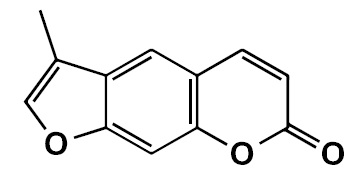
Coumarin analogue 3-methyl-7H-furo[3,2-g] chromen-7-one as a possible antiparkinsonian agent
Abstract
Introduction: Parkinson’s disease is the second most common neurodegenerative disease. Monoamine oxidase B inhibitors are used in the treatment of this disease concomitantly with levodopa or as monotherapy. Several substituted coumarins have shown activity as inhibitors of monoamine oxidase B.
Objective: To evaluate the possible antiparkinsonian effects of the coumarin analogue FCS005 (3-methyl-7H-furo[3,2-g]chromen-7-one) in mouse models, as well as its inhibitory activity towards monoamine oxidases (MAO) and its antioxidant activity.
Materials and methods: FCS005 was synthesized and the reversal of hypokinesia was evaluated in the reserpine and levodopa models. Moreover, in the haloperidol model, its anticataleptic effects were evaluated. Additionally, the monoamine oxidase inhibitory activity and antioxidant activity of FCS005 were evaluated using in vitro and ex vivo studies, respectively.
Results: FCS005 (100 mg/kg) caused the reversal of hypokinesia in the reserpine and levodopa models. This furocoumarin also presented anti-cataleptic effects at the same dose. Besides, it showed selective inhibitory activity towards the MAO-B isoform and antioxidant activity.
Conclusion: These results attribute interesting properties to the compound FCS005. It is important to continue research on this molecule considering that it could be a potential antiparkinsonian agent.
Downloads
References
Elbaz A, Carcaillon L, Kab S, Moisan F. Epidemiology of Parkinson’s disease. Rev Neurol (Paris). 2016;172:14-26. https://doi.org/10.1016/j.neurol.2015.09.012
Dorsey ER, Constantinescu R, Thompson JP, Biglan KM, Holloway RG, Kieburtz K, et al. Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology. 2007;68:384-6. https://doi.org/10.1212/01.wnl.0000247740.47667.03
Connolly BS, Lang AE. Pharmacological treatment of Parkinson disease: A review. JAMA. 2014; 311:1670-83. https://doi.org/10.1001/jama.2014.3654
Alexi T, Borlongan C, Faull R, Williams C, Clark R, Gluckman P, et al. Neuroprotective strategies for basal ganglia degeneration: Parkinson’s and Huntington’s diseases. Prog Neurobiol. 2000;60:409-70. https://doi.org/10.1016/S0301-0082(99)00032-5
Emborg M. Evaluation of animal models of Parkinson’s disease for neuroprotective strategies. J Neurosci Methods. 2004;139:121-43. https://doi.org/10.1016/j.jneumeth.2004.08.004
Gershanik OS. Improving L-dopa therapy: The development of enzyme inhibitors. Mov Disord. 2015;30:103-13. https://doi.org/10.1002/mds.26050
Finberg J. Update on the pharmacology of selective inhibitors of MAO-A and MAO-B; focus on modulation of CNS monoamine neurotransmitter release. Pharmacol Ther. 2014;143:133-52. https://doi.org/10.1016/j.pharmthera.2014.02.010
Ariza S, Rueda D, Rincón J, Linares E, Guerrero M. Efectos farmacológicos sobre el sistema nervioso central inducidos por cumarina aislada de Hygrophila tyttha Leonard. Vitae. 2007;14:51-8.
