Prevalence of adverse events and their manifestations in health professionals as second victims
Abstract
Introduction: Adverse events can cause harm to the patient, but they also affect health professionals making them second victims of the event. Interventions have been focused mostly on patients, but little on professionals, probably due to lack of tools.
Objective: To estimate the prevalence of adverse events and describe their manifestations in healthcare personnel to evidence the phenomenon of second victims in a highly complex hospital.
Materials and methods: We conducted an analytical cross-sectional study by a survey of 419 healthcare professionals from the hospitalization, emergency, and surgical areas in a highly complex hospital in Medellín in 2019. The frequency of adverse events was estimated and its association with some labor and demographic variables was determined.
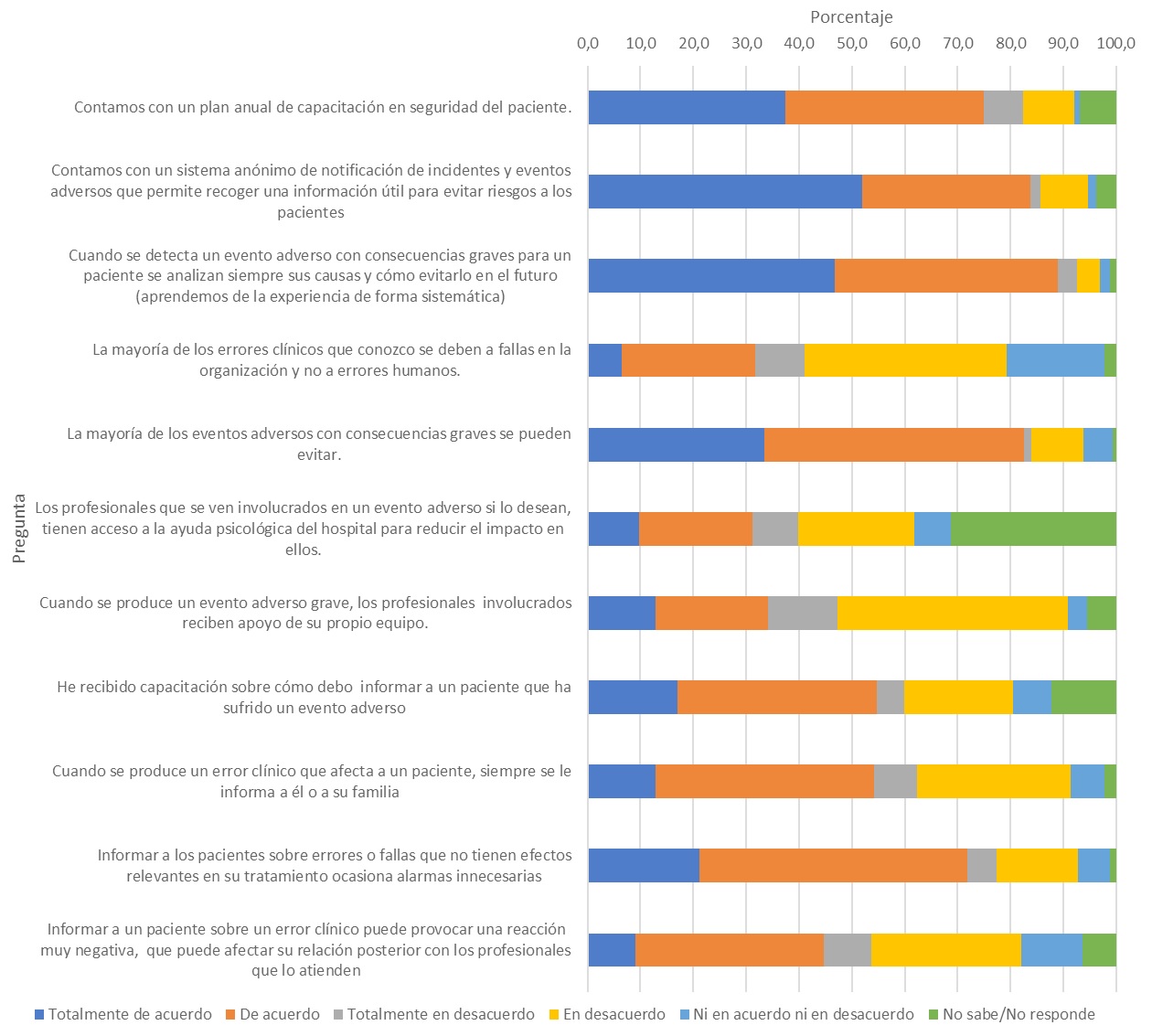
Results: We found that 93.1% of the participants knew of incident cases and 79% of serious adverse events while 44.4% had been involved in them and 99% of these had feelings as a second victim, mainly the difficulty to concentrate, guilt, fatigue, anxiety, and doubts about decisions; 95% indicated they wanted to receive training to face the consequences of adverse events and know how to inform the patient.
Conclusions: Health professionals are frequently exposed to adverse events that can cause negative emotions in them such as guilt, fatigue, anxiety, and insecurity. Most professionals who participate in an adverse event express feelings as a second victim. Informing the patient about an adverse event requires preparation and most professionals requested training on the subject.
Downloads
References
Ministerio de Salud y Protección Social de Colombia. Seguridad del paciente y la atención segura. Guía técnica «Buenas prácticas para la seguridad del paciente en la atención en salud». Fecha de consulta: 10 de agosto de 2019. Disponible en: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/CA/Guia-buenas-practicas-seguridad-paciente.pdf
Organización Mundial de la Salud. Marco conceptual de la clasificación internacional para la seguridad del paciente. Informe técnico definitivo, enero de 2009. Fecha de consulta: 11 de agosto de 2019. Disponible en: https://www.who.int/patientsafety/implementation/icps/icps_full_report_es.pdf
Ministerio de Salud y Protección Social. Resolución No. 3100 de 2019 por la cual se definen los procedimientos y condiciones de inscripción de los prestadores de servicios de salud y de habilitación de los servicios de salud y se adopta el Manual de Inscripción de Prestadores y Habilitación de Servicios de Salud. Bogotá: Minsalud; 2019.
