Full-term low birth weight and its relationship with the socioeconomic conditions of municipalities in Antioquia: Spatio-temporal analysis
Abstract
Introduction: Low birth weight is one of the main health predictors for childhood and adulthood. It is highly prevalent in developing countries and in children from poorer social classes.
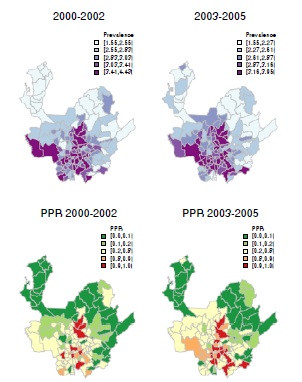
Objective: To analyze the geographical distribution and the trends of full-term low birth weight in the 125 municipalities of the department of Antioquia and their association with the socioeconomic conditions of the municipalities between 2000 and 2014.
Materials and methods: We conducted a longitudinal ecological study. The dependent variable was the prevalence of full-term low birth weight in 125 municipalities. The socioeconomic conditions of the municipalities were evaluated using the Human Development Index and the unsatisfied basic needs index.
Results: Between 2000 and 2014, the prevalence of full-term low birth weight in Antioquia was 2.7 per 100 live births; this prevalence decreased steadily over time. This trend was also observed between regions, with the exception of the Occidente and Urabá regions, which showed increases of approximately 20.0%. The results also showed a reduction in geographical differences between the 125 municipalities, with the coefficient of variation decreasing from 20.6% to 13.72% over the 14-year
period. Finally, we found a positive social gradient between the full-term low birth weight prevalence and the level of development in the municipalities.
Conclusion: Full-term low birth weight prevalence decreased between 2000 and 2014, with some regions showing greater reductions than others. Paradoxically, less developed and poorer areas had a lower prevalence, which may be a result of underreporting of birth weight information in these municipalities.
Downloads
References
Rojas EG, Mamani Y, Choque M del C, Abu-khdeir MA, Bustamante D. Bajo peso al nacer y sus factores asociados en el Hospital Materno infantil Germán Urquidi. Cochabamba, Bolivia. Gaceta Médica Boliviana. 2015;38:24-7.
World Health Organization, Expert Group on Prematurity. Expert Group on Prematurity: Final report. Technical Report Series No. 27. Geneva: World Health Organization; 1950.
Martínez R, Fernández A. Desnutrición infantil en América Latina y el Caribe. Desafíos. 2006;2:4-9.
Wardlaw T, Blanc A, Zupan J, Åhman E. Low birthweight: Country, regional and global estimates. The United Nations Children’s Fund and World Health Organization; 2004. Accessed: October 15, 2017. Available from: https://www.unicef.org/publications/index_24840.html.
Ramírez P. Informe final del evento bajo peso al nacer a término, Colombia, 2015. Final Report. Bogotá: Instituto Nacional de Salud; 2014.
Programa de las Naciones Unidas para el Desarrollo (PNUD). Antioquia - Retos y prioridades del departamento 2016 - 2019. Medellín; 2016. Accessed: October 5, 2017. Available from: http://www.co.undp.org/content/colombia/es/home/library/democratic_governance/retos-yprioridades-del-departamento-2016---20190.html
Baños L. Factores de riesgo asociados al bajo peso al nacer. Rev Cub Salud Pública. 2012;38:238-45.
Coronel C, Rivera I. Peso bajo al nacer. Su influencia en la salud durante el primer año de vida. Rev Mex Pediatr. 2003;70:283-7.
Equipo de Vigilancia Nutricional. Protocolo de vigilancia en salud pública, bajo peso al nacer a término. Bogotá: Instituto Nacional de Salud; 2016.
