Clinical and metabolic effect of a multidisciplinary intervention through a comprehensive care program for children and adolescents with obesity
Abstract
Introduction: The approach to childhood obesity requires multidisciplinary programs including all the dimensions susceptible to management.
Objective: To describe the clinical and metabolic changes in patients with obesity after a comprehensive care program for childhood obesity.
Materials and methods: We conducted a retrospective observational and analytical study in a cohort of patients between 6 and 17 years old treated in the obesity program at the Hospital Universitario San Vicente Fundación (2012-2015). We carried out multidisciplinary care and educational intervention. Anthropometric and laboratory variables were evaluated both at admission to the program and in the last evaluation and statistical differences were sought according to the follow-up time.
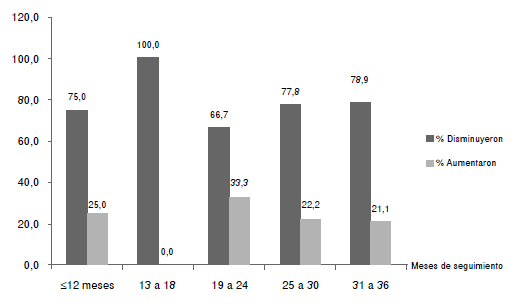
Results: We evaluated 53 patients, of whom 52.8% were men, with an average age of 11 ± 2 years. The follow-up extended for 18 ± 6 months though 30% of the patients were followed for 31 to 36 months. There was a decrease in the BMI (Z score) between admission (2.75 ± 0.58 and the last control (2.32 ± 0.63) with a p-value of 0.000 (95% CI: 0.27 -0.58); 79.25% of the patients reduced the BMI Z score. This decrease was significant regardless of the follow-up time. The proportion of patients with a BMI Z score >3 decreased from 33.4% to 14.6%. The number of positive criteria for metabolic syndrome decreased in the follow-up. Triglycerides and HbA1c were the metabolic variables that improved significantly.
Conclusions: The management of childhood obesity with an interdisciplinary intervention associated with continuous group educational support can significantly impact on clinical and metabolic changes. It is necessary to continue monitoring over time to prevent relapse.
Downloads
References
Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311:806-14. https://doi.org/10.1001/jama. 2014.732
World Health Organization. WHO | Obesity and overweight. Geneva: WHO; 2016. Fecha de consulta: 30 de diciembre de 2017. Disponible en: http://www.who.int/gho/ncd/risk_ factors/overweight/en/
Greydanus DE, Agana M, Kamboj MK, Shebrain S, Soares N, Eke R, et al. Pediatric obesity: Current concepts. Dis Mon. 2018;64:98-156. https://doi.org/10.1016/j.disamonth.2017.12.001
Instituto Colombiano de Bienestar Familiar. Encuesta Nacional de la Situación Nutricional, 2015 (ENSIN, 2015). Fecha de consulta: 30 de enero de 2018. Disponible en: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/ED/GCFI/ presentacion-ensin-2017-medellin.pdf
Alcaldía de Medellín. Plan de seguridad alimentaria y nutricional del municipio de Medellín, 2016-2028. Fecha de consulta: 10 de noviembre de 2015. Disponible en:
Daniels SR. Complications of obesity in children and adolescents. Int J Obes. 2009;33(Suppl.1):S60-5. https://doi.org/10.1038/ijo.2009.20
Daniels SR, Jacobson MS, McCrindle BW, Eckel RH, Sanner BM. American Heart Association Childhood Obesity Research Summit: Executive summary. Circulation. 2009;119:2114-23. https://doi.org/10.1161/CIRCULATIONAHA.109.192215
Lee YS. Consequences of childhood obesity. Ann Acad Med Singapore. 2009;38;75-7.
Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362:485-93. https://doi.org/10.1056/NEJMoa0904130
Dietz WH. Health consequences of obesity in youth: Childhood predictors of adult disease. Pediatrics. 1998;101:518-25.