Vergel N, López J, Orallo F, Viña D, Buitrago D, Olmo E, et al. Antidepressant-like profile and MAO-A inhibitory activity of 4-propyl-2H-benzo[h]- chromen-2-one. Life Sci. 2010;86:819-24. https://doi.org/10.1016/j.lfs.2010.04.001
Matos M, Viña D, Picciau C, Orallo F, Santana L, Uriarte E. Synthesis and evaluation of 6-methyl-3-phenylcoumarins as potent and selective MAO-B inhibitors. Bioorg Med Chem Lett. 2009;19:5053-5. https://doi.org/10.1016/j.bmcl.2009.07.039
Matos M, Viña D, Quezada E, Picciau C, Delogu G, Orallo F, et al. A new series of 3-phenylcoumarins as potent and selective MAO-B inhibitors. Bioorg Med Chem Lett. 2009;19:3268-70. https://doi.org/10.1016/j.bmcl.2009.04.085
Matos M, Viña D, Janeiro P, Borges F, Santana L, Uriarte E. New halogenated 3-phenylcoumarins as potent and selective MAO-B inhibitors. Bioorg Med Chem Lett. 2010;20:5157-60. https://doi.org/10.1016/j.bmcl.2010.07.013
Matos M, Viña D, Vázquez-Rodríguez S, Uriarte E, Santana L. Focusing on new monoamine oxidase inhibitors: Differently substituted coumarins as an interesting scaffold. Curr Top Med Chem. 2012;12:2210-39. https://doi.org/10.2174/1568026611212200008
Matos M, Vilar S, González-Franco R, Uriarte E, Santana L, Friedman C, et al. Novel (coumarin-3-yl) carbamates as selective MAO-B inhibitors: Synthesis, in vitro and in vivo assays, theoretical evaluation of ADME properties and docking study. Eur J Med Chem. 2013;63:151-61. https://doi.org/10.1016/j.ejmech.2013.02.009
Pisani L, Farina R, Nicolotti O, Gadaleta D, Soto-Otero R, Catto M, et al. In silico design of novel 2H-chromen-2-one derivatives as potent and selective MAO-B inhibitors. Eur J Med Chem. 2015;89:98-105. https://doi.org/10.1016/j.ejmech.2014.10.029
Epifano F, Molinaro G, Genovese S, Ngomba R, Nicoletti F, Curini M. Neuroprotective effect of prenyloxycoumarins from edible vegetables. Neurosci Lett. 2008;443:57-60. https://doi.org/10.1016/j.neulet.2008.07.062
Liu WB, Zhou J, Qu Y, Li X, Lu CT, Xie KL, et al. Neuroprotective effect of osthole on MPP+-induced cytotoxicity in PC12 cells via inhibition of mitochondrial dysfunction and ROS production. Neurochem Int. 2010;57:203-15. https://doi.org/10.1016/j.neuint.2010.05.011
Philippens I. Non-human primate models for Parkinson’s disease. Drug Discov Today Dis Models. 2008;5:105-11. https://doi.org/10.1016/j.ddmod.2008.06.004
Matos M, Rodríguez F, Borges F, Santana L, Uriarte E, Estrada M, et al. 3-Amidocoumarins as potential multifunctional agents against neurodegenerative diseases. Chem Med Chem. 2015;10:2071-9. https://doi.org/10.1002/cmdc.201500408
Aguirre P, García O, Tapia V, Muñoz Y, Cassels BK, Núñez MT. Neuroprotective effect of a new 7,8-dihydroxycoumarin-based Fe2+/Cu2+ chelator in cell and animal models of Parkinson’s disease. ACS Chem Neurosci. 2017;8:178-85. https://doi.org/10.1021/acschemneuro.6b00309
Reglodi D, Renaud J, Tamas A, Tizabi Y, Socías SB, Del-Bel E, et al. Novel tactics for neuroprotection in Parkinson’s disease: Role of antibiotics, polyphenols and neuropeptides. Prog Neurobiol. 2017;155:120-48. https://doi.org/10.1016/j.pneurobio.2015.10.004
Garazd M, Garazd Y, Ogorodniichuk A, Khilya V. Modified coumarins. Synthesis of substituted 5-(4-methoxyphenyl)-7H-furo [3,2-g] chromen-7-ones. Chem Nat Compd. 2002;38:539-48. https://doi.org/10.1023/A:1022626402415
National Center for Biotechnology Information. PubChem Open Chemistry Database Compound Summary for CID 608273. Accessed on: January 20, 2018. Available at: https://pubchem.ncbi.nlm.nih.gov/compound/608273
Tadaiesky M, Andreatini R, Vital M. Different effects of 7-nitroindazole in reserpine-induced hypolocomotion in two strains of mice. Eur J Pharmacol. 2006;535:199-207. https://doi.org/10.1016/j.ejphar.2006.02.004
Schmidt W, Mayerhofer A, Meyer A, Kovar K. Ecstasy counteracts catalepsy in rats, an antiparkinsonian effect? Neurosci Lett. 2002;330:251-4.