Schempf A, Strobino D, O’Campo P. Neighborhood effects on birthweight: An exploration of psychosocial and behavioral pathways in Baltimore, 1995-1996. Soc Sci Med. 2009;68:100-10. https://doi.org/10.1016/j.socscimed.2008.10.006
English PB, Kharrazi M, Davies S, Scalf R, Waller L, Neutra R. Changes in the spatial pattern of low birth weight in a southern California county: The role of individual and neighborhood level factors. Soc Sci Med. 2003;56:2073-88. https://doi.org/10.1016/S0277-9536(02)00202-2
Järvelin MR, Elliott P, Kleinschmidt I, Martuzzi M, Grundy C, Hartikainen AL, et al. Ecological and individual predictors of birthweight in a northern Finland birth cohort 1986. Paediatr Perinat Epidemiol. 1997;11:298-312. https://doi.org/10.1111/j.1365-3016.1997.tb00007.x
Brooks-Gunn J, McCormick MC, Klebanov PK, McCarton C. Health care use of 3-year-old low birth weight premature children: Effects of family and neighborhood poverty. J Pediatr. 1998;132:971-5. https://doi.org/10.1016/S0022-3476(98)70393-2
Coley SL, Nichols TR, Rulison KL, Aronson RE, Brown-Jeffy SL, Morrison SD. Does neighborhood risk explain racial disparities in low birth weight among infants born to adolescent mothers? J Pediatr Adolesc Gynecol. 2016;29:122-9. https://doi.org/10.1016/j.jpag.2015.08.004
Nkansah-Amankra S, Luchok KJ, Hussey JR, Watkins K, Liu X. Effects of maternal stress on low birth weight and preterm birth outcomes across neighborhoods of South Carolina, 2000-2003. Matern Child Health J. 2010;14:215-26. https://doi.org/10.1007/s10995-009-0447-4
Farley TA, Mason K, Rice J, Habel JD, Scribner R, Cohen DA. The relationship between the neighbourhood environment and adverse birth outcomes. Paediatr Perinat Epidemiol. 2006;20:188-200. https://doi.org/10.1111/j.1365-3016.2006.00719.x
Masi CM, Hawkley LC, Piotrowski ZH, Pickett KE. Neighborhood economic disadvantage, violent crime, group density, and pregnancy outcomes in a diverse, urban population. Soc Sci Med. 2007;65:2440-57. https://doi.org/10.1016/j.socscimed.2007.07.014
Departamento Administrativo Nacional de Estadística (DANE). Proyecciones nacionales y departamentales de población 2005-2020. Bogotá: Departamento Administrativo Nacional de Estadística; 2009. Accessed: October 16, 2017. Available from: https://www.dane.gov.co/files/investigaciones/poblacion/proyepobla06_20/7Proyecciones_poblacion.pdf
Barceló MA, Saez M, Cano-Serral G, Martínez-Beneito MÁ, Martínez JM, Borrell C, et al. Métodos para la suavización de indicadores de mortalidad: aplicación al análisis de desigualdades en mortalidad en ciudades del Estado español (Proyecto MEDEA). Gac Sanit. 2008;22:596-608.
Besag J, York J, Mollié A. Bayesian image restoration, with two applications in spatial statistics. Ann Inst Stat Math. 1991;43:1-20. https://doi.org/10.1007/BF00116466
Gelman A. Prior distributions for variance parameters in hierarchical models (comment on article by Browne and Draper). Bayesian Anal. 2006;1:515-34. https://doi.org/10.1214/06-BA117A
Rue H, Martino S, Lindgren F, Simpson D, Riebler A, Krainski E. INLA: Functions which allow to perform full Bayesian analysis of latent Gaussian models using Integrated Nested Laplace Approximation. 2014. https://www.researchgate.net/publication/271196512_INLA_Functions_Which_Allow_to_Perform_Full_Bayesian_Analysis_of_Latent_Gaussian_Models_Using_Integrated_Nested_Laplace_Approximaxion
Silva AA, Bettiol H, Barbieri MA, Pereira MM, Brito LG, Ribeiro VS, et al. Why are the low birthweight rates in Brazil higher in richer than in poorer municipalities? Exploring the epidemiological paradox of low birthweight. Paediatr Perinat Epidemiol. 2005;19:43-9. https://doi.org/10.1111/j.1365-3016.2004.00624.x
Juárez S, Ploubidis GB, Clarke L. Revisiting the “Low Birth Weight paradox” using a model-based definition. Gac Sanit. 2014;28:160-2. https://doi.org/10.1016/j.gaceta.2013.08.001
Flores M, Manuck T, Simonsen SE, Dyer J, Turok D. 557:The “Latina epidemiologic paradox” in Utah: Examining risk factors for low birth weight (LBW), preterm birth (PTB), and small-for-gestational-age (SGA) in Latina and White populations. Am J Obstet Gynecol. 2009;201:S207. https://doi.org/10.1016/j.ajog.2009.10.422
Fleuriet J, Sunil T. The Latina birth weight paradox: The role of subjective social status. J Racial Ethn Health Disparities. 2017. https://doi.org/10.1007/s40615-017-0419-0
Donoso E, Donoso A, Villarroel del PL. Mortalidad perinatal e infantil y el bajo peso al nacer en Chile y Cuba en el periodo 1991-2001. Rev Chil Obstet Ginecol. 2004;69:203-8. https://doi.org/10.4067/S0717-75262004000300004
Programa para la Reducción del Bajo Peso al Nacer. La Habana; 1998. Accessed: October 15, 2017. Available from: http://www.sld.cu/galerias/pdf/sitios/centromed/bajo_peso.pdf
Pinzón G, Vargas JE, Márquez MF, Quiroga EF. Análisis del bajo peso al nacer en Colombia 2005-2009. Rev Salud Pública. 2013;15:577-88.
