Chlamydia psittaci seropositivity in workers exposed to birds and review of the literature: Evidence of circulation in Antioquia
Abstract
Introduction. Psittacosis is a zoonotic disease caused by Chlamydia psittaci, a bacterium classified as an agent with bioterrorist potential. It has caused multiple outbreaks in exposed poultry workers around the world. Colombia has no epidemiological follow-up of the infection and a big knowledge gap.
Objectives. To determine the antibodies’ frequency against C. psittaci in workers with occupational exposure to birds and to review the literature on studies conducted in Colombia.
Materials and methods. We conducted a cross-sectional descriptive study with analytical intent on workers in contact with birds and reviewed the related literature in Colombia. IgM and IgG serum antibodies against C. psittaci were detected by microimmunofluorescence. The sociodemographic and exposure characteristics were expressed as frequencies and summary measures. Associated factors were explored by bivariate and multivariate analysis. The scientific and gray literature review was done with a structured search.
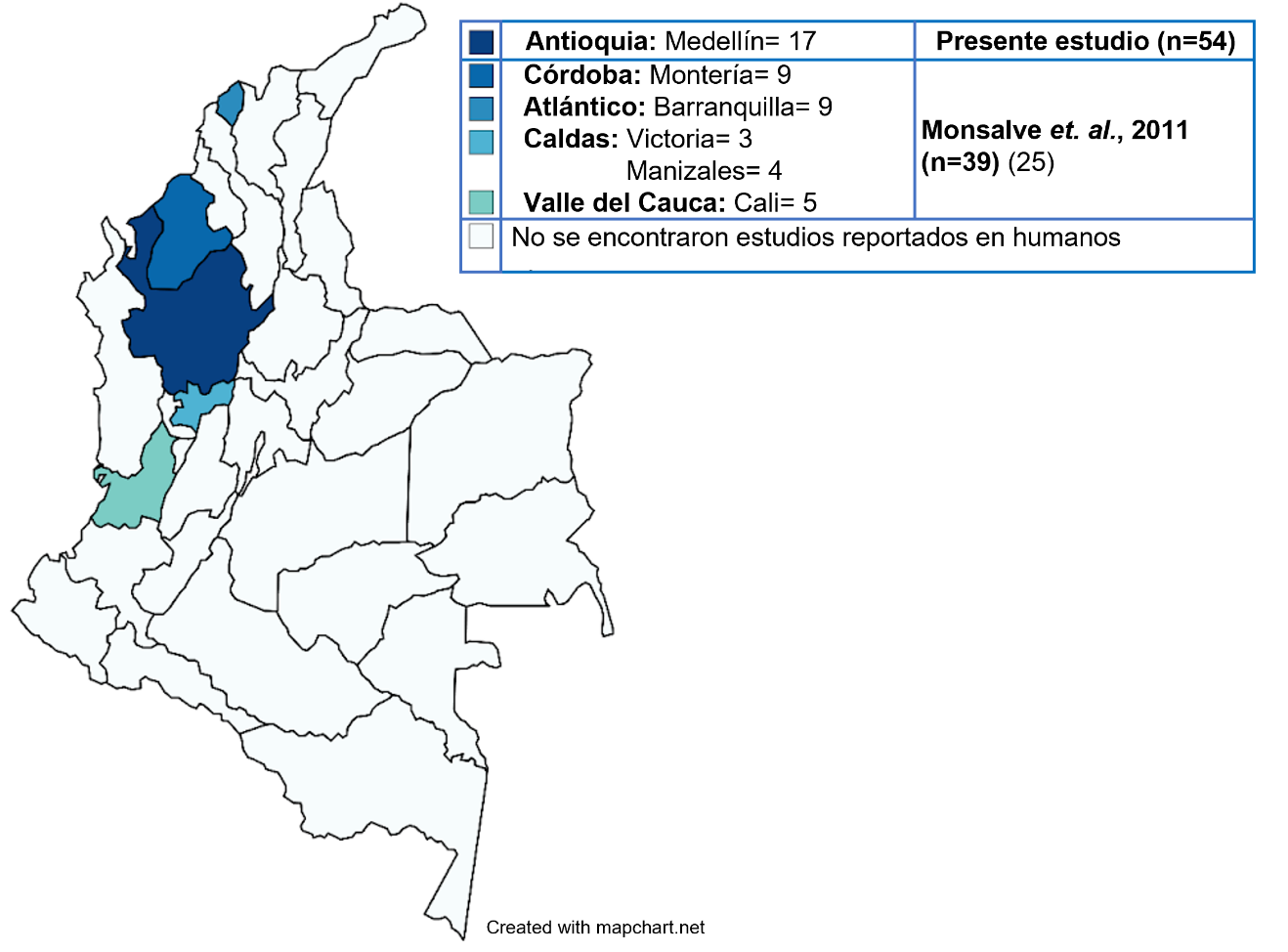
Results. We analyzed 54 workers in contact with birds. Antibody prevalence was 31.5%. Slaughtering and evisceration by non-veterinarians was a risk factor for antibody presence. There are only four previous studies on C. psittaci in Colombia.