Wei L, Chen L. Effects of 5-HT in globus pallidus on haloperidol-induced catalepsy in rats. Neurosci Lett. 2009;454:49-52. https://doi.org/10.1016/j.neulet.2009.02.053
Hijova E, Nistiar F, Sipulova A. Changes in ascorbic acid and malondialdehyde in rats after exposure to mercury. Bratis Lek Listy. 2005;106:248-51.
Levine R, Garland D, Oliver C, Amici A, Climent I, Lenz A, et al. Determination of carbonyl content in oxidatively modified proteins. Methods Enzymol. 1990;186:464-78. https://doi.org/10.1016/0076-6879(90)86141-H
Baltacioglu E, Akalin FA, Alver A, Deger O, Karabulut E. Protein carbonyl levels in serum and gingival crevicular fluid in patients with chronic periodontitis. Arch Oral Biol. 2008;53:716-22. https://doi.org/10.1016/j.archoralbio.2008.02.002
Yáñez M, Fraiz N, Cano E, Orallo F. Inhibitory effects of cis- and trans-resveratrol on noradrenaline and 5-hydroxytryptamine uptake and on monoamine oxidase activity. Biochem Biophys Res Commun. 2006;344:688-95. https://doi.org/10.1016/j.bbrc.2006.03.190
Colpaert F. Pharmacological characteristics of tremor, rigidity and hypokinesia induced by reserpine in rats. Neuropharmacology. 1987;26:1431-40.
Kaur S, Starr M. Antiparkinsonian action of dextramethorphan in the reserpine-treated mouse. Eur J Pharmacol. 1995;280:159-66.
Menzaghi F, Whelan K, Risbrough V, Rao T, Lloyd G. Interactions between a novel cholinergic ion channel agonist, SIB-1765F and L-DOPA in the reserpine model of Parkinson’s disease in rats. J. Pharmacol Exp Ther. 1997;280:393-401.
Foley P, Gerlach M, Youdim M, Riederer P. MAO-B inhibitors: Multiple roles in the therapy of neurodegenerative disorders? Parkinsonism Relat Disord. 2000;6;25-47. https://doi.org/10.1016/S1353-8020(99)00043-7
Fernández H, Chen J. Monoamine oxidase-B inhibition in the treatment of Parkinson’s disease. Pharmacotherapy. 2007;27:174S-85S. https://doi.org/10.1592/phco.27.12part2.174S
Fisher A, Biggs C, Eradiri O, Starr M. Dual effects of L-3,4-dihydroxyphenylalanine on aromatic L-amino acid decarboxylase, dopamine release and motor stimulation in the reserpine-treated rat: Evidence that behavior is dopamine independent. Neuroscience. 2000;95:97-111. https://doi.org/10.1016/S0306-4522(99)00406-6
Haleem DJ, Inam QU, Haleem MA. Effects of clinically relevant doses of methyphenidate on spatial memory, behavioral sensitization and open field habituation: A time related study. Behav Brain Res. 2015;281:208-14. https://doi.org/10.1016/j.bbr.2014.12.031
Deacon RM, Koros E, Bornemann KD, Rawlins JN. Aged Tg2576 mice are impaired on social memory and open field habituation tests. Behav Brain Res. 2009;197:466-8. https://doi.org/10.1016/j.bbr.2008.09.042
Wang X, Han C, Xu Y, Wu K, Chen S, Hu M, et al. Synthesis and evaluation of phenylxanthine derivatives as potential dual A2AR antagonists/MAO-B inhibitors for Parkinson’s disease. Molecules. 2017;22:1-13. https://doi.org/10.3390/molecules22061010
Duty S, Jenner P. Animal models of Parkinson´s disease: A source of novel treatments and clues to the cause of the disease. Br J Pharmacol. 2011;164:1357-91. https://doi.org/10.1111/j.1476-5381.2011.01426.x
Bishnoi M, Chopra K, Kulkarni S. Involvement of adenosinergic receptor system in an animal model of tardive dyskinesia and associated behavioural, biochemical and neurochemical changes. Eur J Pharmacol. 2006;552:55-66. https://doi.org/10.1016/j.ejphar.2006.09.010
