SARS-CoV-2 and rhinovirus/enterovirus co-infection in a critically ill young adult patient in Colombia
Abstract
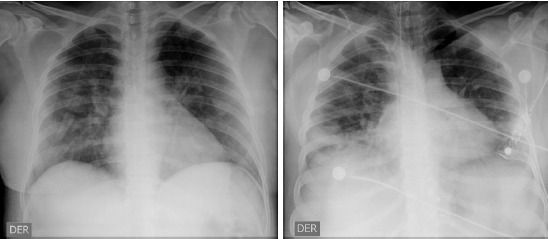
The current SARS-CoV-2 pandemic has caused a huge global public health problem. We report the case of a young adult patient with laboratory-confirmed SARS-CoV-2. We describe the identification of the virus and the clinical course, diagnosis, and treatment of the infection including her rapid clinical deterioration from the mild initial symptoms, which progressed to multilobar pneumonia requiring admission to the intensive care unit.
This case highlights the importance of establishing a diagnosis based on the clinical findings and the patient’s history bearing in mind the possibility of gastrointestinal symptoms in addition to respiratory ones. Besides, the presence of risk factors should be investigated; in this case, we proposed obesity as a possible risk factor. Furthermore, limitations in diagnostic tests and the possibility of co-infection with other respiratory pathogens are highlighted. We describe the imaging, laboratory findings, and treatment taking into account the limited current evidence.
Downloads
References
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708‐20. https://doi.org/10.1056/NEJMoa2002032
Ministerio de Salud y Protección Social. Nuevo coronavirus COVID-19. Fecha de consulta: 23 de abril del 2020. Disponible en: https://www.minsalud.gov.co/portada-covid-19.html
Livingston E, Bucher K. Coronavirus disease 2019 (COVID-19) in Italy. JAMA. 2020;323:1335. https://doi.org/10.1001/jama.2020.4344
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020;395:1054-62. https://doi.org/10.1016/S0140-6736(20)30566-3
Fauci AS, Lane HC, Redfield RR. Covid-19 — Navigating the uncharted. N Engl J Med. 2020;382:1268-9. https://doi.org/10.1056/NEJMe2002387
Young BE, Ong SWX, Kalimuddin S, Low JG, Tan SY, Loh J, et al. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA. 2020;323:1488-94. https://doi.org/10.1001/jama.2020.3204
Fineberg HV. Ten weeks to crush the curve. N Engl J Med. 2020 382:e37. https://doi.org/10.1056/NEJMe2007263
Tian Y, Rong L, Nian W, He Y. Gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther. 2020;51:843-51. https://doi.org/10.1111/apt.15731
Gane SB, Kelly C, Hopkins C. Isolated sudden onset anosmia in COVID-19 infection. A novel syndrome? Rhinology. 2020;58:289-94. https://doi.org/10.4193/Rhin20.114
Gu J, Han B, Wang J. COVID-19: Gastrointestinal manifestations and potential fecal-oral transmission. Gastroenterology. 2020;158:1518-19. https://doi.org/10.1053/j.gastro.2020.02.054
Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929-36. https://doi.org/10.1056/NEJMoa2001191
Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033-4. https://doi.org/10.1016/S0140-6736(20)30628-0
Tan L, Wang Q, Zhang D, Ding J, Huang Q, Tang Y-Q, et al. Lymphopenia predicts disease severity of COVID-19: A descriptive and predictive study. Signal Transduct Target Ther. 2020;5:33. https://doi.org/10.1038/s41392-020-0148-4
Lippi G, Wong J, Henry BM. Hypertension and its severity or mortality in coronavirus disease 2019 (COVID-19): A pooled analysis. Pol Arch Intern Med. 2020;130:304-9. https://doi.org/10.20452/pamw.15272
Ellulu MS, Patimah I, Khaza’ai H, Rahmat A, Abed Y. Obesity and inflammation: The linking mechanism and the complications. Arch Med Sci. 2017;13:851-63. https://doi.org/10.5114/aoms.2016.58928
Lippi G, Simundic AM, Plebani M. Potential preanalytical and analytical vulnerabilities in the laboratory diagnosis of coronavirus disease 2019 (COVID-19). Clin Chem Lab Med. 2020:20200285. https://doi.org/10.1515/cclm-2020-0285
Xiao AT, Tong YX, Zhang S. False-negative of RT-PCR and prolonged nucleic acid conversion in COVID-19: Rather than recurrence. J Med Virol. 2020. https://doi.org/10.1002/jmv.25855
Kim D, Quinn J, Pinsky B, Shah NH, Brown I. Rates of co-infection between SARS-CoV-2 and other respiratory pathogens. JAMA. 2020;e206266. https://doi.org/10.1001/jama.2020.6266
Ding Q, Lu P, Fan Y, Xia Y, Liu M. The clinical characteristics of pneumonia patients coinfected with 2019 novel coronavirus and influenza virus in Wuhan, China. J Med Virol. 2020;1-7. https://doi.org/10.1002/jmv.25781
Khodamoradi Z, Moghadami M, Lotfi M. Co-infection of coronavirus disease 2019 and influenza A: A report from Iran. Arch Iran Med. 2020;23:239-43. https://doi.org/10.34172/aim.2020.04
