Seroprevalence of Chagas disease and associated risk factors in a population of Morroa, Sucre
Keywords:
Trypanosoma cruzi, Chagas disease, serology, risk factors, Elisa test, epidemiology
Abstract
Introduction. Chagas disease is a major public health problem in Latin America. In Colombia, a large area has the ecoepidemiological conditions which favor the active transmition of this infection.Objective. This study was undertaken in a population from the municipality of Morroa, Sucre Province, to evaluate risk factors and to determine the seroprevalence to Chagas disease.
Materials and methods. A questionnaire was given to a sample population of 122 people classed as rural (n=76) or urban area (n = 46). A serological screening was undertaken by Elisa test, with confirmation of seropositives with IHA (Chagatest®) and parasitological confirmation by polymerase chain reaction (PCR).
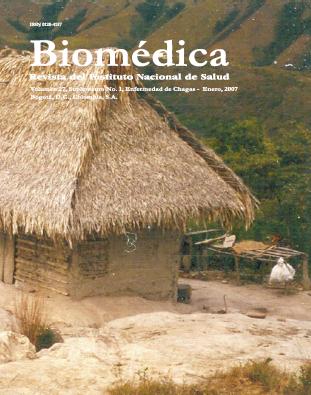
Results. Four people were positive by Elisa test (3.3%); however, they were negative by IHA and PCR. One of the four positives by Elisa was positive by indirect immuno flourescence (IFAT) as well. The sample showed a low presence of seropositives against Trypanosoma cruzi. However, the presence of parasite could not be confirmed by the PCR test.The main risk factors were houses thatched with palm roofs, clay floors, wood walls, and presence of domestic animal reservoirs.
Conclusions. The study population presented risk factors for the establishment of active transmission. The presence of triatomines must be verified in this area and establishment of control measures are necessary for preventiving the resurgence of the Chagas disease in Morroa.
Downloads
Download data is not yet available.
References
1. Atias A. Parasitología médica. Santiago de Chile: Publicaciones Técnicas Mediterráneas Ltda.: 1999. p. 251-64.
2. World Health Organization. Control of Chagas disease. Second Report of the WHO Expert Committee. Technical reports series 905. Geneva: WHO; 2002.
3. Moncayo A. Chagas disease: current epidemiological trends after the interruption of vectorial and transfusional transmission in the southern cone countries. Mem Inst Oswaldo Cruz 2003;98:577-91.
4. Cannova D, Aguilar M, Pacheco M, Simona M, Medina M. Validación del inmunoensayo enzimático (Elisa) y hemoaglutinación indirecta (HAI) para el serodiagnóstico de la enfermedad de Chagas. Salus
2002;6:4-9.
5. Gutierrez R, Angulo VM, Tarazona Z, Britto M, Fernandez O. Comparison of four serological tests for the diagnosis of Chagas disease in a Colombian endemic area. Parasitology 2004;129:439-44.
6. Kirchhoff LV, Votava JR, Ochs DE, Moser DR. Comparison of PCR and microscopic methods for detecting Trypanosoma cruzi. J Clin Microbiol 1996;34:1171-5.
7. Molina JA, Gualdron LE, Brochero HL, Olano VA, Barrios D, Guhl F. Distribución actual e importancia epidemiológica de las especies de triatominos (Reduviidae: Triatominae) en Colombia. Biomédica
2000;20:344-60.
8. Guhl F, Restrepo M, Angulo VM, Antunes CM, Campbell-Lendrum D, Davies C. Lessons from a national survey of Chagas disease transmission risk in Colombia. Trends Parasitol 2005;21:259-62.
9. Gea S, Rodriguez P, Vottero-Cima E. Characterization of Trypanosoma cruzi antigens recognized by sera from patients with chronic Chagas disease. Int Archs Allergy Appl Immun 1987;84:410-3.
10.Takasu N, Masuko T, Hojo H, Hashimoto Y. A microplate-immunofluorescence assay for anti-Trypanosoma cruzi antibodies. Tohoku J Exp Med 1989;159:307-12.
11. Agudelo L. Ecoepidemiología de la enfermedad de Chagas en la cuenca del Río Palomino, Sierra Nevada de Santa Marta. (Tesis de maestría) Medellín: Universidad de Antioquia; 2006.
12. Sambrook J, Fritsh E, Maniatis T. Molecular cloning. A laboratory manual. New York: Cold Spring Harbor Laboratory; 1989. p.223-45.
13. Moser D, Kirchhoff L, Donelson J. Detection of Trypanosoma cruzi by DNA amplification using the polymerase chain reaction. J Clin Microbiol 1989;27:1477-82.