Schaefer A, Winkel K, Finne E, Kolip P, Reinehr T. An effective lifestyle intervention in overweight children: One-year follow-up after the randomized controlled trial on “Obeldicks light”. Eur J Clin Nutr. 2011;30:629-33. https://doi.org/10.1016/j.clnu.2011.03.012
Swinburn B. Obesity prevention in children and adolescents. Child Adolesc Psychiatric Clin N Am. 2009;18:209-23. https://doi.org/10.1016/j.chc.2008.07.015
Swinburn BA, de Silva-Sanigorski AM. Where to from here for preventing childhood obesity: An international perspective. Obesity (Silver Spring). 2010;18(Suppl.1):S4-7. https://doi.org/10.1038/oby.2009.424
Oude Luttikhuis H, Baur L, Jansen H, Shrewsbury VA, O’Malley C, Stolk RP, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev. 2009;(1):CD001872. https://doi.org/10.1002/14651858.CD001872.pub2
Kavey RW, Simons DG. National Heart, Lung, and Blood Institute, National Institutes of Health y American Academy of Pediatrics. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents: Summary Report. Pediatrics. 2011;128(Suppl.6):S213-56. https://doi.org/10.1542/peds.2009-2107C
Congreso de Colombia. Ley 1355 de 2009, por medio de la cual se define la obesidad y las enfermedades crónicas no transmisibles asociadas a esta. Fecha de consulta: 6 de junio de 2017. Disponible en: http://www.dmsjuridica.com/CODIGOS/LEGISLACION/LEYES/2009/LEY_1355_DE_2009.htm
Report of the Commission on Ending Childhood Obesity. Implementation plan: Executive summary. Geneva: World Health Organization; 2017. Fecha de consulta: 30 de enero de 2018. Disponible en: http://apps.who.int/iris/bitstream/10665/259349/1/WHO-NMH-PNDECHO-17.1-eng.pdf
Mead E, Brown T, Rees K, Azevedo LB, Whittaker V, Jones D, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years. Cochrane Database Syst Rev. 2017;6:CD012651. https://doi.org/10.1002/14651858
Al-Khudairy L, Loveman E, Colquitt JL, Mead E, Johnson RE, Fraser H, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese adolescents aged 12 to 17 years. Cochrane Database Syst Rev. 2017;6:CD012691. https://doi.org/10.1002/14651858
Patiño FA, Márquez JJ, Uscátegui RM, Estrada-Restrepo A, Agudelo-Ochoa GM, Manjarrés LM, et al. Efecto de una intervención con ejercicio físico y orientación nutricional sobre componentes del síndrome metabólico en jóvenes con exceso de peso. Iatreia. 2013;26:34-43.
van der Heijden LB, Feskens EJ, Jansel AJ. Maintenance interventions in overweight or obese children: A systematic review and meta-analysis. Obes Rev. 2018;19:798-809. https://doi.org/10.1111/obr.12664
Ministerio de la Protección Social. Resolución 2121 de 2010. Por la cual se adoptan los patrones de crecimiento publicados por la Organización Mundial de la Salud, OMS, en el 2006 y 2007 para los niños, niñas y adolescentes de 0 a 18 años de edad y se dictan otras disposiciones. Fecha de consulta: 30 de enero de 2018. Disponible en: https://www.icbf.gov.co/cargues/avance/docs/resolucion_minproteccion_2121_2010.htm
Ford ES, Ajani UA, Mokdad AH. The metabolic syndrome and concentrations of C-reactive protein among U.S. youth. Diabetes Care. 2005;28:878-88. https://doi.org/10.2337/diacare.28.4.878
American Diabetes Association. Children and adolescents: Standards of medical care in diabetes 2018. Diabetes Care. 2018;41(Suppl.1):S126-36 . https://doi.org/10.2337/dc18-S012
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(Suppl.):555-76.
