Seroprevalence of arboviruses in Ecuador: Implications for improved surveillance
Abstract
Introduction: Arthropod-borne viruses (arboviruses) cause morbidity and mortality in humans and domestic animals worldwide. The percentage of population immunity or susceptibility to these viruses in Ecuador is unknown.
Objectives: To investigate the proportion of Ecuadorian populations with IgG antibodies (Abs) (past exposure/immunity) and IgM Abs (current exposure) against flaviviruses and alphaviruses and to study the activity of these viruses in Ecuador.
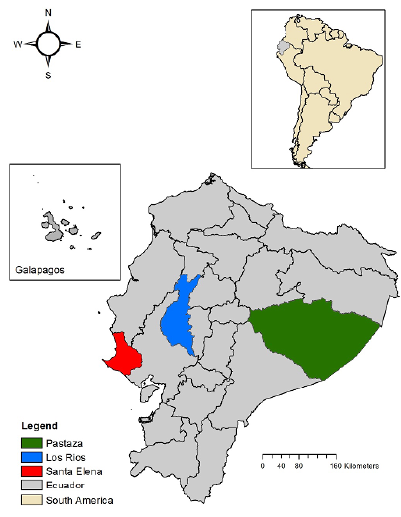
Materials and methods: During 2009-2011, we conducted a serosurvey for selected arboviruses in humans (n=1,842), equines (n=149), and sentinel hamsters (n=84) at two coastal locations and one in the Amazon basin (Eastern Ecuador) using enzyme-linked immunosorbent assay and hemagglutination inhibition test.
Results: From 20.63% to 63.61% of humans showed IgG-antibodies for the flaviviruses: Dengue virus (DENV), yellow fever virus (YFV) Saint Louis encephalitis virus, and West Nile virus (WNV); from 4.67% to 8.63% showed IgG-Abs for the alphaviruses: Venezuelan equine encephalitis virus, eastern equine encephalitis virus, and western equine encephalitis virus. IgM-Abs were found for DENV and WNV. Equines and hamsters showed antibodies to alphaviruses in all locations; two hamsters seroconverted to YFV in the Amazonia.
Conclusions: The results show a YFV vaccination history and suggest the activity of arboviruses not included in the current surveillance scheme. Enhanced arbovirus and mosquito surveillance, as well as continued YFV vaccination and evaluation of its coverage/effectiveness, are recommended.
Downloads
References
Gubler DJ, Vasilakis N. The Arboviruses: Quo Vadis? Norfolk: Caister Academic Press; 2016. p. 1-6. https://doi.org/10.21775/9781910190210.01
Wilder-Smith A, Gubler DJ, Weaver SC, Monath TP, Heymann DL, Scott TW. Epidemic arboviral diseases: Priorities for research and public health. Lancet Infect. Dis. 2017;17:e101-6. https//doi.org/10.1016/S1473-3099(16)30518-7
Karabatsos N. International catalogue of arboviruses, including certain other viruses of vertebrates. San Antonio, Tex.: American Society of Tropical Medicine and Hygiene for the Subcommittee on Information Exchange of the American Committee on Arthropod-borne Viruses; 1985.
Mayer SV, Tesh RB, Vasilakis N. The emergence of arthropod-borne viral diseases: A global prospective on dengue, chikungunya and zika fevers. Acta Trop. 2017;166:155-63. https//doi.org/10.1016/j.actatropica.2016.11.020
Borja Lavayen C. La fiebre amarilla. Apuntes sobre la epidemia de 1880. In: La fiebre amarilla y los médicos de Guayaquil. Quito: Banco Central del Ecuador; 1987. p. 11-81.
Alava AA, Mosquera C, Vargas W, Real J. Dengue en el Ecuador 1989-2002. Rev Ecuat Hig Med Trop. 2005;42:11-34.
Gutiérrez VE, Monath TP, Alava AA, Uriguen BD, Arzube RM, Chamberlain R. Epidemiologic investigations of the 1969 epidemic of Venezuelan encephalitis in Ecuador. Am J Epidemiol. 1975;102:400-13.
Dirección Nacional de Vigilancia Epidemiológica-MSP. Enfermedades transmitidas por vectores. Fiebre Chikungunya. Semana epidemiológica 52/2018. Accessed: August 15, 2020. Available from: https://www.salud.gob.ec/wp-content/uploads/2019/01/GACETA-VECTORES-SE-52.pdf
Dirección Nacional de Vigilancia Epidemiológica-MSP. Zika. Semana epidemiológica 52/2018. Accessed: August 15, 2020. Available from: https://www.salud.gob.ec/wp-content/uploads/2019/01/GACETA-VECTORES-SE-52.pdf
Monath TP. Yellow fever: An update. Lancet Infect Dis. 2001;1:11-20. https//doi.org/10.1016/S1473-3099(01)00016-0
Becerra L. Informe del Director de Sanidad Pública. N 195. Al Ministro de lo Interior y Sanidad. Guayaquil 27 de mayo. In: Guayaquil: 1740-1919 Crónica y reflexiones epidemiológicas sobre la fiebre amarilla en la ciudad. Guayaquil: Facultad de Ciencias Psicológicas, Universidad de Guayaquil; 2004. p. 165-6.
