Risk factors for hospital-acquired bacteremia due to carbapenem-resistant Pseudomonas aeruginosa in a Colombian hospital
Abstract
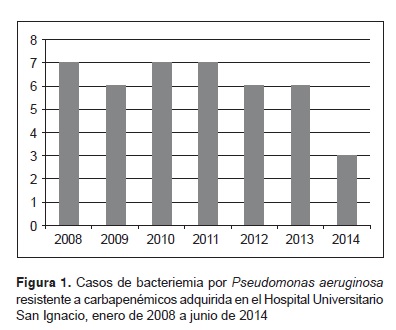
Introduction: Bacteremia due to Pseudomonas aeruginosa resistant to carbapenems is a public health problem due to the limitations it places on therapeutic options, as well as the increased time patients must spend in hospital, costs and the risk of mortality. Objective: To evaluate the risk factors for presentation of bacteremia due to carbapenem-resistant P. aeruginosa acquired in the Hospital Universitario San Ignacio between January 2008 and June 2014. Materials and methods: This was a case control study in which the case patients presented bacteremia due to P. aeruginosa resistant to carbapenems and the control group included patients with P. aeruginosa susceptible to this group of antibiotics. Variables such as the previous use of meropenem and ertapenem, immunosuppression and neoplasia were measured. Mortality and duration of hospital were also described. Results: In all, 168 patients were evaluated, of which 42 were cases and 126 controls. Using a multivariate model, the risk factors related to bacteremia due to carbapenem-resistant P. aeruginosa acquired in hospital were the following: use of parenteral nutrition (OR=8.28; 95% CI: 2.56-26.79; p=0); use of meropenem (OR=1.15; 95% CI: 1.03-1.28; p=0.01); and use of ciprofloxacin (OR=81.99; 95% CI: 1.14-5884; p=0.043). Conclusion: In order to prevent the emergence of carbapenem-resistant P. aeruginosa, antimicrobial control programs should be strengthened by promoting the prudent administration of carbapenems and quinolones. The correct use of parenteral nutrition should also be monitored.
Downloads
References
Horino T, Chiba A, Kawano S, Kato T, Sato F, Maruyama, et al. Clinical characteristics and risk factors for mortality in patients with bacteriemia caused by Pseudomonas aeruginosa. Intern Med. 2012;51:59-64. http://dx.doi.org/10.2169/internalmedicine.51.5698.
Morgan DJ, Rogawski E, Thom KA, Johnson JK, Perencevich EN, Shardell M, et al. Transfer of multidrug-resistant bacteria to healthcare workers' gloves and gowns after patient contact increases with environmental contamination. Crit Care Med. 2012;40:1045-51. http://dx.doi.org/10.1097/CCM.0b013e31823bc7c8.
Johnson JK, Smith G, Lee MS, Venezia RA, Stine OC, Nataro JP, et al. The role of patient-to-patient transmission in the acquisition of imipenem-resistant Pseudomonas aeruginosa colonization in the intensive care unit. J Infect Dis. 2009;200:900-5. http://dx.doi.org/10.1086/605408.
Suárez C, Peña C. Influence of carbapenem resistance on mortality and the dynamics of mortality in Pseudomonas aeruginosa bloodstream infection. Int J Infect Dis. 2010;14s:e73-e8. http://dx.doi.org/10.1016/j.ijid.2009.11.019.
Al-Hasan MN, Wilson JW, Lahr BD, Eckel-Passow JE, Baddour LM. Incidence of Pseudomonas aeruginosa bacteriemia: A population-based study. Am J Med. 2008;121:702-8. http://dx.doi.org/10.1016/j.amjmed.2008.03.029.
Hernández-Gómez C, Blanco VM, Motoa G, Correa A, Vallejo M, Villegas MV, et al. Evolución de la resistencia antimicrobiana de bacilos Gram negativos en unidades de cuidados intensivos en Colombia. Biomédica. 2014; 34(Suppl.1):91-100. http://dx.doi.org/10.7705/biomedica.v34i0.1667.
Villa LM, Cortés JA, Leal AL, Meneses A, Meléndez MP, GREBO. Resistance to antibiotics in Pseudomonas aeruginosa in Colombian hospitals. Rev Chilena Infectol. 2013;30:605-10. http://dx.doi.org/10.4067/S0716-10182013000600005.
Jeong SJ, Yoon SS, Bae IK, Jeong SH, Kim JM, Lee K. Risk factors for mortality in patients with bloodstream infections caused by carbapenem-resistant Pseudonoma aeruginosa: Clinical impact of bacterial virulence and strains on outcome. Diagn Microbiol Infect Dis. 2014;80:130-5. http://dx.doi.org/10.1016/j.diagmicrobio.2014.07.003.
Tumbarello M, Repetto E, Treacarichi EM, Bernardini C, De Pascale G, Parisini A, et al. Multidrug-resistant Pseudomonas aeruginosa bloodstream infections: Risk factors and mortality. Epidemiol Infect. 2011;139:1740-9. http://dx.doi.org/10.1017/S0950268810003055.