Prompetchara E, Ketloy C, Palaga T. Immune responses in COVID-19 and potential vaccines: Lessons learned from SARS and MERS epidemic. Asian Pac J Allergy Immunol. 2020;38:1-9. https://doi.org/10.12932/AP-200220-0772
Dong L, Hu S, Gao J. Discovering drugs to treat coronavirus disease 2019 (COVID-19). Drug Discov Ther. 2020;14:58-60. https://doi.org/10.5582/ddt.2020.01012
Cortegiani A, Ingoglia G, Ippolito M, Giarratano A, Einav S. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J Crit Care. 2020. https://doi.org/10.1016/j.jcrc.2020.03.005
Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, Mailhe M, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: Results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020. https://doi.org/10.1016/j.ijantimicag.2020.105949
Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, Sevestre J, et al. Clinical and microbiological effect of a combination of hydroxychloroquine and azithromycin in 80 COVID-19 patients with at least a six-day follow up: A pilot observational study. Travel Med Infect Dis. 2020. https://doi.org/10.1016/j.tmaid.2020.101663
Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, et al. A trial of lopinavir–ritonavir in adults hospitalized with severe Covid-19. N Engl J Med. 2020;382:1787-99. https://doi.org/10.1056/NEJMoa2001282
Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, Fan E, et al. Surviving sepsis campaign: Guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Intensive Care Med. 2020. https://doi.org/10.1007/s00134-020-06022-5
Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID-19 virus targeting the cns:Tissue distribution, host-virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci. 2020;11:995-8. https://doi.org/10.1021/acschemneuro.0c00122
Saavedra-Trujillo CH, Gutiérrez A, Rodríguez-Morales A, Javier A, Mejía N, et al. Consenso colombiano de atención, diagnóstico y manejo de la infección por SARS-COV-2/COVID-19 en establecimientos de atención de la salud - Recomendaciones basadas en consenso de expertos e informadas en la evidencia. Infectio. 2020;24:1-102. https://doi.org/10.22354/in.v24i3.851
Some similar items:
- Luis Fernando Valladales-Restrepo , Camilo Alexander Constain-Mosquera , María Alejandra Hoyos-Guapacha , Karol Liceth Hoyos-Guapacha , Andrés Gaviria-Mendoza, Manuel Enrique Machado-Duque , Jorge Enrique Machado-Alba, Study of the indications for macrolide prescriptions in a Colombian population , Biomedica: Vol. 42 No. 2 (2022)
- Zulma M. Cucunubá, Latin American scientific research prorities for COVID-19 prevention and control , Biomedica: Vol. 40 No. Supl. 2 (2020): SARS-CoV-2 y COVID-19
- Enrique Gea-Izquierdo, Legionellosis in Spain, 2010-2015 , Biomedica: Vol. 41 No. 1 (2021)
- Luis Alberto Gómez, Editorial note about SARS-CoV-2 in the pandemic era , Biomedica: Vol. 40 No. Supl. 2 (2020): SARS-CoV-2 y COVID-19
- Jorge Alberto Cortés, Pilar Espitia, Yuliet Liliana Rosero-Lasso, Citywide preparedness for a pandemic: A crosssectional survey of knowledge, attitudes, and practices about respiratory infection prevention in Bogotá, Colombia , Biomedica: Vol. 40 No. Supl. 2 (2020): SARS-CoV-2 y COVID-19
- Fernando Bolaños, Leonardo F. Jurado, Rina L. Luna-Tavera, Jaime M. Jiménez, Abdominal angiostrongyliasis, report of two cases and analysis of published reports from Colombia , Biomedica: Vol. 40 No. 2 (2020)
- Alexandra Hurtado-Ortiz, José Moreno-Montoya , Franklyn E. Prieto-Alvarado , Álvaro J. Idrovo, Benchmarking of public health surveillance of COVID-19 in Colombia: First semester , Biomedica: Vol. 40 No. Supl. 2 (2020): SARS-CoV-2 y COVID-19
- Julián Alfredo Fernández-Niño , Andrés Cubillos-Novella, Ietza Bojórquez , Michael Rodríguez , Recommendations for the response against COVID-19 in migratory contexts under a closed border: The case of Colombia , Biomedica: Vol. 40 No. Supl. 2 (2020): SARS-CoV-2 y COVID-19
- José Y. Rodríguez, Carlos A. Álvarez-Moreno, Jorge A. Cortés, Gerson J. Rodríguez, Kelin Esquea, Heidy Pinzón, María J. Mendoza, Yiceth Acosta, Melioidosis in Colombia, description of a clinical case and epidemiological considerations , Biomedica: Vol. 39 No. Sp. 1 (2019): Suplemento 1, Microbiología médica, mayo
- Claudia Calderón, Rodolfo Dennis, Economic cost of Streptococcus pneumoniae community-acquired pneumonia, meningitis and bacteremia in an adult population that required hospitalization in Bogotá, Colombia , Biomedica: Vol. 34 No. 1 (2014)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