14. Lent H, Wigodzinsky P. Revision of the Triatominae (Hemiptera, Reduviidae), and their significance as vectors of Chagas disease. Bull Am Mus Nat Hist 1979;163:123-520.
15. Márquez J, Palencia J. Detección de Trypanosoma cruzi en una población de triatominos (Triatoma maculata) en Córdoba, Bolívar. (Tesis de grado). Sincelejo: Universidad de Sucre; 2004.
16. Gaunt M, Miles M. The ecotopes and evolution of Triatomine bugs (Triatominae) and their associated trypanosomes. Mem Inst Oswaldo Cruz 2000;95:557-65.
17. Pizarro JC, Romaña C. Variación estacional de una población silvestre de Rhodnius pallescens (Heteroptera: Triatominae) BARBER 1932 en la costa Caribe colombiana. Bull Inst Fr Etudes Audines
1998;27:309-25.
18. Cortés L, Suárez H. Triatominos (Reduviidae: Triatominae) en un foco de enfermedad de Chagas en Talaigua Nuevo (Bolívar, Colombia). Biomédica 2005;25:568-74.
19. Segura E, Escobar-Mesa A, Grupo de Estudio Sobre la Enfermedad de Chagas. Epidemiología de la enfermedad de Chagas en el estado de Veracruz. Salud Pública Méx 2005;47:201-8.
20. Sanmartino M, Crocco L. Conocimientos sobre la enfermedad de Chagas y factores de riesgo en comunidades epidemiologicamente diferentes de Argentina. Rev Panam Salud Pública 2000;7:173-8.
21. Valente VC, Valente SA, Noireau F, Carrasco HJ, Miles MA. Chagas disease in the amazon basin: association of Panstrongylus geniculatus (Hemíptera, Reduviidae) with domestic pigs. J Med Entomol
1998;35:99-103.
22. D'Alessandro A, Barreto P, Thomas M. Nuevos registros de triatominos domiciliarios y extradomiciliarios en Colombia. Colombia Médica 1981;12:75-85.
23. Corredor A, Santacruz M, Gomez S, Guatame L. Distribución de los triatominos domiciliados en Colombia. Bogotá: Instituto Nacional de Salud; 1990.
24. Poyet G. Contexte écologique de Rhodnius pallescens (Heteroptera: Reduviidae) vecteur de la maladie de Chagas, dans son biotope natural, le palmera Attalea butyraceae: peuplement de l'entomofaune associée et estratégies adaptatives Rhodnius pallescens. Mémoire de maítrise de biologie des organismos et des populations. Paris: Université Pierre et Marie Curie; 1995.
25. Cárdenas J, Mazariego M. Anticuerpos anti-Trypanosoma cruzi en pacientes con cardiomiopatía dilatada. Rev Med IMSS 2003;41:111-4.
26. Enciso C, Montilla M, Santacruz M, Nicholls S, Rodríguez A, Mercado M, et al. Comparación de la prueba de inmunofluorescencia indirecta, un inmunoensayo enzimático y la prueba comercial
Chagatek® para la detección de anticuerpos anti-Trypanosoma cruzi. Biomédica 2004;24:104-8.
27. Guhl F, Jaramillo C, Carranza JC, Vallejo GA. Molecular characterization and diagnosis of Trypanosoma cruzi and T. rangeli. Arch Med Res 2002;33:362-70.
28. Marcon GE, Andrade PD, de Alburquerque DM, Wanderley Jda S, de Almeida EA, Guariento ME, et al. Use of a nested polymerase chain reaction (N-PCR) to detect Trypanosoma cruzi in blood samples
from chronic chagasic patients and patients' doubtful serologies. Diagn Microbiol Infect Dis 2002;43:39-43.
2. World Health Organization. Control of Chagas disease. Second Report of the WHO Expert Committee. Technical reports series 905. Geneva: WHO; 2002.
3. Moncayo A. Chagas disease: current epidemiological trends after the interruption of vectorial and transfusional transmission in the southern cone countries. Mem Inst Oswaldo Cruz 2003;98:577-91.
4. Cannova D, Aguilar M, Pacheco M, Simona M, Medina M. Validación del inmunoensayo enzimático (Elisa) y hemoaglutinación indirecta (HAI) para el serodiagnóstico de la enfermedad de Chagas. Salus
2002;6:4-9.
5. Gutierrez R, Angulo VM, Tarazona Z, Britto M, Fernandez O. Comparison of four serological tests for the diagnosis of Chagas disease in a Colombian endemic area. Parasitology 2004;129:439-44.