Bishnoi M, Chopra K, Kulkarni S. Possible anti-oxidant and neuroprotective mechanisms of zolpidem in attenuating typical anti-psychotic-induced orofacial dyskinesia -A biochemical and neurochemical study. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:1130-8. https://doi.org/10.1016/j.pnpbp.2007.04.007
Martins M, Petronilho F, Gomes K, Dai-Pizzol F, Streck E, Quevedo J. Antipsychotic induced oxidative stress in rat brain. Neurotox Res. 2008;13:63-9. https://doi.org/10.1007/BF03033368
Naidu P, Singh A, Kulkarni S. Quercetin, a bioflavonoid attenuated haloperidol induced orofacial dyskinesia. Neuropharmacology. 2003;44:1100-6. https://doi.org/10.1016/S0028-3908(03)00101-1
Singh A, Naidu P, Kulkarni S. Possible antioxidant and neuroprotective mechanisms of FK506 in attenuating haloperidol-induced orofacial dyskinesia. Eur J Pharmacol. 2003;477:87-94. https://doi.org/10.1016/S0014-2999(03)02124-1
Pavshintsev VV, Podshivalova LS, Frolova OY, Belopolskaya OA, Averina OA, Kushnir EA, et al. Effects of mitochondrial antioxidant SkQ1 on biochemical and behavioural parameters in a Parkinsonism model in mice. Biochemistry (Mosc). 2003;82:1513-20. https://doi.org/10.1134/S0006297917120100
Molina-Jiménez M F, Sánchez-Reus M I, Benedi J. Effect of fraxetin and myricetin on rotenone-induced cytotoxicity in SH-SY5Y cells: Comparison with N-acetylcysteine. Eur J Pharmacol. 2003;472:81-7. https://doi.org/10.1016/S0014-2999(03)01902-2
Kong LD, Tan RX, Woo AY, Cheng CH. Inhibition of rat brain monoamine oxidase activities by psoralen and isopsoralen: Implications for the treatment of affective disorders. Pharmacol Toxicol. 2001;88:75-80.
Some similar items:
- Edisson Rodríguez, Aura María Gil-Villa, Daniel Camilo Aguirre-Acevedo, Walter Cardona-Maya, Ángela P. Cadavid, Evaluation of atypical semen parameters in individuals whose couples had a history of early recurrent embryo death: in search for a reference value , Biomedica: Vol. 31 No. 1 (2011)
- Jorge E. Machado-Alba, Cristhian David Morales-Plaza, Antipsychotic prescription patterns in patients affiliated to the Social Security Health System in Colombia , Biomedica: Vol. 33 No. 3 (2013)
- Manuela Velásquez, Manuel Alejandro Granada, Juan Camilo Galvis, Ángela María Álvarez, Ángela Cadavid, Oxidative stress in endothelial cells induced by the serum of women with different clinical manifestations of the antiphospholipid syndrome , Biomedica: Vol. 39 No. 4 (2019)
- Nayanna de Oliveira Ramos Melo, Hélio De Sousa Peres Júnior, Clara Araujo Diniz , Matheus De Sousa Silva, Telma L.G. Lemos, Francisco Vagnaldo Fechine Jamacaru, Conceição Aparecida Dornelas, Red propolis reduces inflammation in cyclophosphamide-induced hemorrhagic cystitis in rats , Biomedica: Vol. 42 No. 2 (2022)
- Laura V. Suárez-Patiño, Andrés Orozco-Duque , Estefanía Pérez-Giraldo , Sebastián Roldán-Vasco, Juan Camilo Suárez-Escudero , Lillyana Martínez-Moreno , Synchronization between videofluoroscopic swallowing study and surface electromyography in patients with neurological involvement presenting symptoms of dysphagia , Biomedica: Vol. 42 No. 4 (2022)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























