Factors affecting the tuberculosis program coverage at the first level of care in Honduras
Abstract
Introduction: There is a global consensus that early diagnosis and treatment of tuberculosis (TB) can accelerate its control and mitigate its consequences. The gradual increase in the TB mortality rate from 2014 to 2018 in Honduras, the reform of the health system in 2014, and the partial implementation of the “End TB” strategy motivated this study.
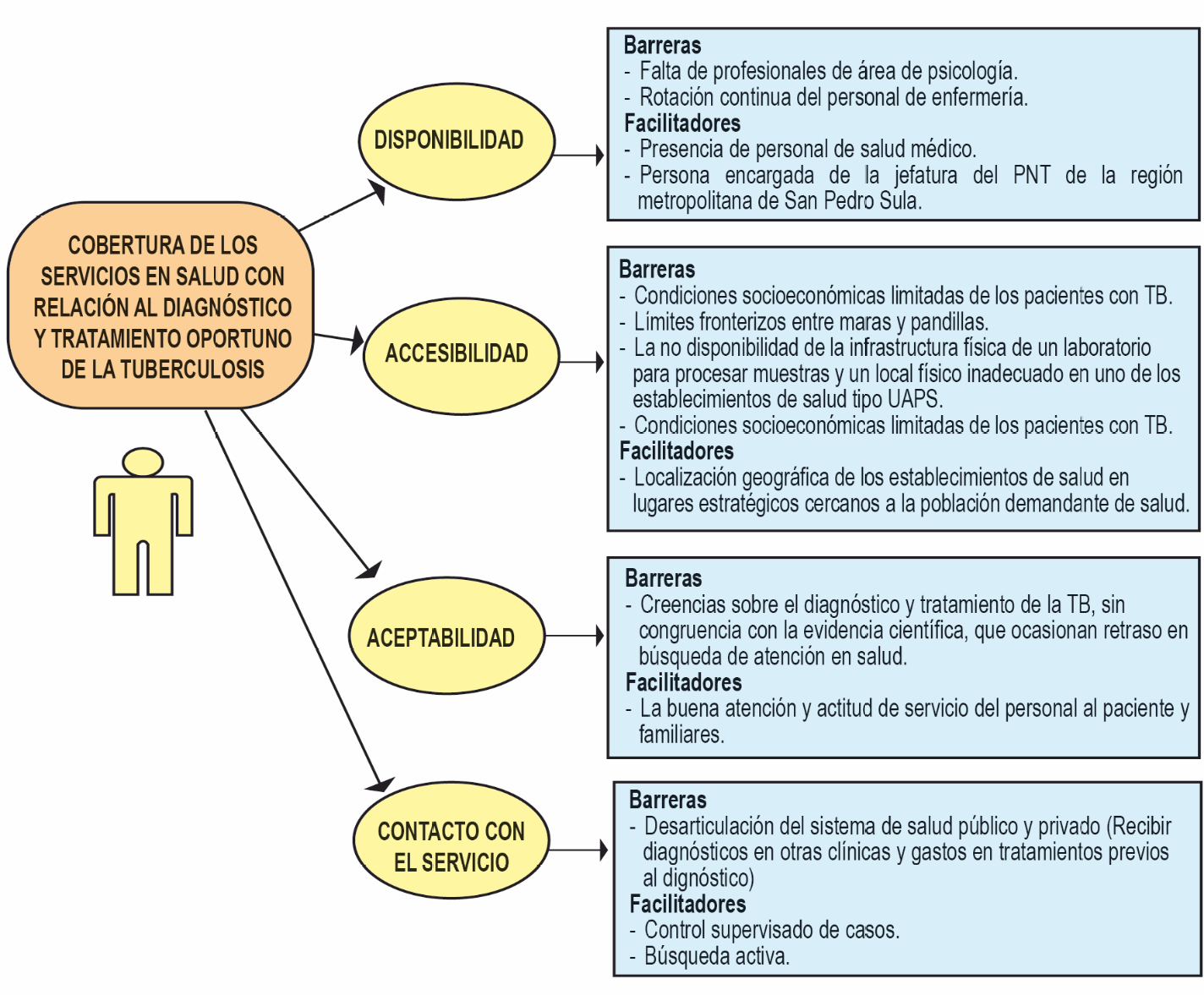
Objective: To analyze barriers to and facilitators of diagnosis and treatment affecting the national TB program coverage using data from 2015 to 2019 and provide tools for the effective implementation of the “End TB” strategy in San Pedro Sula, Honduras.
