiple e infección por el virus linfotrópico humano de tipo I y II, entre otras. Sin embargo, un paciente tenía deficiencia de vitamina B12 asociada con de cobre en el momento del diagnóstico de la mielopatía. En los tres casos hubo ataxia sensitiva y en dos, la paraparesia fue el déficit motor inicial.
Descargas
Referencias bibliográficas
Altarelli M, Ben-hamouda N, Schneider A, Berger M. Copper deficiency: causes, manifestations, and treatment. Nutr Clin Pract. 2019;34:504-13. https://doi.org/10.1002/ncp.10328
Moon N, Aryan M, Westerveld D, Nathoo S, Glover S, Kamel AY. Clinical manifestations of copper deficiency: a case report and review of the literature. Nutr Clin Pract. 2021;36:1080-5. https://doi.org/10.1002/ncp.10582
Turnlund JR. Human whole-body copper metabolism. Am J Clin Nutr. 1998;67:960-4. https://doi.org/10.1093/ajcn/67.5.960S
European Food Safety Authority Panel on Dietetic Products, Nutrition and Allergies. Scientific opinion on dietary reference values for copper. EFSA J. 2015;13:4253. https://doi.org/10.2903/j.efsa.2015.4253
Goodman BP. Metabolic and toxic causes of myelopathy. Continuum (Minneap. Minn). 2015;21:84-99. https://doi.org/10.1212/01.CON.0000461086.79241.3b
Slama MCC, Berkowitz AL. Metabolic and toxic myelopathies. Semin Neurol. 2021;41:427-40. https://doi.org/10.1055/s-0041-1725150
Gletsu-Miller N, Broderius M, Frediani JK, Zhao VM, Griffith DP, Davis SS, et al. Incidence and prevalence of copper deficiency following Roux-en-y gastric bypass surgery. Int J Obes. 2012;36:328-35. https://doi.org/10.1038/ijo.2011.159
Chhetri SK, Mills RJ, Shaunak S, Emsley HCA. Copper deficiency. BMJ. 2014;348:g3691. https://doi.org/10.1136/bmj.g3691
Naismith RT, Shepherd JB, Weihl CC, Tutlam NT, Cross AH. Acute and bilateral blindness due to optic neuropathy associated with copper deficiency. Arch Neurol. 2009;66:1025-7. https://doi.org/10.1001/archneurol.2009.70
Myint ZW, Oo TH, Thein KZ, Tun AM, Saeed H. Copper deficiency anemia: review article. Ann Hematol. 2018;97:1527–34. https://doi.org/10.1007/s00277-018-3407-5
Halfdanarson TR, Kumar N, Li C, Phyliky RL, Hogan WJ. Hematological manifestations of copper deficiency: a retrospective review. Eur J Haematol. 2008;80:523-31. https://doi.org/10.1111/j.1600-0609.2008.01050.x
Kumar P, Hamza N, Madhok B, De Alwis N, Sharma M, Miras AD, et al. Copper deficiency after gastric bypass for morbid obesity: a systematic review. Obes Surg. 2016;26:1335-42. https://doi.org/10.1007/s11695-016-2162-8
Lewis CA, de Jersey S, Seymour M, Hopkins G, Hickman I, Osland E. Iron, vitamin B12, folate and copper deficiency after bariatric surgery and the impact on anaemia: a systematic review. Obes Surg. 2020;30:4542–91. https://doi.org/10.1007/s11695-020-04872-y
Poujois A, Djebrani-Oussedik N, Ory-Magne F, Woimant F. Neurological presentations revealing acquired copper deficiency: diagnosis features, aetiologies and evolution in seven patients. Intern Med J. 2018;48:535-40. https://doi.org/10.1111/imj.13650
Huff JD, Keung YK, Thakuri M, Beaty MW, Hurd DD, Owen J, et al. Copper deficiency causes reversible myelodysplasia. Am J Hematol. 2007;82:625–30. https://doi.org/10.1002/ajh.20864
