Inequalities on mortality due to acute respiratory infection in children: A Colombian analysis
Abstract
Introduction: Acute respiratory infections (ARI) are a leading public health issue worldwide.
Objective: To explore the inequalities in ARI mortality rates in under-5, according to socioeconomic characteristics.
Materials and methods: We conducted an ecological analysis to study inequalities at municipal level due to ARI mortality in children under 5 years. The data were obtained from official death records of the Departamento Administrativo Nacional de Estadística. The analysis of inequalities in the under-5 mortality rate (U5MR) included: 1) Classification of the population in different socio-economic strata, and 2) measurement of the degree of inequality. We used the ARI-U5MR as an outcome measurement.
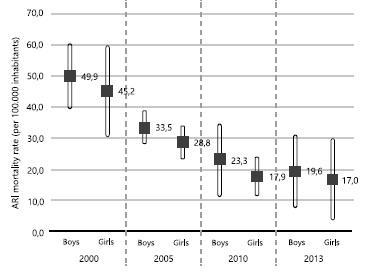
The mortality rates were estimated at national and municipal levels for the years 2000, 2005, 2010, and 2013. Rate ratios, rates differences, and concentration curves were calculated to observe the inequalities.
Results: A total of 18,012 children under 5 years died by ARI in Colombia from 2000 to 2013. ARIU5MR was greater in boys than in girls. During this period, an increase in the infant mortality relative gap in both boys and girls was observed. In 2013, the U5MR evidenced that for boys from municipalities with the highest poverty had a 1.6-fold risk to die than those in municipalities with the lowest poverty (low tercile). In girls, the ARI-U5MR for 2005 and 2013 in the poorest tercile was 1.5 and 2 times greater than in the first tercile, respectively.
Conclusion: Colombian inequalities in the ARI mortality rate among the poorest municipalities compared to the richest ones continue to be a major challenge in public health.
Downloads
References
Ahmad OB, López AD, Inoue M. The decline in child mortality: A reappraisal. Bull World Health Organ. 2000;78:1175-91.
Williams BG, Gouws E, Boschi-Pinto C, Bryce J, Dye C. Estimates of world-wide distribution of child deaths from acute respiratory infections. Lancet Infect Dis. 2002;2:25-32. https://doi.org/10.1016/S1473-3099(01)00170-0
Nair H, Nokes DJ, Gessner BD, Dherani M, Madhi SA, Singleton RJ, et al. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: A systematic review and meta-analysis. Lancet. 2010;375:1545-55. https://doi.org/10.1016/S0140-6736(10)60206-1
World Health Organization. Acute respiratory infections in children: Case management in small hospitals in developing countries. A manual for doctors and other Senior Heath Workers. Geneva: WHO; 1994.
Anders KL, Nguyen HL, Nguyen NM, van Thuy NT, Hong Van NT, Hieu NT, et al. Epidemiology and virology of acute respiratory infections during the first year of life: A birth cohort study in Vietnam. Pediatr Infect Dis J. 2015;34:361-70. https://doi.org/10.1097/INF.0000000000000643
GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1459-544. https://doi.org/10.1016/S0140-6736(16)31012-1
Instituto Nacional de Salud. Infección Respiratoria Aguda (IRA). Protocolo de Vigilancia en Salud Pública. Versión 05. 2016. Accessed on: October 3, 2016. Available from: http://www.ins.gov.co/lineas-de-accion/Subdireccion-Vigilancia/sivigila/Protocolos SIVIGILA/PRO Infeccion RespiratoriaAguda IRA.pdf
Álvarez-Castelló M, Castro-Almarales R, Abdo-Rodríguez A, Orta-Hernández SD, Gómez-Martínez M, Álvarez-Castelló M del P. Infecciones respiratorias altas recurrentes: algunas consideraciones. Rev Cuba Med Gen Integr. 2008;24.