Conclusions. Here, we present the first evidence of C. psittaci circulation among workers exposed to birds in Antioquia and the second report in the country. These findings contribute to the “One Health” public health strategy.
Downloads
References
Chu J, Yarrarapu SNS, Vaqar S, Durrani MI. Psittacosis. Treasure Island (FL): Stat Pearls Publishing; 2023. Fecha de consulta: 11 de diciembre de 2022. Disponible en: https://www.ncbi.nlm.nih.gov/books/NBK538305/
Stewardson AJ, Grayson ML. Psittacosis. Infect Dis Clin North Am. 2010;24:7-25. https://doi.org/10.1016/j.idc.2009.10
Kaleta EF, Taday EMA. Avian host range of Chlamydophila spp. based on isolation, antigen detection and serology. Avian Pathol. 2003;32:435-62. https://doi.org/10.1080/03079450310001593613
The Center for Food Security & Public Health, Institute for International Cooperation in Animal Biologics. Psittacosis/Clamidosis Aviar. Fecha de consulta: 9 de diciembre de 2022. Disponible en: https://www.cfsph.iastate.edu/Factsheets/es/psittacosis-es.pdf
Rodríguez-Leo C, Camacho D, Hernández V, Viettri M, Flores C, Henríquez H, et al. Primera evidencia de Chlamydia psittaci en hurón sable (Mustella putorios furo) en Venezuela. Revista de la Facultad de Medicina Veterinaria y de Zootecnia. 2018;65. https://doi.org/10.15446/rfmvz.v65n2.75639
Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases. Emergency preparedness and response. Bioterrorism agents/diseases. Fecha de consulta: 10 de diciembre de 2022. Disponible en: https://emergency.cdc.gov/agent/agentlist-category.asp
Hogerwerf L, De Gier B, Baan B, van Der Hoek W. Chlamydia psittaci (psittacosis) as a cause of community-acquired pneumonia: A systematic review and meta-analysis. Epidemiol Infect. 2017;145:3096-105. https://doi.org/10.1017/S0950268817002060
Dickx V, van Droogenbroeck C, van Vaerenbergh B, Herman P, Braeckman L, Vanrompay D. Chlamydia psittaci, causative agent of avian chlamydiosis and human psittacosis: Risk assessment and biosafety recommendations for laboratory use. Appl Biosaf. 2012;17:82-8.
Fenga C, Cacciola A, Di Nola C, Camileri S, Lo Giudice D, Pugliese M, et al. Serologic investigation of the prevalence of Chlamydophila psittaci in occupationally-exposed subjects in eastern Sicily. Ann Agric Environ Med. 2007;14:93-6.
Ramsey E. The psittacosis outbreak of 1929–1930. J Avian Med Surg. 2003;17:235-7.