Farkas GJ, Pitot MA, Berg AS, Gater DR. Nutritional status in chronic spinal cord injury: a systematic review and meta-analysis. Spinal Cord. 2019;57:3–17. https://doi.org/10.1038/s41393-018-0218-4
Gwathmey KG, Grogan J. Nutritional neuropathies. Muscle Nerve. 2020;62:13-29. https://doi.org/10.1002/mus.26783
Goodman BP, Bosch EP, Ross MA, Hoffman-Snyder C, Dodick DD, Smith BE. Clinical and electrodiagnostic findings in copper deficiency myeloneuropathy. J Neurol Neurosurg Psychiatry. 2009;80:524-7. https://doi.org/10.1136/jnnp.2008.144683
Wazir SM, Ghobrial I. Copper deficiency, a new triad: anemia, leucopenia, and myeloneuropathy. J Community Hosp Intern Med Perspect. 2017;7:265-8. https://doi.org/10.1080/20009666.2017.1351289
Kranz PG, Amrhein TJ. Imaging approach to myelopathy: acute, subacute, and chronic. Radiol Clin North Am. 2019;57:257-79. https://doi.org/10.1016/j.rcl.2018.09.006
Sarbu N, Lolli V, Smirniotopoulos JG. Magnetic resonance imaging in myelopathy: a pictorial review. Clin Imaging. 2019;57:56-68. https://doi.org/10.1016/j.clinimag.2019.05.002
Schwendimann R. Metabolic and toxic myelopathies. Continuum (Minneap. Minn). 2018; 24:427-40. https://doi.org/10.1212/CON.0000000000000596
Kumar N. Neurologic presentations of nutritional deficiencies. Neurol Clin. 2010;28:107-70. https://doi.org/10.1016/j.ncl.2009.09.006
Urtiaga S, Terrero R, Malumbres M, Pinel A. Mielopatía por déficit de cobre: la gran simuladora. Neurologia. 2018;33:278-81. https://doi.org/10.1016/j.nrl.2017.02.009
Mechanick JI, Youdim A, Jones DB, Garvey T, Hurley DL, McMahon M, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 Update: Cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity (Silver Spring). 2013;21(Suppl.1):S1-27. https://doi.org/10.1002/oby.20461
Algunos artículos similares:
- Rosa Magdalena Uscátegui, Adriana M. Correa, Jaime Carmona-Fonseca, Cambios en las concentraciones de retinol, hemoglobina y ferritina en niños palúdicos colombianos , Biomédica: Vol. 29 Núm. 2 (2009)
- Elpidia Poveda, Alexandra Cuartas, Saralicia Guarín, Yibby Forero, Elsa Villarreal, Estado de los micronutrientes hierro y vitamina A, factores de riesgo para las deficiencias y valoración antropométrica en niños preescolares del municipio de Funza, Colombia , Biomédica: Vol. 27 Núm. 1 (2007)
- Margarita Arboleda, María Fernanda Pérez, Diana Fernández, Luz Yaned Usuga, Miler Meza, Perfil clínico y de laboratorio de los pacientes con malaria por Plasmodium vivax, hospitalizados en Apartadó, Colombia , Biomédica: Vol. 32 (2012): Suplemento 1, Malaria
- Beatriz Elena Parra, Luz Mariela Manjarrés, Alba Lucía Gómez, Dora María Alzate, María Clemencia Jaramillo, Evaluación de la educación nutricional y un suplemento para prevenir la anemia durante la gestación. , Biomédica: Vol. 25 Núm. 2 (2005)
- Ángela Medina, David López, Luis Reinel Vásquez, Pediculosis capitis grave en una niña inscrita en una guardería , Biomédica: Vol. 39 Núm. 4 (2019)
- Carlos Julio Vargas-Potes, Diana Marcela Mendoza-Urbano, Luis Gabriel Parra-Lara , Ángela R. Zambrano, Desafíos en el manejo del sarcoma de Ewing en una paciente testigo de Jehová , Biomédica: Vol. 43 Núm. 1 (2023)
Derechos de autor 2023 Biomédica

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.
| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |

