Alvis-Zakzuk N, Paternina-Caicedo Á, Carrasquilla-Sotomayor M, De La Hoz-Restrepo F, Alvis-Guzmán N. Desigualdades de mortalidad infantil y pobreza en Colombia: análisis inter-censal (1993 y 2005). Revista Ciencias Biomédicas. 2015;6:29-37.
Departamento Administrativo Nacional de Estadística - DANE. Estimación de mortalidad infantil 2015. Accessed on: June 2, 2016. Available from: http://www.dane.gov.co/files/investigaciones/poblacion/vitales/Pres_TMI_DCD_2013.pdf
Instituto Nacional de Salud. Informe final del evento infección respiratoria aguda, Colombia 2015. Accessed on: October 28, 2016. Available from: http://www.ins.gov.co/lineas-de-accion/Subdireccion-Vigilancia/Informe de Evento Epidemiolgico/IRA 2015.pdf
World Bank. World Development Indicators. World Develop ment Indicators. Washington, D.C.: World Bank Group; 2017.
Waldmann RJ. Income distribution and infant mortality. Q J Econ. 1992;107:1283-302.
Wagstaff A, van Doorslaer E. Income inequality and health: What does the literature tell us? Annu Rev Public Health. 2000;21:543-67. https://doi.org/10.1146/annurev.publhealth.21.1.543
Subramanian SV, Kawachi I. Income inequality and health: What have we learned so far? Epidemiol Rev. 2004;26:78-91. https://doi.org/10.1093/epirev/mxh003
Wagstaff A. Desigualdades socioeconómicas y mortalidad infantil: comparación de nueve países en desarrollo. Boletín de la Organización Mundial de la Salud. 2000;3:18-28.
Arik H, Arik M. Is it economic growth or socioeconomic development?: A cross-sectional analysis of the determinants of infant mortality. J Dev Areas. 2009;42:31-55.
Departamento Administrativo Nacional de Estadística - DANE. Codificación de la división político-administrativa de Colombia (Divipola). 2016. Accessed on: July 18, 2016. Available from: http://geoportal.dane.gov.co:8084/Divipola/
Banco de la República. PIB. Metodología año base 2005| Banco de la República (Banco Central de Colombia). Accessed on: July 18, 2016. Available from: http://www.banrep.gov.co/es/pib 20. Departamento Administrativo Nacional de Estadística - DANE. Pobreza y condiciones de vida. Cifras departamentales de pobreza monetaria y desigualdad. Accessed on: July 18, 2016. Available from: https://www.google.com.co/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=0ahUKEwiyjuHDrP3NAhWGpB4KHYC0AyAQFggaMAA&url=http%3A%2F%2Fwww.dane.gov.co%2Ffiles%2Finvestigaciones%2Fcondiciones_vida%2Fpobreza%2Fanexos_pobreza_departamentos_2012.xls&usg=AFQjCNGXV-D
Departamento Administrativo Nacional de Estadística - DANE. Estadísticas vitales. Nacimientos y defunciones. Accessed on: July 18, 2016. Available from: http://www.dane.gov.co/index.php/poblacion-y-registros-vitales/nacimientos-y-defunciones/nacimientos-y-defunciones
Departamento Administrativo Nacional de Estadística - DANE. Estadísticas por tema. Demografía y población. Accessed on: October 3, 2016. Available from: http://www.dane.gov.co/index.php/estadisticas-por-tema/demografiay-poblacion
Departamento Administrativo Nacional de Estadística - DANE. Necesidades básicas insatisfechas (NBI). 2016. Accessed on: October 3, 2016. Available from: https://www.dane.gov.co/index.php/estadisticas-por-tema/pobreza-ycondiciones-de-vida/necesidades-basicas-insatisfechasnbi
Departamento Administrativo Nacional de Estadística - DANE. Pobreza monetaria y multidimensional en Colombia 2015. Accessed on: October 3, 2016. Available from: http://www.dane.gov.co/files/investigaciones/condiciones_vida/pobreza/bol_pobreza_15_.pdf
Zere E, Tumusiime P, Walker O, Kirigia J, Mwikisa C, Mbeeli T. Inequities in utilization of maternal health interventions in Namibia: Implications for progress towards MDG 5 targets. Int J Equity Health. 2010;9:1. https://doi.org/10.1186/1475-9276-9-16
Zere E, Kirigia JM, Duale S, Akazili J. Inequities in maternal and child health outcomes and interventions in Ghana. BMC Public Health. 2012;12:1. https://doi.org/10.1186/1471-2458-12-252
Mackenbach JP, Kunst AE. Measuring the magnitude of socio-economic inequalities in health: An overview of available measures illustrated with two examples from Europe. Soc Sci Med. 1997;44:757-71. https://doi.org/10.1016/S0277-9536(96)00073-1
Schneider MC, Castillo-Salgado C, Bacallao J, Loyola E, Mujica OJ, Vidaurre M, et al. Métodos de medición de las desigualdades de salud. Rev Panam Salud Pública. 2002;12:398-414. https://doi.org/10.1590/S1020-49892002001200006
Organización Panamericana de la Salud. Manual para el monitoreo de las desigualdades en salud, con especial énfasis en países de ingresos medianos y bajos. Washington, D.C.: OPS; 2016.