García E. La fiebre amarilla en Ecuador. Rev Ecuat Hig Med Trop. 1953;10:1-7.
Dirección Nacional de Vigilancia Epidemiológica-MSP. Enfermedades transmitidas por vectores Ecuador, SE 01- 27 - 2020. Accessed: August 16, 2020. Available from: https://www.salud.gob.ec/wp-content/uploads/2020/07/ETV-SE-27.pdf
Dirección Nacional de Vigilancia Epidemiológica-MSP. Enfermedades transmitidas por vectores. Dengue. SE01-31/2020. Accessed: August 15, 2020. Available from https://www.salud.gob.ec/wp-content/uploads/2020/08/Vectores-SE-31.pdf
Gutiérrez VE. Encefalitis venezolana en el Ecuador. Brote epizoodémico de 1972. Rev Ecuat Hig Med Trop. 1977;30:169-88.
Centers for Disease Control and Prevention (CDC). Venezuelan equine encephalitis. Arbovirus Catalog. Accessed: August 15, 2020. Available from: https://wwwn.cdc.gov/arbocat/VirusDetails.aspx?ID=507&SID=10
Young NA. Origin of epidemics of Venezuelan equine encephalitis. J Infect Dis. 1972;125:565-7.
Kinney RM, Tsuchiya KR, Sneider JM, Trent DW. Molecular evidence for the origin of the widespread Venezuelan equine encephalitis epizootic of 1969 to 1972. J Gen Virol. 1992;73:3301-5. https//doi.org/10.1099/0022-1317-73-12-3301
Weaver SC, Pfeffer M, Marriott K, Kang W, Kinney RM. Genetic evidence for the origins of Venezuelan equine encephalitis virus subtype IAB outbreaks. Am J Trop Med Hyg. 1999;60:441-8. https//doi.org/10.4269/ajtmh.1999.60.441
Calisher CH, Gutiérrez VE, Francy DB, Alava AA, Muth DJ, Lazuick JS. Identification of hitherto unrecognized arboviruses from Ecuador: Members of serogroups B, C, Bunyamwera, Patois, and Minatitlan. Am J Trop Med Hyg. 1983;32:877-85. https//doi.org/10.4269/ajtmh.1983.32.877
Coello R. Presencia del virus del Nilo occidental en equinos (Equus caballus) de doshumedales de la Provincia de los Ríos, año 2007 al 2009. Revista de la Universidad de Guayaquil. 2011;111:15-22.
Johnson BW, Cruz C, Felices V, Espinoza WR, Manock SR, Guevara C, et al. Ilheus virus isolate from a human, Ecuador. Emerg Infect Dis. 2007;13:956. https//doi.org/10.3201/eid1306.070118
Izurieta R, Macaluso M, Watts D, Tesh R, Guerra B, Cruz L, et al. Hunting in the rainforest and Mayaro virus infection: An emerging alphavirus in Ecuador. J Glob Infect Dis. 2011;3:317. ttps//doi.org/10.4103/0974-777x.91049
Wise EL, Pullan ST, Márquez S, Paz V, Mosquera JD, Zapata S, et al. Isolation of oropouche virus from febrile patient, Ecuador. Emerg Infect Dis. 2018;24:935. https//doi.org/10.3201/eid2405.171569
Manock SR, Jacobsen KH, De Bravo NB, Russell KL, Negrete M, Olson JG, et al. Etiology of acute undifferentiated febrile illness in the Amazon basin of Ecuador. Am J Trop Med Hyg. 2009;81:146-51.
World Organization for Animal Health-OIE. Encefalomielitis equina del este, Ecuador. 2013. Accessed: August 15, 2020. Available from: https://www.oie.int/wahis_2/public/wahid.php/Reviewreport/Review?page_refer=MapFullEventReport&reportid=13534&newlang=es
Groseth A, Vine V, Weisend C, Guevara C, Watts D, Russell B, et al. Maguari virus associated with human disease. Emerg Infect Dis. 2017;23:1325. https//doi.org/10.3201/eid2308.161254
Metcalf CJE, Farrar J, Cutts FT, Basta NE, Graham AL, Lessler J, et al. Use of serological surveys to generate key insights into the changing global landscape of infectious disease. Lancet. 2016;388:728-30. https//doi.org/10.1016/S0140-6736(16)30164-7
Beaty BJ, Calisher CH, Shope RE. Arboviruses. En: Lennette EH, Lennette DA, Lennette ET, editors. Diagnostic procedures for viral, rickettsial, and chlamydial infections. 7th edition. Washington: American Public Health Association 1995; p.189-212.
Sudia WD, Chamberlain RW. Battery-operated light trap, an improved model. Mosq News. 1962;22:126-9.
Johnson AJ, Martin DA, Karabatsos N, Roehrig JT. Detection of anti-arboviral immunoglobulin G by using a monoclonal antibody-based capture enzyme-linked immunosorbent assay. J Clin Microbiol. 2000;38:1827-31. https//doi.org/10.1128/JCM.38.5.1827-1831.2000
Casals J. Immunological techniques for animal viruses. In: Methods in virology. New York: Elsevier; 1967. p. 113-98. https://doi.org/10.1016/B978-1-4832-3219-5.50010-X
Instituto de Medicina Tropical Pedro Kouri. Técnicas de laboratorio para el diagnóstico y la caracterización de los virus del dengue. Habana: Instituto de Medicina Tropical “Pedro Kourí”; 2013.
Sudia WD, Lord RD, Hayes RO. Collection and processing of vertebrate specimens for arbovirus studies. Atlanta: US Department of Health, Education and Welfare; 1970. p. 28-46.
Ayers M, Adachi D, Johnson G, Andonova M, Drebot M, Tellier R. A single tube RT-PCR assay for the detection of mosquito-borne flaviviruses. J Virol Methods. 2006;135:235-9. https//doi.org/10.1016/j.jviromet.2006.03.009
Sánchez-Seco MP, Rosario D, Quiroz E, Guzmán G, Tenorio A. A generic nested-RT-PCR followed by sequencing for detection and identification of members of the alphavirus genus. J Virol Methods. 2001;95:153-61. https//doi.org/10.1016/S0166-0934(01)00306-8
Eastwood G, Goodman SJ, Hilgert N, Cruz M, Kramer LD, Cunningham AA. Using avian surveillance in Ecuador to assess the imminence of West Nile virus incursion to Galápagos. Ecohealth. 2014;11:53-62. https//doi.org/10.1007/s10393-014-0911-5
Guerra HL, Sardinha TM, da Rosa AP, Lima e Costa MF. Effectiveness of the yellow fever vaccine 17D: An epidemiologic evaluation in health services. Rev Panam Salud Pública. 1997;2:115-20.
Staples JE, Gershman M, Fischer M. Yellow fever vaccine: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2010:59;1-27.
World Health Organization. Ecuador: WHO and UNICEF estimates of immunization coverage: 2019 revision. Accessed: August 15, 2020. Available from: https://www.who.int/immunization/monitoring_surveillance/data/ecu.pdf
Shearer FM, Moyes CL, Pigott DM, Brady OJ, Marinho F, Deshpande A, et al. Global yellow fever vaccination coverage from 1970 to 2016: An adjusted retrospective analysis. Lancet Infect Dis. 2017;17:1209-17. https//doi.org/10.1016/S1473-3099(17)30419-X
Franck PT, Johnson KM. An outbreak of Venezuelan equine encephalomyelitis in Central America: Evidence for exogenous source of a virulent virus subtype. Am J Epidemiol. 1971;94:487-95. https//doi.org/10.1093/oxfordjournals.aje.a121346
Rico-Hesse R, Weaver SC, De Siger J, Medina G, Salas RA. Emergence of a new epidemic/epizootic Venezuelan equine encephalitis virus in South America. Proc Natl Acad Sci. 1995;92:5278-81. https//doi.org/10.1073/pnas.92.12.5278
Forrester NL, Wertheim JO, Dugan VG, Auguste AJ, Lin D, Adams AP, et al. Evolution and spread of Venezuelan equine encephalitis complex alphavirus in the Americas. PLoS Negl Trop Dis. 2017;11:e0005693. https//doi.org/10.1371/journal.pntd.0005693
Arrigo NC, Adams AP, Weaver SC. Evolutionary patterns of eastern equine encephalitis virus in North versus South America suggest ecological differences and taxonomic revision. J Virol. 2010;84:1014-25. https//doi.org/10.1128/JVI.01586-09
Carrera JP, Forrester N, Wang E, Vittor AY, Haddow AD, Loṕez-Vergès S, et al. Eastern equine encephalitis in Latin America. N Engl J Med. 2013;22;369:732-44. https//doi.org/10.1056/NEJMoa1212628
Espinal MA, Andrus JK, Jauregui B, Waterman SH, Morens DM, Santos JI, et al. Emerging and reemerging aedes-transmitted arbovirus infections in the region of the Americas: Implications for health policy. Am J Public Health. 2019;109:387-92. https//doi.org/10.2105/AJPH.2018.304849