Micek ST, Lloyd AE, Ritchie DJ, Reichley RM, Fraser VJ, Kollef MH. Pseudomonas aeruginosa bloodstream infection: Importance of appropriate initial antimicrobial treatment. Antimicrob Agents Chemother. 2005;49:1306-11. http://dx.doi.org/10.1128/AAC.49.4.1306-1311.2005.
Tacconelli E, Cataldo MA, Dancer SJ, De Angelis G, Falcone M, Frank U, et al. European Society of Clinical Microbiology. ESCMID guidelines for the management of the infection control measures to reduce transmission of multidrug-resistant Gram-negative bacteria in hospitalized patients. Clin Microbiol Infect. 2014;20(Suppl.1):1-55. http://dx.doi.org/10.1111/1469-0691.12427.
Tuon F, Gortz L, Rocha J. Risk factors for pan-resistant Pseudomonas aeruginosa bacteriemia and the adequacy of antibiotic therapy. Braz J Infect Dis. 2012;16:351-6. http://dx.doi.org/10.1016/j.bjid.2012.06.009.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; approved standard. Twenty second information supplement. Document M100-S-22. Wayne: CLSI; 2012.
Hongsuwan M, Srisamang P, Kanoksil M, Luangasanatip N, Jatapai A, Day NP, et al. Increasing incidence of hospital-acquired and healthcare-associated bacteriemia in northeast Thailand: A multicenter surveillance study. PLoS One. 2014;9:e109324. http://dx.doi.org/10.1371/journal.pone.0109324.
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute Dialysis Quality Initiative workgroup. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: The Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8:R204-12. http://dx.doi.org/10.1186/cc2872.
El Amari EB, Chamot E, Auckenthaler R, Pechère JC, van Delden C. Influence of previous exposure to antibiotic therapy on the susceptibility pattern of Pseudomonas aeruginosa bacteremic isolates. Clin Infect Dis. 2001;33: 1859-64. http://dx.doi.org/10.1086/324346.
Falagas ME, Koletsi PK, Kopterides P, Michalopoulos A. Risk factors for isolation of strains susceptible only to polymyxin among patients with Pseudomonas aeruginosa bacteriemia. Antimicrob Agents Chemother. 2006;50:2541-3. http://dx.doi.org/10.1128/AAC.00224-06.
Lazcano-Ponce E, Salazar-Martínez E, Hernández-Ávila M. Case-control epidemiological studies: Theoretical bases, variants and applications. Salud Pública Mex. 2001;43:135-50.
Mikura S, Wada H, Okazaki M, Nakamura M, Honda K, Yasutake T, et al. Risk factors for bacteraemia attributable to Pseudomonas aeruginosa resistant to imipenem, levofloxacin, or gentamicin. J Hosp Infect. 2011;79:267-8. http://dx.doi.org/10.1016/j.jhin.2011.07.003.
Voor In't Holt AF, Severin JA, Lesaffre EM, Vos MC. A systematic review and meta-analyses show that carbapenem use and medical devices are the leading risk factors for carbapenem-resistant Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2014;58:2626-37. http://dx.doi.org/10.1128/AAC.01758-13.
Echeverri-Toro LM, Rueda ZV, Maya W, Agudelo Y, Ospina S. Multidrug-resistant Klebsiella pneumoniae, predisposing factors and associated mortality in a tertiary-care hospital in Colombia. Rev Chilena Infectol. 2012;29:175-82. http://dx.doi.org/10.4067/S0716-10182012000200009.
Masterton RG. Antibiotic de-escalation. Crit Care Clin. 2011;27:149-62. http://dx.doi.org/10.1016/j.ccc.2010.09.009.
Rodríguez-Osorio CA, Sánchez-Martínez CO, Araújo-Meléndez J, Criollo E, Macías-Hernández AE, Ponce-de-León A, et al. Impact of ertapenem on antimicrobial resistance in a sentinel group of Gram-negative bacilli: A 6 year antimicrobial resistance surveillance study. J Antimicrob Chemother. 2015;70:914-21. http://dx.doi.org/10.1093/jac/dku471.
Sousa D, Castelo-Corral L, Gutiérrez-Urbón JM, Molina F, López-Calviño B, Bou G, et al. Impact of ertapenem use on Pseudomonas aeruginosa and Acinetobacter baumannii imipenem susceptibility rates: Collateral damage or positive effect on hospital ecology? J Antimicrob Chemother. 2013;68:1917-25. http://dx.doi.org/10.1093/jac/dkt091.
Sligl W, Taylor G, Brindley PG. Five years of nosocomial Gram-negative bacteriemia in a general intensive care unit: Epidemiology, antimicrobial susceptibility patterns, and outcomes. Int J Infect Dis. 2006;10:320-5. http://dx.doi.org/10.1016/j.ijid.2005.07.003.