Gussinyer S, García-Reyna NI, Carrascosa A, Gussinyer M, Yeste D, Clemente M, et al. Cambios antropométricos, dietéticos y psicológicos tras la aplicación del programa “Niñ@s en movimiento” en la obesidad infantil. Med Clin. 2008;131:245-9. https://doi.org/10.1016/S0025-7753(08)72243-7
Chen MJ, Fan X, Moe ST. Criterion-related validity of the Borg ratings of perceived exertion scale in healthy individuals: A meta-analysis. J Sports Sci. 2002;20:873-99. https://doi.org/10.1080/026404102320761787
Cook S, Auinger P, Huang TT. Growth curves for cardio-metabolic risk factors in children and adolescents. J Pediatr. 2009;155:S6.e15-26. https://doi.org/10.1016/j.jpeds.2009.04.051
Zimmet P, Alberti KG, Kaufman F, Tajima N, Silink M, Arslanian S, et al. The metabolic syndrome in children and adolescents - an IDF consensus report. Pediatr Diabetes. 2007;8:299-306. https://doi.org/10.1111/j.1399-5448.2007.00271.x
Druet C, Ong K, Levy Marchal C. Metabolic syndrome in children: Comparison of the International Diabetes Federation 2007 consensus with an adapted National Cholesterol Education Program definition in 300 overweight and obese French children. Horm Res Paediatr. 2010;73:181-6. https://doi.org/10.1159/000284359
Matsha T, Hassan S, Bhata A, Yako Y, Fanampe B, Somers A, et al. Metabolic syndrome in 10-16-year-old learners from the Western Cape, South Africa: Comparison of the NCEP ATP III and IDF criteria. Atherosclerosis. 2009;205:363-6. https://doi.org/10.1016/j.atherosclerosis.2009.01.030
National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents. Pediatrics. 2011;128 S5:213-56. https://doi.org/10.1542/peds.2009-2107C
Agudelo GM, Bedoya G, Estrada A, Patiño FA, Muñoz AM, Velásquez CM. Variations in the prevalence of metabolic syndrome in adolescents according to different criteria used for diagnosis: Which definition should be chosen for this age group? Metab Syndr Relat Disord. 2014;12:202-9. https://doi.org/10.1089/met.2013.0127
National Health and Nutrition Examination Survey. Anthropometry Procedures Manual. Fecha de consulta: 30 de enero de 2018. Disponible en: https://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_an.pdf
Organización Mundial de la Salud. OMS Anthro (versión 3.2.2, enero de 2011) y macros. Fecha de consulta: 3 de junio de 2015. Disponible en: http://www.who.int/childgrowth/software/es/
Snethen JA, Broome ME, Treisman P, Castro E, Kelber ST. Effective weight loss for children: A meta-analysis of intervention studies 2002-2015. Worldviews Evid Based Nurs. 2016;13:294-302. https://doi.org/10.1111/wvn.12156
Rosado JL, Del R Arellano M, Montemayor K, García OP, Caamaño M. An increase of cereal intake as an approach to weight reduction in children is effective only when accompanied by nutrition education: A randomized controlled trial. Nutr J. 2008;7:28. http://doi.org/10.1186/1475-2891-7-28
Farpour-Lambert NJ, Aggoun Y, Marchand LM, Martin XE, Herrmann FR, Beghetti M. Physical activity reduces systemic blood pressure and improves early markers of atherosclerosis in pre-pubertal obese children. J Am Coll Cardiol. 2009;54:2396-406. https://doi.org/10.1016/j.jacc.2009.08.030
Maddison R, Foley L, Ni Mhurchu C, Jiang Y, Jull A, Prapavessis H, et al. Effects of active video games on body composition: A randomized controlled trial. Am J Clin Nutr. 2011;94:156-63. https://doi.org/10.3945/ajcn.110.009142
Wong EM, Cheng MM. Effects of motivational interviewing to promote weight loss in obese children. J Clin Nurs. 2013;22:2519-30. https://doi.org/10.1111/jocn.12098
Davis JN, Ventura EE, Cook LT, Gyllenhammer LE, Gatto NM. LA Sprouts: A gardening, nutrition, and cooking intervention for Latino youth improves diet and reduces obesity. J Am Diet Assoc. 2011;111:1224-30. https://doi.org/10.1016/j.jada.2011.05.009
Harder-Lauridsen NM, Birk NM, Ried-Larsen M, Juul A, Andersen LB, Pedersen BK, et al. A randomized controlled trial on a multicomponent intervention for overweight school-aged children-Copenhagen, Denmark. BMC Pediatr. 2014;14:273. https://doi.org/10.1186/1471-2431-14-273