6. Kirchhoff LV, Votava JR, Ochs DE, Moser DR. Comparison of PCR and microscopic methods for detecting Trypanosoma cruzi. J Clin Microbiol 1996;34:1171-5.
7. Molina JA, Gualdron LE, Brochero HL, Olano VA, Barrios D, Guhl F. Distribución actual e importancia epidemiológica de las especies de triatominos (Reduviidae: Triatominae) en Colombia. Biomédica
2000;20:344-60.
8. Guhl F, Restrepo M, Angulo VM, Antunes CM, Campbell-Lendrum D, Davies C. Lessons from a national survey of Chagas disease transmission risk in Colombia. Trends Parasitol 2005;21:259-62.
9. Gea S, Rodriguez P, Vottero-Cima E. Characterization of Trypanosoma cruzi antigens recognized by sera from patients with chronic Chagas disease. Int Archs Allergy Appl Immun 1987;84:410-3.
10.Takasu N, Masuko T, Hojo H, Hashimoto Y. A microplate-immunofluorescence assay for anti-Trypanosoma cruzi antibodies. Tohoku J Exp Med 1989;159:307-12.
11. Agudelo L. Ecoepidemiología de la enfermedad de Chagas en la cuenca del Río Palomino, Sierra Nevada de Santa Marta. (Tesis de maestría) Medellín: Universidad de Antioquia; 2006.
12. Sambrook J, Fritsh E, Maniatis T. Molecular cloning. A laboratory manual. New York: Cold Spring Harbor Laboratory; 1989. p.223-45.
13. Moser D, Kirchhoff L, Donelson J. Detection of Trypanosoma cruzi by DNA amplification using the polymerase chain reaction. J Clin Microbiol 1989;27:1477-82.
14. Lent H, Wigodzinsky P. Revision of the Triatominae (Hemiptera, Reduviidae), and their significance as vectors of Chagas disease. Bull Am Mus Nat Hist 1979;163:123-520.
15. Márquez J, Palencia J. Detección de Trypanosoma cruzi en una población de triatominos (Triatoma maculata) en Córdoba, Bolívar. (Tesis de grado). Sincelejo: Universidad de Sucre; 2004.
16. Gaunt M, Miles M. The ecotopes and evolution of Triatomine bugs (Triatominae) and their associated trypanosomes. Mem Inst Oswaldo Cruz 2000;95:557-65.
17. Pizarro JC, Romaña C. Variación estacional de una población silvestre de Rhodnius pallescens (Heteroptera: Triatominae) BARBER 1932 en la costa Caribe colombiana. Bull Inst Fr Etudes Audines
1998;27:309-25.
18. Cortés L, Suárez H. Triatominos (Reduviidae: Triatominae) en un foco de enfermedad de Chagas en Talaigua Nuevo (Bolívar, Colombia). Biomédica 2005;25:568-74.
19. Segura E, Escobar-Mesa A, Grupo de Estudio Sobre la Enfermedad de Chagas. Epidemiología de la enfermedad de Chagas en el estado de Veracruz. Salud Pública Méx 2005;47:201-8.
20. Sanmartino M, Crocco L. Conocimientos sobre la enfermedad de Chagas y factores de riesgo en comunidades epidemiologicamente diferentes de Argentina. Rev Panam Salud Pública 2000;7:173-8.
21. Valente VC, Valente SA, Noireau F, Carrasco HJ, Miles MA. Chagas disease in the amazon basin: association of Panstrongylus geniculatus (Hemíptera, Reduviidae) with domestic pigs. J Med Entomol
1998;35:99-103.
22. D'Alessandro A, Barreto P, Thomas M. Nuevos registros de triatominos domiciliarios y extradomiciliarios en Colombia. Colombia Médica 1981;12:75-85.
23. Corredor A, Santacruz M, Gomez S, Guatame L. Distribución de los triatominos domiciliados en Colombia. Bogotá: Instituto Nacional de Salud; 1990.
24. Poyet G. Contexte écologique de Rhodnius pallescens (Heteroptera: Reduviidae) vecteur de la maladie de Chagas, dans son biotope natural, le palmera Attalea butyraceae: peuplement de l'entomofaune associée et estratégies adaptatives Rhodnius pallescens. Mémoire de maítrise de biologie des organismos et des populations. Paris: Université Pierre et Marie Curie; 1995.
25. Cárdenas J, Mazariego M. Anticuerpos anti-Trypanosoma cruzi en pacientes con cardiomiopatía dilatada. Rev Med IMSS 2003;41:111-4.
26. Enciso C, Montilla M, Santacruz M, Nicholls S, Rodríguez A, Mercado M, et al. Comparación de la prueba de inmunofluorescencia indirecta, un inmunoensayo enzimático y la prueba comercial
Chagatek® para la detección de anticuerpos anti-Trypanosoma cruzi. Biomédica 2004;24:104-8.