Sachse K, Laroucau K, Vanrompay D. Avian chlamydiosis. Curr Clin Microbiol Rep. 2015;2:10-21. https://doi.org/10.1007/s40588-014-0010-y
Cadario ME, Frutos MC, Arias MB, Origlia JA, Zelaya V, Madariaga MJ, et al. Epidemiological and molecular characteristics of Chlamydia psittaci from 8 human cases of psittacosis and 4 related birds in Argentina. Rev Argent Microbiol. 2017;49:323-7. https://doi.org/10.1016/j.ram.2017.04.001
Leo JR, Hernández V, Abou Orm S, Díaz Yender, Camacho D, Naillet A, et al. Chlamydia psittaci en aves psitácidas en dos parques zoológicos de Venezuela. Acta Biol Colomb. 2017;22. https://doi.org/10.15446/abc.v22n3.64742
Vega VV. Determinación de la presencia de bacterias de la familia Chlamydiaceae mediante reacción en cadena de la polimerasa PCR en las aves Psittaciformes de dos centros de manejo de fauna silvestre: zoológico de Quito en Guayllabamba y Centro de Rescate Hacienda Santa Martha (tesis). Quito: Universidad San Francisco de Quito; 2010.
Pinto K, Villalobos F, Fischer C, Barrientos C, González-Acuña D, Troncoso I. Detección serológica de Chlamydophila psittaci en psitácidos en cautiverio de la Región del Biobío, Chile. Rev de Investig Vet del Perú. 2018;29:950-6. https://doi.org/10.15381/rivep.v29i3.14838
Raso T de F, Júnior AB, Pinto AA. Evidence of Chlamydophila psittaci infection in captive Amazon parrots in Brazil. J Zoo Wildl Med. 2002;33:118- 21. https://doi.org/10.1638/1042-7260(2002)033[0118:EOCPII]2.0.CO;2
Deschuyffeleer TP, Tyberghien LF, Dickx VL, Geens T, Saelen JM, Vanrompay DC, et al. Risk assessment and management of Chlamydia psittaci in poultry processing plants. Ann Occup Hyg. 2012;56:340-9. https://doi.org/10.1093/annhyg/mer102
Rotz LD, Khan AS, Lillibridge SR, Ostroff SM, Hughes JM. Public health assessment of potential biological terrorism agents. Emerg Infect Dis. 2002;8:225-30. https://doi.org/10.3201/eid0802.010164
Centers for Disease Control and Prevention. Psittacosis. Fecha de consulta: 9 de diciembre de 2022. Disponible en: https://www.cdc.gov/pneumonia/atypical/psittacosis/about/causes.html
Ghai RR, Wallace RM, Kile JC, Shoemaker TR, Vieira AR, Negron ME, et al. A generalizable one health framework for the control of zoonotic diseases. Sci Rep. 2022;12:8588. https://doi.org/10.1038/s41598-022-12619-1
Sachse K, Vretou E, Livingstone M, Borel N, Pospischil A, Longbottom D. Recent developments in the laboratory diagnosis of chlamydial infections. Vet Microbiol. 2009;135:2-21. https://doi.org/10.1016/j.vetmic.2008.09.040
Ravichandran K, Anbazhagan S, Karthik K, Angappan M, Dhayananth B. A comprehensive review on avian chlamydiosis: A neglected zoonotic disease. Trop Anim Health Prod. 2021;53:414. https://doi.org/10.1007/s11250-021-02859-0
Instituto Nacional de Salud. Fichas y protocolos. Fecha de consulta: 9 de diciembre de 2022. Disponible en: https://www.ins.gov.co/buscador-eventos/Paginas/Fichas-y-Protocolos.aspx