Ministerio de Salud y Protección Social de Colombia. Decreto 1011 de 2006 por el cual se establece el Sistema Obligatorio de Garantía de Calidad de la Atención de Salud del Sistema General de Seguridad Social en Salud. Bogotá: Minsalud; 2006.
Ministerio de Salud y de la Protección Social de Colombia. Resolución 5095 de 2018, por el cual se adopta el “Manual de Acreditación en Salud Ambulatoria y Hospitalaria de Colombia, versión 3.1. Bogotá: Minsalud; 2018.
Organización Mundial de la Salud. 10 datos sobre seguridad del paciente. Fecha de consulta: 30 de agosto de 2019. Disponible en: https://www.who.int/features/factfiles/patient_safety/es/
Ministerio de Sanidad y Politica Social de España/OMS. Estudio IBEAS: Prevalencia de efectos adversos en hospitales de Latinoamérica. 2010. Fecha de consulta: 8 de julio de 2019. Disponible en: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/CA/resultados-estudio-ibeas.pdf
Parra CV, López JS, Bejarano CH, Puerto AH, Galeano ML. Eventos adversos en un hospital pediátrico de tercer nivel de Bogotá. Rev Fac Nac Salud Pública. 2017;35:286-92. https://doi.org/10.17533/udea.rfnsp.v35n2a12
Mira JJ, Carrillo I, Lorenzo S, Ferrús L, Silvestre C, Pérez-Pérez P, et al. The aftermath of adverse events in Spanish primary care and hospital health professionals. BMC Health Serv Res. 2015;15:1-9. https://doi.org/10.1186/s12913-015-0790-7
Han K, Bohnen JD, Peponis T, Martínez M, Nandan A, Yeh DD, et al. The surgeon as the second victim? Results of the Boston Intraoperative Adverse Events Surgeons’ Attitude (BISA ) study. J Am Coll Surg. 2017;224:1048-56. https://doi.org/10.1016/j.jamcollsurg.2016.12.039
Conway J, Federico F, Stewart K, Campbell M. Respectful management of serious clinical adverse events. Second edition. Cambridge, Massachusetts: Institute for Healthcare Improvement; 2011. Fecha de consulta: 20 de agosto de 2020. Disponible en: http://www.ihi.org/resources/Pages/IHIWhitePapers/RespectfulManagementSeriousClinicalAEsWhitePaper.aspx
Mira JJ, Lorenzo S. Las segundas víctimas de los incidentes para la seguridad de los pacientes. Rev Calid Asist. 2016;31:1-2. https://doi.org/10.1016/j.cali.2016.02.005
Seys D, Wu AW, van Gerven E, Vleugels A, Euwema M, Panella M, et al. Health care professionals as second victims after adverse events: A systematic review. Eval Heal Prof. 2013;36:135-62. https://doi.org/10.1177/0163278712458918
Scott SD, Hirschinger LE, Cox KR, McCoig M, Brandt J, Hall LW. The natural history of recovery for the healthcare provider «second victim» after adverse patient events. Qual Saf Heal Care. 2009;18:325-30. https://doi.org/10.1136/qshc.2009.032870
Martens J, van Gerven E, Lannoy K, Panella M, Euwema M, Sermeus W. Serious reportable events within the inpatient mental health care: Impact on physicians and nurses. Rev Calid Asist. 2020;31:26-33. https://doi.org/10.1016/j.cali.2016.04.004
Vanhaecht K, Seys D, Schouten L, Bruyneel L, Coeckelberghs E, Panella M, et al. Duration of second victim symptoms in the aftermath of a patient safety incident and association with the level of patient harm: A cross-sectional study in the Netherlands. BMJ Open. 2019;9:1-9. https://doi.org/10.1136/bmjopen-2019-029923
Schrøder K, Edrees HH, Depont R, Jørgensen JANS, Frances R, Hvidt NC. Second victims in the labor ward: Are Danish midwives and obstetricians getting the support they need ? Int J Qual Heal Care. 2019;31:583-9. https://doi.org/10.1093/intqhc/mzy219
Edrees HH, Paine LA, Feroli ER, Wu AW. Health care workers as second victims of medical errors. Pol Arch Med Wewn. 2011;121:101-8.
Rinaldi C, Leigheb F, Vanhaecht K, Donnarumma C, Panella M. Becoming a ‘‘second victim’’ in health care. Rev Calid Asist. 2020;31:11-9. https://doi.org/10.1016/j.cali.2016.05.001
Some similar items:
- Doris Cardona, Alejandro Estrada, Héctor Byron Agudelo, Quality of life and health conditions of the elderly population of Medellin. , Biomedica: Vol. 26 No. 2 (2006)
- José Moreno-Montoya, Ana M. Barragán, Margin Martínez, Amanda Rodríguez, Ángela Carmela González, Quality of life and perceived social support in people with HIV in Bogotá, Colombia , Biomedica: Vol. 38 No. 4 (2018)
- Jorge Alberto Cortés, Pilar Espitia, Yuliet Liliana Rosero-Lasso, Citywide preparedness for a pandemic: A crosssectional survey of knowledge, attitudes, and practices about respiratory infection prevention in Bogotá, Colombia , Biomedica: Vol. 40 No. Supl. 2 (2020): SARS-CoV-2 y COVID-19
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