27. Guhl F, Jaramillo C, Carranza JC, Vallejo GA. Molecular characterization and diagnosis of Trypanosoma cruzi and T. rangeli. Arch Med Res 2002;33:362-70.
28. Marcon GE, Andrade PD, de Alburquerque DM, Wanderley Jda S, de Almeida EA, Guariento ME, et al. Use of a nested polymerase chain reaction (N-PCR) to detect Trypanosoma cruzi in blood samples
from chronic chagasic patients and patients' doubtful serologies. Diagn Microbiol Infect Dis 2002;43:39-43.
How to Cite
1.
Hoyos R, Pacheco L, Agudelo LA, Zafra G, Blanco P, Triana O. Seroprevalence of Chagas disease and associated risk factors in a population of Morroa, Sucre. biomedica [Internet]. 2007 Jan. 1 [cited 2024 May 11];27(1esp):130-6. Available from: https://revistabiomedica.org/index.php/biomedica/article/view/256
Some similar items:
- Liliana Torcoroma García, Jhancy Rocío Aguilar, Marly Yojhana Bueno , Erika Marcela Moreno, Herminia Ramírez , Nelson Daza , Disagreement between PCR and serological diagnosis of Trypanosoma cruzi infection in blood donors from a Colombian endemic region , Biomedica: Vol. 41 No. Supl. 1 (2021): Mayo, Parasitología médica
- Óscar Quirós-Gómez, Nicolás Jaramillo, Víctor Angulo, Gabriel Parra-Henao, Triatoma dimidiata in Colombia: Distribution, ecology and epidemiological importance , Biomedica: Vol. 37 No. 2 (2017)
- Lisbeth A. Hurtado, José E. Calzada, Vanesa Pineda, Kadir González, Ana María Santamaría, Lorenzo Cáceres, Coridalia Wald, Azael Saldaña, Knowledge and risk factors related to Chagas’ disease in two Panamanian communities where Rhodnius pallescens is the main vector , Biomedica: Vol. 34 No. 2 (2014)
- Rubén Santiago Nicholls, Zulma Milena Cucunubá, Angélica Knudson, Astrid Carolina Flórez, Marleny Montilla, Concepción Judith Puerta, Paula Ximena Pavía, Acute Chagas disease in Colombia: a rarely suspected disease. Report of 10 cases presented during the 2002-2005 period , Biomedica: Vol. 27 No. 1esp (2007): Enfermedad de Chagas
- María Clara Echeverry, Nubia Catalina Tovar, Guillermo Mora, Presence of antibodies to cardiac neuroreceptors in patients with Chagas disease , Biomedica: Vol. 29 No. 3 (2009)
- Dairo Alonso Rendón, Carlos M. Genes, Omar Triana, Myocardial cellular damage and the activity of the mitochondrial ATP synthase in rats infected with a Colombian strain of Trypanosoma cruzi , Biomedica: Vol. 27 No. 1esp (2007): Enfermedad de Chagas
- Sandra Paola Santander, Adriana Cuéllar, María del Carmen Thomas, Fanny Guzmán, Alberto Gómez, Manuel Carlos López, Concepción Puerta, Expression of markers on dendritic cells from chronic chagasic patients stimulated with the KMP-11 protein and the K1 peptide from Trypanosoma cruzi , Biomedica: Vol. 27 No. 1esp (2007): Enfermedad de Chagas
- Concepción Judith Puerta, Johana María Guevara, Paula Ximena Pavía, Marleny Montilla, Rubén Santiago Nicholls, Edgar Parra, Yuli Katherine Barrera, Evaluation of TcH2AF-R and S35-S36 primers in PCR tests for the detection of Trypanosoma cruzi in mouse cardiac tissue , Biomedica: Vol. 28 No. 4 (2008)
- Gladys Acuña-González, Carlo E. Medina-Solís, Gerardo Maupomé, Mauricio Escoffie-Ramírez, Jesús Hernández-Romano, María de L. Márquez-Corona, Arturo J. Islas-Márquez, Juan J. Villalobos-Rodelo, Family history and socioeconomic risk factors for non-syndromic cleft lip and palate: A matched case-control study in a less developed country , Biomedica: Vol. 31 No. 3 (2011)
- Luz Adriana Botero, Ana María Mejía, Omar Triana, Biological and genetic characterization of two Colombian clones of Trypanosoma cruzi groups I and II , Biomedica: Vol. 27 No. 1esp (2007): Enfermedad de Chagas
Section
Short communication
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |