Sporotrichosis in Argentina: clinical and epidemiological analysis
Abstract
Introduction. Sporotrichosis is an implantation mycosis caused by Sporothrix spp. It is distributed worldwide and can be found in vegetation and soil. The most frequent route of infection is by trauma with elements contaminated with fungal propagules. Since domestic cats are the most affected animals and can transmit this infection to humans, sporotrichosis is considered a zoonosis. Clinical presentations include nodular lymphangitis, fixed cutaneous, pulmonary (rare), and disseminated (exceptional).
Objectives. To analyze the epidemiology of sporotrichosis in Argentina during 2010 and 2022. To describe the clinical presentation, diagnostic methods, and treatment of cases diagnosed during this period. To know the circulating genotypes and to observe possible associations with the geographic location where the infection was acquired.
Materials and methods. Analytical, retrospective, and observational study. We analyzed the medical records of patients with sporotrichosis from 12 health institutions in Argentina, between 2010 and 2022.
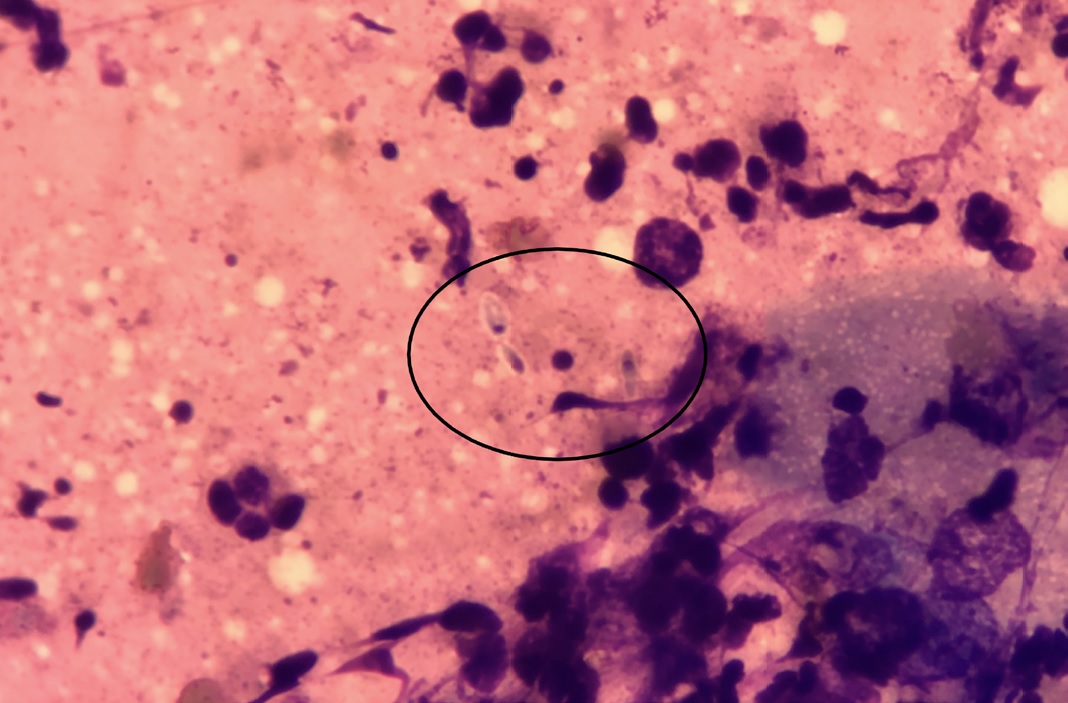
Results. We present 54 cases in which the most frequent clinical form was nodular lymphangitis, and the treatment of choice was itraconazole. Conventional diagnosis was
made in all cases. Culture of clinical samples was more sensitive than direct examination because it allowed the isolation of Sporothrix spp. in all 54 cases. Molecular identification was performed in 22 cases, with Sporothrix schenkii sensu stricto being the most frequently isolated species.
Conclusions. This study allowed to know the epidemiology of this mycosis in Argentina, as well as the availability of diagnostic methods and the treatment of choice.
Downloads
References
Lopes-Bezerra LM, Mora-Montes HM, Zhang Y, Nino-Vega G, Rodrigues AM, de Camargo ZP, et al. Sporotrichosis between 1898 and 2017: The evolution of knowledge on a changeable disease and on emerging etiological agents. Med Mycol. 2018;56(Suppl. 1):S126-43. https://doi.org/10.1093/mmy/myx103
Rossow JA, Queiroz-Telles F, Caceres DH, Beer KD, Jackson BR, Pereira JG, et al. A One health approach to combatting Sporothrix brasiliensis: narrative review of an emerging zoonotic fungal pathogen in South America. J Fungi (Basel). 2020;6:247. https://doi.org/10.3390/jof6040247
Rodrigues AM, Della Terra PP, Gremião ID, Pereira SA, Orofino-Costa R, de Camargo ZP. The threat of emerging and re-emerging pathogenic Sporothrix species. Mycopathologia. 2020;185:813-42. https://doi.org/10.1007/s11046-020-00425-0
Cabañes FJ. Esporotricosis en Brasil: animales + humanos = una sola salud. Rev Iberoam Micol. 2020;37:73-4. https://doi.org/10.1016/j.riam.2020.01.001
de Andrade Galliano Daros Bastos F, Raimundo Cognialli RC, Rodrigues de Farias M, dos Santos Monti F, Wu K, Queiroz-Telles F. Spread of Sporothrix spp. through respiratory droplets from infected cats: A potential route of transmission. Med Mycol. 2022;60:myac079. https://doi.org/10.1093/mmy/myac079
Bonifaz A, Tirado-Sánchez A. Cutaneous disseminated and extracutaneous sporotrichosis: Current status of a complex disease. J Fungi. 2017;3:6. https://doi.org/10.3390/jof3010006
Chakrabarti A, Bonifaz A, Gutierrez-Galhardo MC, Mochizuki T, Li S. Global epidemiology of sporotrichosis. Med Mycol. 2015 53:3-14. https://doi.org/10.1093/mmy/myu062
Han HS, Kano R. Feline sporotrichosis in Asia. Braz J Microbiol. 2020;52:125-34. https://doi.org/10.1007/s42770-020-00274-5
Martínez Cepeda GE. Esporotricosis en caninos y felinos: hallazgos clínicos, métodos de diagnóstico y tratamiento. Analecta Vet. 2016;36:30-9.