Wagstaff A, Paci P, van Doorslaer E. On the measurement of inequalities in health. Soc Sci Med. 1991;33:545-57. https://doi.org/10.1016/0277-9536(91)90212-U
Organisation for Economic Co-operation and Development - OECD. OECD Factbook 2011–2012: Economic, environmental and social statistics. Paris Organ Econ Co-operation Dev. 2011;1:268. https://doi.org/10.1787/factbook-2015-en
Khadka KB, Lieberman LS, Giedraitis V, Bhatta L, Pan dey G. The socio-economic determinants of infant mortality in Nepal: Analysis of Nepal Demographic Health Survey, 2011. BMC Pediatr. 2015;15:152. https://doi.org/10.1186/s12887-015-0468-7
Ministerio de la Protección Social. Plan Nacional de Salud Pública. Bogotá, D.C.: Ministerio de la Protección Social; 2007.
Castañeda-Orjuela C, Alvis-Guzmán N, Velandia-González M, De la Hoz-Restrepo F. Cost-effectiveness of pneumococcal conjugate vaccines of 7, 10, and 13 valences in Colombian children. Vaccine. 2012;30:1936-43. https://doi.org/10.1016/j.vaccine.2012.01.031
Álvis-Guzmán N, De la Hoz F. Cost effectiveness of heptavalent pneumococcal conjugate vaccine in populations of high risk in Colombia. Colomb Med. 2010;41:315-22.
Guzmán NA, De la Hoz-Restrepo F, Consuelo DV. The cost-effectiveness of Haemophilus influenzae type b vaccine for children under 2 years of age in Colombia. Rev Panam Salud Pública. 2006;20:248-55.
Balsara SL, Faerber JA, Spinner NB, Feudtner C, Tatter D. Pediatric mortality in males versus females in the United States, 1999-2008. Pediatrics. 2013;132:631-8. https://doi.org/10.1542/peds.2013-0339
Ministerio de Salud y Protección Social. Plan Decenal de Salud Pública, PDSP, 2012 - 2021. 2013. Accessed on: July 18, 2016. Available from: https://www.minsalud.gov.co/Documentos%20y%20Publicaciones/Plan%20Decenal%20-%20Documento%20en%20consulta%20para%20aprobaci%C3%B3n.pdf
Szwarcwald CL, Bastos FI, Andrade CLT de. Medidas de desigualdad en salud: la discusión de algunos aspectos metodológicos con una aplicación para la mortalidad neonatal en el Municipio de Rio de Janeiro, 2000. Cad Saúde Pública. 2002;18:959-70. https://doi.org/10.1590/S0102-311X2002000400005
Frenz P, González C. Aplicación de una aproximación metodológica simple para el análisis de las desigualdades: el caso de la mortalidad infantil en Chile. Rev Med Chil. 2010;138:1157-64. https://doi.org/10.4067/S0034-98872010000900012
Barros FC, Matijasevich A, Requejo JH, Giugliani E, Maranhao AG, Monteiro CA, et al. Recent trends in maternal, newborn, and child health in Brazil: Progress toward Millennium Development Goals 4 and 5. Am J Public Health. 2010;100:1877-89. https://doi.org/10.2105/AJPH.2010.196816
McKinnon B, Harper S, Kaufman JS, Bergevin Y. Socioeconomic inequality in neonatal mortality in countries of low and middle income: A multicountry analysis. Lancet Glob Health.2014;2:165-73. https://doi.org/10.1016/S2214-109X(14)70008-7