Adam S, Westenhofer J, Rudolphi B, Kraaibeek HK. Effects of a combined inpatientoutpatient treatment of obese children and adolescents. Obes Facts. 2009;2:286-93. https://doi.org/10.1159/000234415
Croker H, Viner R, Nicholls D, Haroun D, Chadwick P, Edwards C, et al. Family-based behavioural. Treatment of childhood obesity in a UK National Health Service setting: Randomized controlled trial. Int J Obes. 2012;36:16-26. https://doi.org/10.1038/ijo.2011.182
Maddison R, Marsh S, Foley L, Epstein LH, Olds T, Dewes O, et al. Screen-Time Weightloss Intervention Targeting Children at Home (SWITCH): A randomized controlled trial. Int J Behav Nutr Phys Act. 2014,11:111. https://doi.org/10.1186/s12966-014-0111-2
Reinehr T, Schaefer A, Winkel K, Finne E, Toschke AM, Kolip P. An effective lifestyle intervention in overweight children: Findings from a randomized controlled trial on “Obeldicks light.” Clin Nutr. 2010;29:331-6. https://doi.org/10.1016/j.clnu.2009.12.010
Sacher PM, Kolotourou M, Chadwick PM, Cole TJ, Lawson MS, Lucas A, et al. Randomized controlled trial of the MEND program: A family-based community intervention for childhood obesity. Obesity. 2010;18:S62-8. https://doi.org/10.1038/oby.2009.433
Reinehr T, Hoffmeister U, Mann R, Goldap C, Westenho J, Egmond A, et al. Medical care of overweight children under real-life conditions: The German BZgA obsrvation study. Int J Obesity. 2009;33:418-23. https://doi.org/10.1038/ijo.2009.50
Hampl S, Odar-Stough C, Poppert-Cordts K, Best C, Blackburn K, Dreyer-Gillette ML. Effectiveness of a hospital-based multidisciplinary pediatric weight management program: Twoyear outcomes of PHIT kids. Child Obes. 2016;12:20-5. https://doi.org/10.1089/chi.2014.0119
National Academies of Sciences, Engineering, and Medicine. Driving action and progress on obesity prevention and treatment: Proceedings of a workshop. 2017. Washington, DC: The National Academies Press; 2017. https://doi.org/10.17226/24734
Rajjo T, Mohammed K, Alsawas M, Ahmed AT, Farah W, Asi N, et al. Treatment of pediatric obesity: An umbrella systematic review. J Clin Endocrinol Metab. 2017;102:763-75. https://doi.org/10.1210/jc.2016-2574
Bray GA, Heisel WE, Afshin A, Jensen MD, Dietz WH, Long M, et al. The science of obesity management: An Endocrine Society Scientific statement. Endocr Rev. 2018;39:79-132. https://doi.org/10.1210/er.2017-00253
Reinehr T. Lifestyle intervention in childhood obesity: Changes and challenges. Nat Rev Endocrinol. 2013;9:607-14. https://doi.org/10.1038/nrendo.2013.149
Kiess W, Wabitsch M, Maffeis C, Sharma AM. Metabolic syndrome and obesity in childhood and adolescence. Pediatr Adolesc Med. 2015;19:171-8. https://doi.org/10.1159/000368134
Mameli C, Zuccotti GV, Carnovale C, Galli E, Nannini P, Cervia D, et al. An update on the assessment and management of metabolic syndrome, a growing medical emergency in paediatric populations. Pharmacol Res. 2017;119:99-117. https://doi.org/10.1016/j.phrs.2017.01.017
Andersen LB, Lauersen JB, Brønd JC, Anderssen SA, Sardinha LB, Steene-Johannessen J, et al. A new approach to define and diagnose cardiometabolic disorder in children. J Diabetes Res. 2015;2015:539-835. https://doi.org/10.1155/2015/539835
Ahrens W, Moreno LA, Mårild S, Molnár D, Siani A, De Henauw S, et al. Metabolic syndrome in young children: Definitions and results of the IDEFICS study I; IDEFICS consortium. Int J Obes. 2014;38(Suppl.2):S4-14. https://doi.org/10.1038/ijo.2014.130
Hesse MB, Young G, Murray RD. Evaluating health risk using a continuous metabolic syndrome score in obese children. J Pediatr Endocrinol Metab. 2016;29:451-8. https://doi.org/10.1515/jpem-2015-0271
Eisenmann JC. On the use of a continuous metabolic syndrome score in pediatric research. Cardiovasc Diabetol. 2008;5;7:17. https://doi.org/10.1186/1475-2840-7-17
American Diabetes Association. Classification and diagnosis of diabetes: Standards of medical care in diabetes-2018. Diabetes Care. 2018;41(Suppl.1):S13-S27. https://doi.org/10.2337/dc18-S002