Rodrigues AM, Gonçalves SS, de Carvalho JA, Borba-Santos LP, Rozental S, Camargo ZP. Current progress on epidemiology, diagnosis, and treatment of sporotrichosis and their future trends. J Fungi. 2022;8:776. https://doi.org/10.3390/jof8080776
Gremião ID, Miranda LH, Pereira-Oliveira GR, Menezes RC, Machado AC, Rodrigues AM, et al. Advances and challenges in the management of feline sporotrichosis. Rev Iberoam Micol. 2022;39:61-7. https://doi.org/10.1016/j.riam.2022.05.002
Queiroz-Telles F, Bonifaz A, Cognialli R, Lustosa BPR, Vicente VA, Ramírez-Marín HA. Sporotrichosis in children: Case series and narrative review. Curr Fungal Infect Rep. 2022;16:33-46. https://doi.org/10.1007/s12281-022-00429-x
Mora-Montes HM. Sporothrix and sporotrichosis 2.0. J Fungi. 2022;8:821. https://doi.org/10.3390/jof8080821
Nava-Pérez N, Neri-García LG, Romero-González OE, Terrones-Cruz JA, García-Carnero LC, Mora-Montes HM. Biological and clinical attributes of Sporothrix globosa, a causative agent of sporotrichosis. Infect Drug Resist. 2022;15:2067-90. https://doi.org/10.2147/IDR.S362099
Rudramurthy SM, Shankarnarayan SA, Hemashetter BM, Verma S, Chauhan S, Nath R, et al. Phenotypic and molecular characterisation of Sporothrix globosa of diverse origin from India. Braz J Microbiol. 2021;52:91-100. https://doi.org/10.1007/s42770-020-00346-6
Poester VR, Basso RP, Stevens DA, Munhoz LS, de Souza Rabello VB, Almeida-Paes R, et al. Treatment of human sporotrichosis caused by Sporothrix brasiliensis. J Fungi. 2022;8:70. https://doi.org/10.3390/jof8010070
Cognialli R, Bloss K, Weiss I, Caceres DH, Davis R, Queiroz-Telles F. A lateral flow assay for the immunodiagnosis of human cat-transmitted sporotrichosis. Mycoses. 2022;65:926-34. https://doi.org/10.1111/myc.13516
Kauffman C.A.; Bustamante, B.; Chapman, S.W.; Pappas, P.G. Clinical practice guidelines for the management of sporotrichosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis. 2007;45:1255-65. https://doi.org/10.1086/522765
Bonifaz A, Vázquez-González D. Diagnosis, and treatment of lymphocutaneous sporotrichosis: What are the options? Curr Fungal Infect Rep. 2013;7:252-9. https://doi.org/10.1007/s12281-013-0140-3
Almeida-Paes R, Oliveira MME, Freitas DFS, Valle ACFD, Gutierrez‑Galhardo MC, Zancopé-Oliveira RM. Refractory sporotrichosis due to Sporothrix brasiliensis in humans appears to be unrelated to in vivo resistance. Med Mycol. 2017;55:507-17. https://doi.org/10.1093/mmy/myw103
Zhang X, Huang H, Feng P, Zhang J, Zhong Y, Xue R, et al. In vitro activity of itraconazole in combination with terbinafine against clinical strains of itraconazole-insensitive Sporothrix schenckii. Eur J Dermatol. 2011;21:573-6. https://doi.org/10.1684/ejd.2011.1400
Some similar items:
- Ricardo G. Díaz, Karina A. Salvatierra, Gustavo A. Silva, Enrique J. Deschutter, Fernando J. Bornay-Llinares, Lucrecia Acosta, First molecular characterization of Leishmania infantum species in patients infected with visceral leishmaniasis in Misiones province, Argentina , Biomedica: Vol. 39 No. 2 (2019)
- Juan Sergio Mollinedo, Zoraida Mollinedo , Marcelo Magne , Wilson J. Gironda, Óscar D. Salomón , Leishmaniasis en Bolivia. Comprehensive review and current status in Tarija, in the border with Argentina , Biomedica: Vol. 40 No. Supl. 1 (2020): Mayo, Infecciones en el trópico
- Laura C. Álvarez-Acevedo, María C. Zuleta-González, Óscar M. Gómez-Guzmán, Álvaro L. Rúa-Giraldo, MSc PhD, M.D. PhD, Martha E. Urán-Jiménez, Myrtha Arango-Arteaga, MSc PhD, Manoel Marques Evangelista de Oliveira, María del P. Jiménez-Alzate, Phenotypic and genotypic characterization of Colombian clinical isolates of Sporothrix spp. , Biomedica: Vol. 43 No. Sp. 1 (2023): Agosto, Micología médica
Copyright (c) 2023 Biomedica

This work is licensed under a Creative Commons Attribution 4.0 International License.
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