Fondo de las Naciones Unidas para la Infancia. Progreso para la Infancia. Final Report. Report No. 6. New York:UNICEF; 2006.
Some similar items:
- Roxanna Uribe-Quintero , Luz Stella Álvarez-Castaño-Castaño, Beatriz Caicedo-Velásquez, Isabel, Trends in undernutrition mortality among children under five years of age and adults over 60 , Biomedica: Vol. 42 No. 1 (2022)
- Javier H. Eslava-Schmalbach, Carlos Javier Rincón, Carol Cristina Guarnizo, Life expectancy at birth in Colombia, 2000-2009: inequalities by region and gender , Biomedica: Vol. 33 No. 3 (2013)
- Silvia González, Olga L. Sarmiento, Óscar Lozano, Andrea Ramírez, Carlos Grijalba, Physical activity levels among Colombian adults: Inequalities by gender and socioeconomic status , Biomedica: Vol. 34 No. 3 (2014)
- Eduardo Bustos-Vázquez, Julián Alfredo Fernández-Niño, Claudia Iveth Astudillo-Garcia, Self-rated health, multimorbidity and depression in Mexican older adults: Proposal and evaluation of a simple conceptual model , Biomedica: Vol. 37 No. Sup.1 (2017): Suplemento 1, Alteraciones del sistema nervioso
- Laura Cabezas, Wilson Cabanzo, Fernando Santa, Victor Alberto Olano, Diana Sarmiento, Sandra Vargas, Juan Felipe Jaramillo, Thor-Axel Stenstrom, Hans J. Overgaard, María Inés Matiz, Spatial distribution of Aedes aegypti (Diptera: Culicidae) in the rural area of two municipalities of Cundinamarca, Colombia , Biomedica: Vol. 37 No. Sup. 2 (2017): Suplemento 2, Entomología médica, 2017
- Daniel Elías Cuartas, Genny Martínez, Diana María Caicedo, Jhonny Garcés, Yoseth Ariza-Araujo, Miguel Peña, Fabián Mendéz, Spatial distribution of potential and positive Aedes aegypti breeding sites , Biomedica: Vol. 37 No. Sup. 2 (2017): Suplemento 2, Entomología médica, 2017
- Jaime Badel-Mogollón, Laura Rodríguez-Figueroa, Gabriel Parra-Henao, Spatio-temporal analysis of the biophysical and ecological conditions of Triatoma dimidiata (Hemiptera: Reduviidae: Triatominae) in the northeast region of Colombia , Biomedica: Vol. 37 No. Sup. 2 (2017): Suplemento 2, Entomología médica, 2017
- Carmen Lucía Curcio, Andrés Fernando Giraldo, Fernando Gómez, The healthy aging phenotype in older people in Manizales , Biomedica: Vol. 40 No. 1 (2020)
- Diana Marcela Campo-Portacio, Luisa Fernanda Guerrero-Velásquez, Angie Patricia Castillo-García , Kelly Orozco-Méndez , Pedro José Blanco-Tuirán , Detection of Toxoplasma gondii in water for human consumption from water wells (jagüeyes) in the rural area of the municipality of Sincelejo , Biomedica: Vol. 41 No. Supl. 1 (2021): Mayo, Parasitología médica
- Javier Torres-Muñoz , Daniel Alberto Cedeño, Jennifer Murillo, Sofía Torres-Figueroa, Julián Torres-Figueroa, Sociodemographic determinants and mortality of premature newborns in a medium and low-income population in Colombia, 2017-2019 , Biomedica: Vol. 43 No. 3 (2023)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























