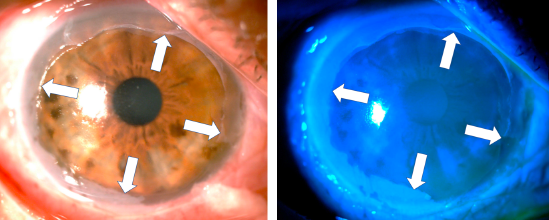
Severe corneal burn due to the accidental application of salicylic acid packed in a plastic dropper bottle
Abstract
Eye burns due to the accidental application of pharmacological or nonpharmacological substances packaged in plastic dropper bottles have been described for more than three decades and continue to occur. These burns can cause potentially serious corneal injuries.
We report the case of a patient who mistakenly applied salicylic acid to the right eye after confusing it with an eye lubricant, which caused him a severe corneal burn. Fortunately, after aggressive medical and surgical management (including oxygen therapy and amniotic membrane grafting), the visual results were good.
We suggest conducting educational campaigns and taking legislative measures in our country to avoid packaging corrosive substances in this type of dropper bottle to reduce the risk of accidental burns.
Downloads
References
Galvis V, Díaz AL, Ochoa ME, Rey JJ, Ardila LC, Olivero LP, et al. Primary causes of emergency ophthalmological consultations at a tertiary care institution in Colombia. Med UNAB. 2019;22:162-70. https://doi.org/10.29375/01237047.3489
Gudas PP Jr. Ophthaine drug alert. Arch Ophthalmol. 1979;97:2211-2. https://doi.org/10.1001/archopht.1979.01020020517024
Ling RF, Villalobos R, Latina M. Inadvertent instillation of hemoccult developer in the eye: Case report. Arch Ophthalmol. 1988;106:1033-4. https://doi.org/10.1001/archopht.1988.01060140185013
Steinemann TL, Henry KE. Misuse of nonophthalmic and ophthalmic drops due to packaging similarity. Arch Ophthalmol. 1995;113:1578-9. https://doi.org/10.1001/archopht.1995.01100120110027
Wheeler J, Shah P. Minerva picture. BMJ. 2001;322:182.
Haylor V, Daines J. Olbas oil mistaken as eye drops. Letter. Pharm J. 2004;272:670.
Adams MK, Sparrow JM, Jim S, Tole DM. Inadvertent administration of Olbas oil into the eye: A surprisingly frequent presentation. Eye (Lond). 2009;23:244. https://doi.org/10.1038/eye.2008.70
Shazly TA. Ocular acid burn due to 20% concentrated salicylic acid. Cutan Ocul Toxicol. 2011;30:84-6. https://doi.org/10.3109/15569527.2010.521536
Brown JA. Medicinal mishap. Incorrectly dropped in the eye. Australian Prescriber. 2013;36:56-7. https://doi.org/10.18773/austprescr.2013.026
Jamison A, Lockington D. Ocular chemical injury secondary to electronic cigarette liquid misuse. JAMA Ophthalmol. 2016;134:1443. https://doi.org/10.1001/jamaophthalmol.2016.3651
Johnson TV, Pandit RR, Weinberg RS. Ocular chemical burns secondary to unintentional instillation of aqua regia hobbyist reagent: Not all that glitters is gold. JAMA Ophthalmol. 2017;135:673-5. https://doi.org/10.1001/jamaophthalmol.2017.0924
Jinagal J, Gupta PC, Gupta G, Sahu KK, Ram J. Ocular chemical burns from accidental exposure to topical dermatological medicinal agent. Indian J Ophthalmol. 2018;66:1476-7. https://doi.org/10.4103/ijo.IJO_365_18
Parker RT, McCall DP, Samarawickrama C. Eye injury from toxic chemical mistaken for eye drops. Med J Aust. 2018;208:369. https://doi.org/10.5694/mja17.00979
Ma KN, Thanos A, Chodosh J, Shah AS, Mantagos IS. A novel technique for amniotic membrane transplantation in patients with acute Stevens-Johnson syndrome. Ocul Surf. 2016;14:31-6. https://doi.org/10.1016/j.jtos.2015.07.002
Sharifipour F, Baradaran-Rafii A, Idani E, Zamani M, Jabbarpoor-Bonyadi MH. Oxygen therapy for acute ocular chemical or thermal burns: A pilot study. Am J Ophthalmol. 2011;151:823-8. https://doi.org/10.1016/j.ajo.2010.11.005
Sharifipour F, Panahi-Bazaz M, Idani E, Hajizadeh M, Saki A. Oxygen therapy for corneal edema after cataract surgery. J Cataract Refract Surg. 2015;41:1370-5. https://doi.org/10.1016/j.jcrs.2014.10.033
Yanoff M, Sassani JW. Ocular Pathology. Eight edition. New York, USA: Elsevier; 2020. p. 155.
Bizrah M, Yusuf A, Ahmad S. An update on chemical eye burns. Eye (Lond). 2019;33:1362-77. https://doi.org/10.1038/s41433-019-0456-5
Sharma N, Kaur M, Agarwal T, Sangwan VS, Vajpayee RB. Treatment of acute ocular chemical burns. Surv Ophthalmol. 2018;63:214-35. https://doi.org/10.1016/j.survophthal.2017.09.005
Clare G, Suleman H, Bunce C, Dua H. Amniotic membrane transplantation for acute ocular burns. Cochrane Database Syst Rev. 2012;(9):CD009379. https://doi.org/10.1002/14651858.CD009379.pub2
American Academy of Ophthalmology. Color codes for topical ocular medications. Accessed on: 11 de noviembre de 2019. Available at: https://www.aao.org/about/policies/color-codestopical-ocular-medications
Fraunfelder FT. Drug-packaging standards for eye drop medications. Arch Ophthalmol. 1988;106:1029. https://doi.org/10.1001/archopht.1988.01060140181003
Cohen MR, Davis NM. How to prevent eye medication errors. Am Pharm. 1992;NS32:22-3. https://doi.org/10.1016/s0160-3450(15)31047-3
Some similar items:
- Claudia Blanco, María Ximena Núñez, Efficacy of Orbscan II® and Pentacam® topographers by a repeatability analysis when assessing elevation maps in candidates to refractive surgery , Biomedica: Vol. 29 No. 3 (2009)
- Katherine Rothstein, Jubby M. Gálvez, Ángela M. Gutiérrez, Laura Rico, Eveling Criollo, Alejandra de-la-Torre, Ocular findings in Fabry disease in Colombian patients , Biomedica: Vol. 39 No. 3 (2019)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