Instituto Colombiano Agropecuario, Ministerio de Agricultura República de Colombia. Resolución No. 3714 de 2015. Por la cual se establecen las enfermedades de declaración obligatoria en Colombia. Fecha de consulta: 10 de diciembre de 2022. Disponible en: https://www.ica.gov.co/getattachment/3188abb6-2297-44e2-89e6-3a5dbd4db210/2015R3714.aspx#:~:text=003714-,%22Por%20la%20cual%20se%20establecen%20las,de%20declaraci%C3%B3n%20obligatoria%20en%20Colombia%22.&text=Enfermedades%20e%20infecciones%20de%20los%20%C3%A9quidos%20Anemia%20infecciosa%20equina%20Durina,Enfermedad%20de%20Borna%20(Bunyaviridae)
Monsalve S, Miranda J, Mattar S. Primera evidencia de circulación de Chlamydophila psittaci en Colombia: posible riesgo de salud pública. Rev Salud Pública. 2011;13:314-26. https://doi.org/10.1590/S0124-00642011000200013
Vircell Microbiologists. Chlamydia: el método MIF de referencia para un análisis específico de especie. Fecha de consulta: 9 de diciembre de 2022. Disponible en: https://www.vircell.com/media/filer_public/fe/e9/fee9c3f5-1c8b-4f51-b605-78fbc706e0be/chlamydophila_pneumoniae_ifa_es.pdf
Rivera-Osorio S. Identificación de Chlamydophila psittaci en aves Psitácidas del hogar de paso de fauna silvestre “La María”, Pereira (tesis). Pereira: Universidad Tecnológica de Pereira; 2018.
Ocampo MC, Rendón L, Castillo L, Ramírez A, Mosquera G, Jaramillo-Delgado I. Detección serológica y molecular de Chlamydia psittaci en palomas (Columba livia domestica) en tres parques de la ciudad de Medellín. Rev Panam Enf Inf. 2019;2:e3. https://revistas.utp.edu.co/index.php/panamericana/article/view/24443/16348
Ruiz-Laiton A, Molano-Ayala N, García-Castiblanco S, Puentes-Orozco AM, Falla AC, Camargo M, et al. The prevalence of Chlamydia psittaci in confiscated Psittacidae in Colombia. Prev Vet Med. 2022;200:105591. https://doi.org/10.1016/j.prevetmed.2022.105591
Gitsels A, van Lent S, Sanders N, Vanrompay D. Chlamydia : What is on the outside does matter. Crit Rev Microbiol. 2020;46:100-19. https://doi.org/10.1080/1040841X.2020.1730300
Lugert R, Groß U, Masanta WO, Linsel G, Heutelbeck A, Zautner AE. Seroprevalence of Chlamydophila psittaci among employees of two German duck farms. Eur J Microbiol Immunol (Bp). 2017;7:267-73. https://doi.org/10.1556/1886.2017.00024
Shaw KA, Szablewski CM, Kellner S, Kornegay L, Bair P, Brennan S, et al. Psittacosis outbreak among workers at chicken slaughter plants, Virginia and Georgia, USA, 2018. Emerg Infect Dis. 2019;25:2143-5. https://doi.org/10.3201/eid2511.190703
Laroucau K, Aaziz R, Meurice L, Servas V, Chossat I, Royer H, et al. Outbreak of psittacosis in a group of women exposed to Chlamydia psittaci- infected chickens. Euro Surveill. 2015;18:20:21155. https://doi.org/10.2807/1560-7917.es2015.20.24.21155.35
Centers for Disease Control and Prevention. Psittacosis. Information about psittacosis for employers and employees at poultry slaughter plants. Fecha de consulta: 10 de diciembre de 2022. Disponible en: https://www.cdc.gov/pneumonia/atypical/psittacosis/surveillancereporting/outbreaks/poultry-slaughter-plants-factsheet.html
Balsamo G, Maxted AM, Midla JW, Murphy JM, Wohrle R, Edling TM, et al. Compendium of measures to control Chlamydia psittaci infection among humans (psittacosis) and pet birds (avian chlamydiosis), 2017. J Avian Med Surg. 2017;31:262-82. https://doi.org/10.1647/217-265
