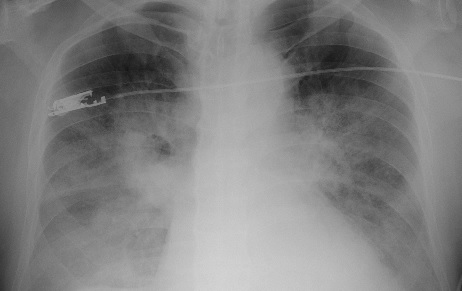
Severe hypoxemic respiratory failure caused by Pneumocystis jirovecii in a late kidney transplant recipient
Abstract
Pneumonia caused by Pneumocystis jirovecii is an uncommon infection in kidney transplant patients that can have an acute and rapid progression to respiratory failure and death. The period of greatest risk occurs in the first six months after the transplant, and it relates to the high doses of immunosuppression drugs required by patients. However, it may occur late, associated with the suspension of prophylaxis with trimethoprim-sulfamethoxazole.
We present two cases of renal transplant patients who had severe hypoxemic respiratory failure due to P. jirovecii six years after transplantation. In addition to steroids, they received treatment with trimethoprim-sulfamethoxazole. One patient died, while the other had clinical recovery, with preservation of the renal graft function.
Downloads
References
Ribes JA, Limper AH, Espy MJ, Smith TF. PCR detection of Pneumocystis carinii in bronchoalveolar lavage specimens: Analysis of sensitivity and specificity. J Clin Microbiol. 1997;35:830-5.
Thomas CF, Limper AH. Pneumocystis pneumonia. N Engl J Med. 2004;350:2487-98. https://doi.org/10.1056/NEJMra032588
Mulpuru S, Knoll G, Weir C, Desjardins M, Johnson D, Gorn L, et al. Pneumocystis pneumonia outbreak among renal transplant recipients at a North American transplant center: Risk factors and implications for infection control. Am J Infect Control. 2016;44;425-31. https://doi.org/10.1016/j.ajic.2015.11.012
Iriart X, Challan Belval T, Fillaux J, Esposito L, Lavergne RA, Cardeau-Desangles I, et al. Risk factors of Pneumocystis pneumonia in solid organ recipients in the era of the common use of posttransplantation prophylaxis.Am J Transplant. 2015;15:190-9. https://doi.org/10.1111/ajt.12947
Pareja JG, Garland R, Koziel H. Use of adjunctive corticosteroids in severe adult non-HIV Pneumocystis carinii pneumonia. Chest. 1998;113:1215-24. https://doi.org/10. 1378/chest.113.5.1215
Lemiale V, Debrumetz A, Delannoy A, Alberti C, Azoulay E. Adjunctive steroid in HIV-negative patients with severe Pneumocystis pneumonia. Respir Res. 2013;14:87. https://doi.org/10.1186/1465-9921-14-87
Moon SM, Kim T, Sung H, Kim MN, Kim SH, Choi SH, et al. Outcomes of moderate-to-severe Pneumocystis pneumonia treated with adjunctive steroid in non-HIV-infected patients. Antimicrob Agents Chemother. 2011;55:4613-8. https://doi.org/10.1128/AAC.00669-11
Anand S, Samaniego M, Kaul D. Pneumocystis jirovecii pneumonia is rare in renal transplant recipients receiving only one month of prophylaxis. TransplInfect Dis. 2011;13(6):570-4. https://doi.org/10.1111/j.1399-3062.2011.00692.x
Borstnar S, Lindic J, Tomazic J, Kandus A, Pikelj A, Prah J, et al. Pneumocystis jirovecii pneumonia in renal transplant recipients: A national center experience. Transplant Proc. 2013;45(4):1614-7. https://doi.org/10.1016/j.transproceed. 2013.02.107
Struijk GH, Gijsen AF, Yong SL, Zwinderman AH, Geerlings SE, Lettinga KD, et al. Risk of Pneumocystis jiroveci pneumonia in patients long after renal trans-plantation. Nephrol Dial Transplant. 2011;26:3391-8. https://doi.org/10.1093/ndt/gfr048