Stelmach-Mardas M, Walkowiak J. Dietary interventions and changes in cardio-metabolic parameters in metabolically healthy obese subjects: A systematic review with meta-analysis. Nutrients. 2016;8:E455. https://doi.org/10.3390/nu8080455
Serra PN, Ensenyat A, Castro VI, Real J, Sinfreu BX, Zapata A, et al. Effectiveness of a multi-component intervention for overweight and obese children (Nereu Program): A randomized controlled trial. PLoS ONE. 2015;10:e0144502. https://doi.org/10.1371/journal.pone.0144502
Aguilar MJ, Ortegón A, Baena L, Noack JP, Levet MC, Sánchez AM. Rebound effect of intervention programs to reduce overweight and obesity in children and adolescents; systematic review. Nutr Hosp. 2015;32:2508-17. https://doi.org/10.3305/nh.2015.32.6.10071
Curilem C, Almagia A, Rodríguez F, Yuing T, Berral de la Rosa F, Martínez C, et al. Evaluación de la composición corporal en niños y adolescentes: directrices y recomendaciones. Nutr Hosp. 2016;33:734-8. https://doi.org/10.20960/nh.285
Some similar items:
- Greta Rodríguez-Arroyo, Irene Paradisi, Merlyn Vívenes-Lugo, Dinorah Castro-Guerra, Álvaro Rodríguez-Larralde, LEP, LDLR and APOA4 gene polymorphisms and their relationship with the risk of overweight, obesity and chronic diseases in adults of the State of Sucre, Venezuela , Biomedica: Vol. 36 No. 1 (2016)
- Ana C. Orozco, Angélica M. Muñoz, Claudia M. Velásquez, Rosa M. Uscátegui, María V. Parra, Fredy A. Patiño, Luz M. Manjarres, Beatriz E. Parra, Alejandro Estrada, Gloria M. Agudelo, Variant in CAPN10 gene and environmental factors show evidence of association with excess weight among young people in a Colombian population , Biomedica: Vol. 34 No. 4 (2014)
- Constanza Palomino-Devia, Felipe Augusto Reyes-Oyola, Antonio Jesús Sánchez-Oliver, Levels of physical activity, health-related quality of life, physical self-concept and body-mass index among Colombian students , Biomedica: Vol. 38 No. 2 (2018)
- Ana Yibby Forero , Gina Emely Morales , Luis Carlos Forero, Relationship between physical activity, sedentarism and obesity in adults, Colombia, 2015 , Biomedica: Vol. 43 No. Sp. 3 (2023): Enfermedades crónicas no transmisibles
- Ricardo Sánchez, Heidy Cáceres, Dora Gómez, Suicidal ideation among university adolescents: prevalence and associated factors. , Biomedica: Vol. 22 (2002): Suplemento 2
- Álvaro J. Ruiz, Pablo J. Aschner, María Fernanda Puerta, Rafael Alfonso-Cristancho, IDEA Study (International Day for the Evaluation of Abdominal Obesity): Primary care study of the prevalence of abdominal obesity and associated risk factors in Colombia , Biomedica: Vol. 32 No. 4 (2012)
- Liliana Franco-Hincapié, Constanza Elena Duque, María Victoria Parra, Natalia Gallego, Alberto Villegas, Andrés Ruiz-Linares, Gabriel Bedoya, Association between polymorphism in uncoupling proteins and type 2 diabetes in a northwestern Colombian population , Biomedica: Vol. 29 No. 1 (2009)
- Luis Eduardo Echeverría, Clara Saldarriaga, Sebastián Campbell-Quintero, Lisbeth Natalia Morales-Rodríguez, Juan David López-Ponce de León, Andrés Felipe Buitrago, Erika Martínez-Carreño, Jorge Alberto Sandoval-Luna, Alexis Llamas, Gustavo Adolfo Moreno-Silgado, Julián Vanegas-Eljach, Nelson Eduardo Murillo-Benítez, Ricardo Gómez-Paláu, Alex Arnulfo Rivera-Toquica, Juan Esteban Gómez-Mesa, RECOLFACA research group, Diabetes mellitus in patients with heart failure and effect modification of risk factors for short-term mortality: An observational study from the Registro Colombiano de Falla Cardíaca (RECOLFACA) , Biomedica: Vol. 44 No. Sp. 1 (2024): Enfermedades crónicas no transmisibles
- Juan Carlos Aristizábal, María Teresa Restrepo, Amalia López, Validation by hydrodensitometry of skinfold thickness equations used for female body composition assessment , Biomedica: Vol. 28 No. 3 (2008)
- Ligia Inés Moncada, Sandra Milena Rios, Julián Alfredo Fernández, Fabio Rivas, María Luz Sáenz, Pediculosis prevalence and associated risk factors in a nursery school, Bogotá, Colombia , Biomedica: Vol. 28 No. 2 (2008)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