Occupational Safety and Health Administration. OSHA Fact Sheet. Personal Sheet Personal Protective Equipment. Fecha de consulta: 10 de diciembre de 2022. Disponible en: https://www.osha.gov/sites/default/files/publications/ppe-factsheet.pdf
Liu SY, Li KP, Hsieh MK, Chang PC, Shien JH, Ou SC. Prevalence and genotyping of Chlamydia psittaci from domestic waterfowl, companion birds, and wild birds in Taiwan. Vector Borne Zoonotic Dis. 2019;19:666-73. https://doi.org/10.1089/vbz.2018.2403.39
Vanrompay D, Harkinezhad T, van de Walle M, Beeckman D, van Droogenbroeck C, Verminnen K, et al. Chlamydophila psittaci transmission from pet birds to humans. Emerg Infect Dis. 2007;13:1108-10. https://doi.org/10.3201/eid1307.070074
Some similar items:
- Mónica Marcela Jiménez, Jesús Arias, Gabriel Carrasquilla, Seroprevalence of dengue infection in the municipalities of Armenia, Calarcá, La Tebaida and Montenegro in Quindío, 2014 , Biomedica: Vol. 37 No. 1 (2017)
- Milagros Joya , Ricardo Heredia , Daniel Bastidas, Gilberto Bastidas , Detection of Chlamydia trachomatis infection in sexually active women in Venezuela , Biomedica: Vol. 42 No. 3 (2022)
- Jairo Echeverry, Carlos Mauricio Hurtado, Myriam Gutiérrez, Clinical manifestations of lead levels in children exposed to automobile battery recycling processes in Soacha and Bogotá, D.C. , Biomedica: Vol. 28 No. 1 (2008)
- Carlos Humberto Torres, Marcela E. Varona, Angélica Lancheros, Rosa Isabel Patiño, Helena Groot, DNA damage assessment and biological monitoring of occupational exposure to organic solvents, 2006 , Biomedica: Vol. 28 No. 1 (2008)
- Omayda Cárdenas, Elizabeth Silva, Jaime Eduardo Ortiz, The use of acetylcholinesterase inhibitors pesticides in eleven local health institutions, Colombia, 2002-2005 , Biomedica: Vol. 30 No. 1 (2010)
- Lucía Carolina Leal-Esteban, Jessica Lineth Rojas, Andrea Lizeth Jaimes, Juan David Montoya, Nilton Edu Montoya, Lily Leiva, Claudia Milena Trujillo-Vargas, An immunoenzymatic test for IgG antibody levels against 10 serotypes of Streptococcus pneumoniae , Biomedica: Vol. 32 No. 1 (2012)
- Francisca Mercedes Monsalve-Castillo, Luciana Ana Costa-León, María Elena Castellano, Anais Suárez, Ricardo José Atencio, Prevalence of infectious agents in indigenous women of childbearing age in Venezuela , Biomedica: Vol. 32 No. 4 (2012)
- Beatriz Eugenia Ferro, Ana Lucía Rodríguez, Mauricio Pérez, Bruno Luis Travi, Seroprevalence of Leptospira infection in habitants of peripheral neighborhoods in Cali, Colombia. , Biomedica: Vol. 26 No. 2 (2006)
- Manuel Toquero, Antonio Morocoima, Elizabeth Ferrer, Seroprevalence and risk factors of cysticercosis in two rural communities in Anzoátegui state, Venezuela , Biomedica: Vol. 37 No. Sup.1 (2017): Suplemento 1, Alteraciones del sistema nervioso
- Jorge Sánchez, Susana Diez, Ricardo Cardona, Pet avoidance in allergy cases: Is it possible to implement it? , Biomedica: Vol. 35 No. 3 (2015)
Copyright (c) 2023 Biomedica

This work is licensed under a Creative Commons Attribution 4.0 International License.
Funding data
-
Universidad Cooperativa de Colombia
Grant numbers INV1195
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