Calisher CH, Blair CD, Bowen MD, Casals J, Drebot MA, Henchal EA, et al. Identification of arboviruses and certain rodent-borne viruses: Reevaluation of the paradigm. Emerg Infect Dis. 2001;7:756. https//doi.org/10.3201/eid0704.010431
Faria NR, Kraemer MU, Hill SC, De Jesus JG, Aguiar RS, Iani FC, et al. Genomic and epidemiological monitoring of yellow fever virus transmission potential. Science. 2018;361:894-9. https//doi.org/1126/science.aat7115
Holmes EC. RNA virus genomics: A world of possibilities. J Clin Invest. 2009;119:2488-95. https//doi.org/10.1172/JCI38050
Coffey LL, Page BL, Greninger AL, Herring BL, Russell RC, Doggett SL, et al. Enhanced arbovirus surveillance with deep sequencing: Identification of novel rhabdoviruses and bunyaviruses in Australian mosquitoes. Virology. 2014;448:146-58. https//doi.org/10.1016/j.virol.2013.09.026
Miranda JJ, Castro-Ávila AC, Salicrup LA. Advancing health through research partnerships in Latin America. BMJ. 2018;16;362:k2690. https//doi.org/10.1136/bmj.k2690
Some similar items:
- María Cristina Ferro, Victor Alberto Olano, Martha Ahumada, Scott Weaver, Mosquitos (Diptera: Culicidae) in the small village where a human case of Venezuelan equine encephalitis was recorded , Biomedica: Vol. 28 No. 2 (2008)
- Claudia M.E. Romero, Humberto Llinás, Andrew K.I. Falconar, Evaluation of a rapid water-surface sweeping method to curately estimate numbers of Aedes aegypti (Diptera: Culicidae) late larval stages in large water-storage containers: comparison with pupal estimates , Biomedica: Vol. 30 No. 2 (2010)
- Ángela María Segura, Doris Cardona, María Osley Garzón, Trends in yellow fever mortality in Colombia, 1998-2009 , Biomedica: Vol. 33 (2013): Suplemento 1, Fiebres hemorrágicas
- Raquel E. Ocazionez-Jiménez, Ayda Susana Ortiz-Báez, Sergio Yebrail Gómez-Rangel, Daniel R. Miranda-Esquivel, Dengue virus serotype 1 (DENV-1) from Colombia: its contribution to dengue occurrence in Santander , Biomedica: Vol. 33 (2013): Suplemento 1, Fiebres hemorrágicas
- María C. Méndez, Cristina Domingo, Antonio Tenorio, Lissethe C. Pardo, Gloria J. Rey, Jairo A. Méndez, Development of a reverse transcription polymerase chain reaction method for yellow fever virus detection , Biomedica: Vol. 33 (2013): Suplemento 1, Fiebres hemorrágicas
- Jairo A. Méndez, Gerzaín Rodríguez, María del Pilar Bernal, Dora de Calvache, Jorge Boshell, Molecular detection of yellow fever virus in human sera and mice brains. , Biomedica: Vol. 23 No. 2 (2003)
- Berlin Londoño-Rentería, Jenny C. Cárdenas, Jeniffer E. Giovanni, Lucio Cárdenas, Paloma Villamizar, Jenniffer Rolón, Daniel M. Chisenhall, Rebecca C. Christofferson, Daysi J. Carvajal, Omar G. Pérez, Dawn M. Wesson, Christopher N. Mores, Aedes aegypti anti-salivary gland antibody concentration and dengue virus exposure history in healthy individuals living in an endemic area in Colombia , Biomedica: Vol. 35 No. 4 (2015)
- Liliana Morales, Myriam L. Velandia, María Angélica Calderon, Jaime E. Castellanos, Jacqueline Chaparro-Olaya, Polyclonal antibodies against recombinant dengue virus NS3 protein , Biomedica: Vol. 37 No. 1 (2017)
- Mauricio Hernández, Diana Arboleda, Stephania Arce, Allan Benavides, Paola Andrea Tejada, Sindy Vanessa Ramírez, Ángela Cubides, Methodology to develop endemic channels and notification trends for dengue in Valle del Cauca, Colombia, 2009-2013 , Biomedica: Vol. 36 (2016): Suplemento 2, Enfermedades virales
- Juliana Pérez-Pérez, William H. Sanabria, Carolina Restrepo, Raúl Rojo, Enrique Henao, Omar Triana, Ana María Mejía, Sandra M. Castaño, Guillermo L. Rúa-Uribe, Virological surveillance of Aedes (Stegomyia) aegypti and Aedes (Stegomyia) albopictus as support for decision making for dengue control in Medellín , Biomedica: Vol. 37 No. Sup. 2 (2017): Suplemento 2, Entomología médica, 2017
Funding data
-
Secretaría de Educación Superior, Ciencia, Tecnología e Innovación
Grant numbers PIC-08-IZP-00002
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