Morita Y, Tomida J, Kawamura Y. Responses of Pseudomonas aeruginosa to antimicrobials. Front Microbiol. 2014;4:422. http://dx.doi.org/10.3389/fmicb.2013.00422.
Lin KY, Lauderdale TL, Wang JT, Chang SC. Carbapenem-resistant Pseudomonas aeruginosa in Taiwan: Prevalence, risk factors, and impact on outcome of infections. J Microbiol Immunol Infect. 2014. http://dx.doi.org/10.1016/j.jmii.2014.01.005.
Talpaert MJ, Gopal RG, Cooper BS, Wade P. Impact of guidelines and enhanced antibiotic stewardship on reducing broad-spectrum antibiotic usage and its effect on incidence of Clostridium difficile infection. J Antimicrob Chemother. 2011;66:2168-74. http://dx.doi.org/10.1093/jac/dkr253.
Leekha S, Terrell L, Edson RS. General principles of antimicrobial therapy. Mayo Clin Proc. 2011;86:156-67. http://dx.doi.org/10.4065/mcp.2010.0639.
Swartz MN. Impact of antimicrobial agents and chemotherapy from 1972 to 1998. Antimicrob Agents Chemother. 2000;44:2009-16. http://dx.doi.org/10.1128/AAC.44.8.2009-2016.2000.
Zaloga GP. Parenteral nutrition in adult inpatients with functioning gastrointestinal tracts: Assessment of outcomes. Lancet. 2006;367:1101-11. http://dx.doi.org/10.1016/S0140-6736(06)68307-4.
Turpin RS, Canada T, Rosenthal V, Nitzki-George D, Liu FX, Mercaldi CJ. Bloodstream infections associated with parenteral nutrition preparation methods in the United States: A retrospective, large database analysis. J Parenter Enteral Nutr. 2012;36:169-76. http://dx.doi.org/10.1177/0148607111414714.
Heuer JG, Sharma GR, Zhang T, Ding C, Bailey DL, Stephens EJ, et al. Effects of hyperglycemia and insulin therapy on outcome in a hyperglycemic septic model of critical illness. J Trauma. 2006;60:865-72. http://dx.doi.org/10.1097/01.ta.0000215565.29846.ab.
Dissanaike S, Shelton M, Warner K, O'Keefe GE. The risk for bloodstream infections is associated with increased parenteral caloric intake in patients receiving parenteral nutrition. Crit Care. 2007;11:R114. http://dx.doi.org/10.1186/cc6167.
Turpin RS, Canada T, Rosenthal V, Nitzki-George D, Liu FX, Mercaldi CJ. Bloodstream infections associated with parenteral nutrition preparation methods in the United States: A retrospective, large database analysis. J Parenter Enteral Nutr. 2012;36:169-76. http://dx.doi.org/10.1177/0148607111414714.
Tuon F, Gortz L, Rocha J. Risk factors for pan-resistant Pseudomonas aeruginosa bacteriemia and the adequacy of antibiotic therapy. Braz J Infect Dis. 2012;16:351-6. http://dx.doi.org/10.1016/j.bjid.2012.06.009.
González AL, Leal AL, Cortés JA, Sánchez R, Barrero LI, Castillo JS, et al. Effect of adequate initial antimicrobial therapy on mortality in critical patients with Pseudomonas aeruginosa bacteriemia. Biomédica. 2014;34(Suppl.1):58-66. http://dx.doi.org/10.7705/biomedica.v34i0.1691.
Some similar items:
- Karen Melissa Ordóñez, Odismar Andrea Hernández, Jorge Alberto Cortés, María José López, Gladys Alfonso, Alejandro Junca, Left-sided infective endocarditis caused by Pseudomonas aeruginosa treated medically , Biomedica: Vol. 30 No. 2 (2010)
- Andrés Leonardo González, Aura Lucía Leal, Jorge Alberto Cortés, Ricardo Sánchez, Liliana Isabel Barrero, Juan Sebastián Castillo, Carlos Arturo Álvarez, Effect of adequate initial antimicrobial therapy on mortality in critical patients with Pseudomonas aeruginosa bacteremia , Biomedica: Vol. 34 (2014): Abril, Suplemento 1, Resistencia bacteriana
- Sandra Yamile Saavedra, Carolina Duarte, María Nilse González, María Elena Realpe, Characterization of isolates of carbapenemase-producing Pseudomonas aeruginosa from seven Colombian provinces , Biomedica: Vol. 34 (2014): Abril, Suplemento 1, Resistencia bacteriana
- Natalia Andrea Maldonado, María Isabel Múnera, Jaime Alberto López, Patricia Sierra, Carlos Robledo, Jaime Robledo, Grupo GERMEN, Trends in antibiotic resistance in Medellín and municipalities of the Metropolitan Area between 2007 and 2012: Results of six years of surveillance , Biomedica: Vol. 34 No. 3 (2014)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