Gabardi S, Millen P, Hurwitz S, Martin S, Roberts K, Chandraker A. Atovaquone versus trimethoprimsulfamethoxazole as neumocystis jirovecii pneumonia prophylaxis following renal transplantation. Clin Transplant. 2012;26:E184-90. https://doi.org/10.1111/j.1399-0012.2012.01624.x
Tu GW, Ju MJ, Xu M, Rong RM, He YZ, Xue ZG, et al. Combination of caspofungin and low-dose trimethoprim/sulfamethoxazole for the treatment of severe Pneumocystis jirovecii pneumonia in renal transplant recipients. Nephrology (Carlton). 2013;18:736-42. https://doi.org/10.1111/nep.12133
Some similar items:
- Melissa Andrea Ortiz , Cristiam Mauricio Álvarez , Ana María Arrunátegui , Yazmin Rocío Arias , Adriana Villegas , Immunological follow-up of patients with renal transplants: A proposal for clinical practice in Colombia , Biomedica: Vol. 40 No. 3 (2020)
- Karen Melissa Ordóñez, Odismar Andrea Hernández, Jorge Alberto Cortés, María José López, Gladys Alfonso, Alejandro Junca, Left-sided infective endocarditis caused by Pseudomonas aeruginosa treated medically , Biomedica: Vol. 30 No. 2 (2010)
- Jairo Lizarazo, Melva Linares, Catalina de Bedout, Ángela Restrepo, Clara Inés Agudelo, Elizabeth Castañeda, Grupo Colombiano para el Estudio de la Criptococosis, Results of nine years of the clinical and epidemiological survey on cryptococcosis in Colombia, 1997-2005 , Biomedica: Vol. 27 No. 1 (2007)
- Jhon Carlos Castaño, Fidel Ángel Núñez, María Mercedes González, Germán Téllez, María Isabel Giraldo, First case report of Mammomonogamus (Syngamus) laryngeus human infection in Colombia , Biomedica: Vol. 26 No. 3 (2006)
- Álvaro J. Ruiz, Pablo J. Aschner, María Fernanda Puerta, Rafael Alfonso-Cristancho, IDEA Study (International Day for the Evaluation of Abdominal Obesity): Primary care study of the prevalence of abdominal obesity and associated risk factors in Colombia , Biomedica: Vol. 32 No. 4 (2012)
- Andrés Leonardo González, Aura Lucía Leal, Jorge Alberto Cortés, Ricardo Sánchez, Liliana Isabel Barrero, Juan Sebastián Castillo, Carlos Arturo Álvarez, Effect of adequate initial antimicrobial therapy on mortality in critical patients with Pseudomonas aeruginosa bacteremia , Biomedica: Vol. 34 (2014): Abril, Suplemento 1, Resistencia bacteriana
- Doris Cardona, Ángela María Segura, Adriana Espinosa, Alejandra Segura, Homicide and suicide in 15 to 24 year-old people in Colombia, 1998-2008 , Biomedica: Vol. 33 No. 4 (2013)
- Ricardo Pineda-Tamayo, Giovanna Arcila, Patricia Restrepo, Juan Manuel Anaya, Impact of cardiovascular illness on hospitalization costs in patients with rheumatoid arthritis. , Biomedica: Vol. 24 No. 4 (2004)
- Myriam Janeth Salazar, Ligia Inés Moncada, Life cycle of Culex quinquefasciatus Say (Diptera: Culicidae) under uncontrolled conditions. , Biomedica: Vol. 24 No. 4 (2004)
- Angela María Segura, Juan José Rey, María Patricia Arbelaéz, Trends of tuberculosis related mortality and hospital discharges before and after the implementation of the health sector reform, Colombia, 1985-1999. , Biomedica: Vol. 24 (2004): Suplemento 1
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