Materials and methods: This was an explanatory sequential mixed-methods study on smear-positive pulmonary TB patients older than 18 years of age. TB notification sheets and medical records from two primary health care facilities were reviewed. Semistructured interviews were conducted with health care providers, patients, and their families.
Results: A total of 74.6% of the cases (297/398) did not receive a timely diagnosis; 62.3% (185/297) were men, 80.8% (240/297) were adults, 53.7% (108/297) had less than high school education, 49.2% (123/297) had some occupation, and 98.2% of participants received timely treatment. Identified barriers included low socioeconomic conditions, lack of coordination between public and private health systems, and boundaries set by gangs. Identified facilitators included good care and attitude of the health care personnel and the availability of medications.
Conclusions: The lack of opportunity to diagnose the disease affected the coverage of the national TB program due to cultural and health care barriers.
Downloads
References
Organización Mundial de la Salud. Reporte Global de TB 2020. Fecha de consulta: 3 de mayo de 2021. Disponible en: https://www.who.int/publications/i/item/9789240013131
Organización Mundial de la Salud. Reporte Global de TB 2012. Fecha de consulta: 3 de septiembre de 2018. Disponible en: http://www.who.int/iris/handle/10665/75938
Organización Mundial de la Salud. Reporte Global de TB 2013. Fecha de consulta: 6 de septiembre de 2018. Disponible en: http://www.who.int/iris/handle/10665/91355
Organización Mundial de la Salud. Reporte Global de TB 2016. Fecha de consulta: 6 de septiembre de 2018. Disponible en: http://www.who.int/iris/handle/10665/250441
Organización Mundial de la Salud. Reporte Global de TB 2017. Fecha de consulta: 6 de septiembre de 2018. Disponible en: http://www.who.int/iris/handle/10665/259366
Organización Mundial de la Salud. Reporte Global TB 2018. Fecha de consulta: 28 de septiembre del 2018. Disponible en: https://apps.who.int/iris/bitstream/handle/10665/274453/9789241565646-eng.pdf
Secretaría de Salud de Honduras. Unidad de Vigilancia de la Salud. Resumen de Actividades de TB. I trimestre del 2018. Tegucigalpa: Secretaría de Salud de Honduras; 2018.
La Gaceta. Diario Oficial República de Honduras. Reglamento interno de organizacion y funciones de la Secretaría de Salud. Acuerdo N° 406. Número 33495. Tegucigalpa: La Gaceta; 2014. p. 4-56.
Varela-Martínez C. Tuberculosis en las principales cuidades de Honduras desde el enfoque de determinantes sociales. Construyendo una estrategia de salud para el desarrollo humano sostenible. Tesis doctoral. Tegucigalpa: Universidad Autonóma de Honduras; 2017. p. 1-355.
Secretaría de Salud de Honduras. Unidad de Vigilancia de la Salud. Informe situacion epidemiológica y programática de la TB en Honduras. Tegucigalpa: Secretaría de Salud de Honduras; 2017. p. 26-7.
Peters DH, Adam T, Alonge O, Agyepong IA, Tran N. Implementation research: what it is and how to do it. BMJ. 2013;347:1-7. https://doi.org/10.1136/bmj.f6753
Pirkis JE, Speed BR, Yung AP, Dunt DR, MacIntyre CR, Plant AJ. Time to initiation of antituberculosis treatment. Tuber Lung Dis. 1996;77:401-6. https://doi.org/10.1016/S0962-8479(96)90111-2
Petry MN. A comparison of young, middle-aged, and older adult treatment-seeking pathological gamblers. Gerontologist. 2002;42:92-9. https://doi.org/10.1093/geront/42.1.92
Ulin PR, Robinson ET, Tolley EE. Investigación aplicada en salud pública, métodos cualitativos. Washington, D. C.: OPS; 2006. p. 1-304.
Korstjens I, Moser A. Series: Practical guidance to qualitative research. Part 4: Trustworthiness and publishing. Eur J Gen Pract. 2018;24:120-4. https://doi.org/10.1080/13814788.2017.1375092
Hernández-Carrera R. La investigación cualitativa a través de entrevistas: su análisis mediante la teoría fundamentada. Cuestiones Pedagógicas. 2014;23:187-210.
Bronfenbrenner U. Ecological systems theory. London: Jessica Kingsley; 1992.
McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351-77. https://doi.org/10.1177/109019818801500401
Sallis JF, Owen N, Fisher EB. Ecological models of health behavior. En: Glanz K, Rimer BV, editors. Health Behavior and Health Education. 4th edition. San Francisco, CA: Jossey-Bass A Wiley; 2008. p. 465-85.
Benjumea-Bedoya D, Becker M, Haworth-Brockman M, Balakumar S, Hiebert K, Lutz JA, et al. Integrated Care for Latent Tuberculosis Infection (LTBI) at a primary health care facility for refugees in Winnipeg, Canada: A mixed-methods evaluation. Front Public Health. 2019;7:1-9. https://doi.org/10.3389/fpubh.2019.00057
Ivankova N, Creswell JW, Stick SL. Using mixed-methods sequential explanatory design: From theory to practice. Field Methods. 2006;18:3-20. https://doi.org/10.1177/1525822X05282260
Ministerio de Salud de Colombia. Resolución No 008430. Bogotá: Minsalud; 1993. p. 1-19.
Tanahashi T. Health service coverage and its evaluation. Bull World Health Organ. 1978;56:295-303.
Rao S. Tuberculosis and patient gender: An analysis and its implications in tuberculosis control. Lung India. 2009;26:46-7. https://doi.org/10.4103/0970-2113.48897
La Manna MP, Orlando V, Dieli F, Di Carlo P, Cascio A, Cuzzi G, et al. Quantitative and qualitative profiles of circulating monocytes may help identifying tuberculosis infection and disease stages. PLoS ONE. 2017;12:1-14. https://doi.org/10.1371/journal.pone.0171358
Miandad M, Nawaz-Ul-Huda S, Burke F, Hamza S, Azam M. Educational status and awareness among tuberculosis patients of Karachi. J Pakistan Med Assoc. 2016;66: 265-9.
Deponti G, Silva DR, Coelho AC, Muller AM, Dalcin P de T. Delayed diagnosis and associated factors among new pulmonary tuberculosis patients diagnosed at the emergency department of a tertiary care hospital in Porto Alegre, South Brazil: A prospective patient recruitment study. BMC Infect Dis. 2013;13:1-8. https://doi.org/10.1186/1471-2334-13-538
Rodrigo T. Análisis del retraso diagnóstico en tuberculosis. Rev Enf Emerg. 2019;18:113-8.
Rodríguez DA, Verdonck K, Bissell K, Victoria JJ, Khogali M, Marín D, et al. Monitoring delays in diagnosis of pulmonary tuberculosis in eight cities in Colombia. Rev Panam Salud Pública. 2016;39:12-8.
Htun YM, Khaing TMM, Ying Y, Myint Z, Aung ST, Hlaing TM. Delay in diagnosis and treatment among adult multidrug resistant tuberculosis patients in Yangon Regional Tuberculosis Center, Myanmar: A cross-sectional study. BMC Health Serv Res. 2018;18:1-13. https://doi.org/10.1186/s12913-018-3715-4
Gaviria M, Henao HM, Martínez T, Bernal H. Papel del personal de salud en el diagnóstico tardío de la tuberculosis pulmonar en adultos de Medellín, Colombia. Rev Panam Salud Pública. 2010;27:83-92.
Getnet F, Demissie M, Worku A, Gobena T, Seyoum B, Tschopp R. Determinants of patient delay in diagnosis of pulmonary tuberculosis in Somali pastoralist setting of Ethiopia: A matched case-control study. Int J Environ Res Public Health. 2019;16:1-12. https://doi.org/10.3390/ijerph16183391
InSight Crime A. Maras y pandillas en Honduras. 2015. Fecha de consulta: 14 de abril de 2020. Disponible en: https://www.insightcrime.org/images/PDFs/2015/MarasHonduras.pdf
Paramasivam S, Thomas B, Chandran P, Thayyil J, George B, Sivakumar CP. Diagnostic delay and associated factors among patients with pulmonary tuberculosis in Kerala. J Fam Med Prim care. 2017;6:643-8. https://doi.org/10.4103/2249-4863.222052
Arbeláez MP. La reforma del sector salud y el control de la tuberculosis en Colombia. En: Yadón ZE, Gürtler RE, Tobar F, Medici AC. Descentralización y gestión del control de las enfermedades transmisibles en América Latina. Buenos Aires: OPS; 2006. p. 115-28.