Chaparro-Narváez P, León-Quevedo W, Castañeda-Orjuela CA. Comportamiento de la mortalidad por dengue en Colombia entre 1985 y 2012. Biomédica. 2016;36:125-34. https://doi.org/10.7705/biomedica.v36i0.3009
Departamento Administrativo Nacional de Estadística - DANE. Nota metodológica. Cambio de la mortalidad infantil en la línea base 2005. 2012 Accessed on: October 13, 2016. Available from: https://www.dane.gov.co/files/investigaciones/poblacion/vitales/nota_metodologica.pdf
Sedgwick P. Understanding the ecological fallacy. BMJ. 2015;351:h4773. https://doi.org/10.1136/bmj.h4773
Some similar items:
- Rosa Magdalena Uscátegui, Adriana María Correa, Nutritional status of children with malaria in northwest Colombia , Biomedica: Vol. 27 No. 4 (2007)
- Hollman Miller, Gerzaín Rodríguez, Tungiasis in native Amerindians in Vaupés province: epidemiology, clinical aspects, treatment, and prevention , Biomedica: Vol. 30 No. 2 (2010)
- Guillermo Sánchez, Carlos Gustavo Niño, Carolina Estupiñán, Factors associated with the timely treatment of women with breast cancer supported by a non-governmental organization in Bogotá, Colombia , Biomedica: Vol. 35 No. 4 (2015)
- David Andrés Espinal, Isabel Cristina Hurtado, Ana Eugenia Arango, Josefina García, V. Alberto Laguna-Torres, Sergio Jaramillo, Human metapneumovirus in children: first cases in Colombia , Biomedica: Vol. 32 No. 2 (2012)
- Ana Cecilia Aguilar, Alberto Pradilla, Mildrey Mosquera, Ana Beatriz Gracia, José Guillermo Ortega, Jaime Humberto Leiva, Robinson Ramírez-Vélez, Percentile values for physical condition for Cali, Colombian children and adolescents , Biomedica: Vol. 31 No. 2 (2011)
- Ángela Liliana Londoño-Franco, Juliana Loaiza-Herrera, Fabiana María Lora-Suárez, Jorge Enrique Gómez-Marín, Blastocystis sp. frequency and sources among children from 0 to 5 years of age attending public day care centers in Calarcá, Colombia , Biomedica: Vol. 34 No. 2 (2014)
- Astrid Berena Herrera, Laura A. Rodríguez, Jürg Niederbacher, Biological pollution and its relationship with respiratory symptoms indicative of asthma, Bucaramanga, Colombia , Biomedica: Vol. 31 No. 3 (2011)
- Jairo Echeverry, Carlos Mauricio Hurtado, Myriam Gutiérrez, Clinical manifestations of lead levels in children exposed to automobile battery recycling processes in Soacha and Bogotá, D.C. , Biomedica: Vol. 28 No. 1 (2008)
- Rosa Magdalena Uscátegui, Adriana M. Correa, Jaime Carmona-Fonseca, Changes in retinol, hemoglobin and ferritin concentrations in Colombian children with malaria , Biomedica: Vol. 29 No. 2 (2009)
- Elpidia Poveda, Diana Giraldo, Yibby Forero, Carlos Mendivil, Self-reported physical activity in comparison with anthropometric body fat indicators in school children , Biomedica: Vol. 28 No. 3 (2008)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