Ayala-Cerna C, Kroger A. La reforma del sector salud en Colombia y sus efectos en los programas de control de tuberculosis e inmunización. Cad Saúde Pública. 2002;18: 1771-81. https://doi.org/10.1590/S0102-311X2002000600032
Gebremariam MK, Bjune GA, Frich JC. Barriers and facilitators of adherence to TB treatment in patients on concomitant TB and HIV treatment: A qualitative study. BMC Public Health. 2010;10:1-9. https://doi.org/10.1186/1471-2458-10-651
Awoke N, Dulo B, Wudneh F. Total delay in treatment of tuberculosis and associated factors among new pulmonary TB patients in selected health facilities of Gedeo Zone, Southern Ethiopia 2017/18. Interdiscip Perspect Infect Dis. 2019;2019:1-14. https://doi.org/10.1155/2019/2154240
Peri AM, Bernasconi DP, Galizz N, Matteelli A, Codecasa L, Giorgio V, et al. Determinants of patient and health care services delays for tuberculosis diagnosis in Italy: A cross-sectional observational study. BMC Infect Dis. 2018;18:1-11. https://doi.org/10.1186/s12879-018-3609-4
Some similar items:
- Liddy Varela, Jimena Ortiz, Pamela K. García, Lucy Luna, Jose F. Fuertes-Bucheli, Robinson Pacheco, Factors associated with unsuccessful treatment outcome for tuberculosis in previously treated patients in Cali, Colombia, during the period 2015-2019 , Biomedica: Vol. 43 No. 3 (2023)
- Nelson José Alvis-Zakzuk, María de los Ángeles Carrasquilla, Verónica Jhajaira Gómez, Jaime Robledo, Nelson Rafael Alvis-Guzmán, José Mauricio Hernández, Diagnostic accuracy of three technologies for the diagnosis of multi-drug resistant tuberculosis , Biomedica: Vol. 37 No. 3 (2017)
- Juan Gabriel Bueno-Sánchez, Jairo René Martínez-Morales, Elena E. Stashenko, Wellman Ribón, Anti-tubercular activity of eleven aromatic and medicinal plants occurring in Colombia , Biomedica: Vol. 29 No. 1 (2009)
- María Consuelo Garzón, Dailyn Yorledy Angée, Claudia Llerena, Dora Leticia Orjuela, Jorge Ernesto Victoria, Surveillance of Mycobacterium tuberculosis resistance to antituberculosis drugs , Biomedica: Vol. 28 No. 3 (2008)
- Leandro Galvis, Ángel Y. Sánchez, Leonardo F. Jurado, Martha I. Murcia, Tuberculosis associated with tumor necrosis factor-α antagonists, case description and analysis of reported cases in Colombia , Biomedica: Vol. 38 No. 1 (2018)
- Diego Chaves, Andrea Sandoval, Luis Rodríguez, Juan C. García, Silvia Restrepo, María Mercedes Zambrano, Comparative analysis of six Mycobacterium tuberculosis complex genomes , Biomedica: Vol. 30 No. 1 (2010)
- María Imaz, Sonia Allassia, Mónica Aranibar, Alba Gunia, Susana Poggi, Ana Togneri, Lidia Wolff, Group of Implementation of Fluorescence, Performance of LED fluorescence microscopy for the detection of acid-fast bacilli from respiratory samples in peripheral laboratories in Argentina , Biomedica: Vol. 37 No. 2 (2017)
- Luis Miguel Sosa, Luz Libia Cala, Julio César Mantilla, Congenital tuberculosis associated with maternal disseminated miliary tuberculosis , Biomedica: Vol. 27 No. 4 (2007)
- Jorge Alberto García-Aguilar, Jackeline Alger, Frequency of strongyloidiasis and associated factors: Analysis of 13 years of laboratory results in a tertiary referral hospital in Honduras, 2010-2022 , Biomedica: Vol. 43 No. 4 (2023)
- Adriana Rojas-Villarraga, Carlos Andrés Agudelo, Ricardo Pineda-Tamayo, Alvaro Porras, Gustavo Matute, Juan Manuel Anaya, Tuberculosis in patientes treated with tumor necrosis factor alpha antagonists living in an endemic area. Is the risk worthwhile? , Biomedica: Vol. 27 No. 2 (2007)
Funding data
-
TDR
Grant numbers TDR B40323
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























