Genotyping, levels of expression and physical status of human papilloma virus in oropharyngeal squamous cell carcinoma among Colombian patients
Abstract
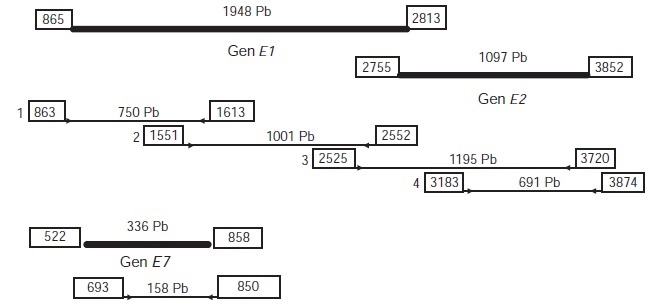
Introduction: One of the risk factors for squamous cell oropharyngeal carcinoma is infection with the human papilloma virus (HPV), with prevalences that vary depending on the geographical region. Objective: To identify the most frequent HPV viral types in oropharyngeal cancer, the levels of expression and the physical condition of the viral genome. Materials and methods: Forty-six patients were included in the study from among those attending head and neck surgical services in the cities of Bogotá, Manizales and Bucaramanga. In the histopathological report all study samples were characterized as oropharyngeal squamous cell carcinoma. DNA extraction was subsequently performed for HPV genotyping and to determine the physical state of the viral genome, as well as RNA to determine viral transcripts using real-time PCR. Results: HPV prevalence in tumors was 21.74% (n=10) and the most common viral type was HPV-16 (nine cases). Viral expression for HPV-16 was low (one of 11 copies) and the predominant physical state of the virus was mixed (eight cases), with disruption observed at the E1 - E2 binding site (2525 – 3720 nucleotides). Conclusion: The prevalence of HPV associated with oropharyngeal carcinoma among the Colombian study population was 21.7%, which is relatively low. The most frequent viral type was HPV-16, found in a mixed form and with low expression of E7, possibly indicating a poor prognosis for these patients.
Downloads
References
BarnesL, Eveson JW, Reichart P, Sidransky D. World Health Organization Classification of tumours. Pathology and Genetics of Head and Neck Tumours. Lyon: IARC Press; 2005. p. 168-75.
Westra WH. The morphologic profile of HPV-related head and neck squamous carcinoma: Implications for diagnosis, prognosis, and clinical management. Head Neck Pathol. 2012;6:48-54. http://dx.doi.org/10.1007/s12105-012-0371-6
Woods R, O’Regan EM, Kennedy S, Martin C, O’Leary JJ, Timon C. Role of human papillomavirus in oropharyngeal squamous cell carcinoma: A review. World J Clin Cases. 2014;2:172-93. http://dx.doi.org/10.12998/wjcc.v2.i6.172
Chaturvedi AK, Engels EA, Anderson WF, Gillison ML. Incidence trends for human papillomavirus-related and -unrelated oral squamous cell carcinomas in the United States. J Clin Oncol. 2008;26:612-9. http://dx.doi.org/10.1200/JCO.2007.14.1713
International Agency for Research on Cancer. GLOBOCAN 2012. Estimated cancer incidence, mortality and prevalence worldwide in 2012. Fecha de consulta: 20 de febrero de 2015. Disponible en: http://globocan.iarc.fr/Pages/fact_sheets_population.aspx.
van Monsjou HS, Balm AJ, Brekel MM, Wreesmann VB. Oropharyngeal squamous cell carcinoma: A unique disease on the rise?. Oral Oncol. 2010;46:780-5. http://dx.doi.org/10.1016/j.oraloncology.2010.08.011
Genden EM, Sambur IM, de Almeida JR, Posner M, Rinaldo A, Rodrigo JP, et al. Human papillomavirus and oropharyngeal squamous cell carcinoma: What the clinician should know. Eur Arch Otorhinolaryngol. 2013;270:405-16. http://dx.doi.org/10.1007/s00405-012-2086-4
Hafkamp HC, Manni JJ, Speel EJ. Role of human papillomavirus in the development of head and neck squamous cell carcinomas. Acta Otolaryngol. 2004;124: 520-6.
Nichols AC, Dhaliwal SS, Palma DA, Basmaji J, Chapeskie C, Dowthwaite S, et al. Does HPV type affect outcome in oropharyngeal cancer? J Otolaryngol Head Neck Surg. 2013;42:1-9. http://dx.doi.org/10.1186/1916-0216-42-9
Evans M, Newcombe R, Fiander A, Powell J, Rolles M, Thavaraj S, et al. Human papillomavirus-associated oropharyngeal cancer: An observational study of diagnosis, prevalence and prognosis in a UK population. BMC Cancer. 2013;13:1-10. http://dx.doi.org/10.1186/1471-2407-13-220
Machiels JP, Lambrecht M, Hanin FX, Duprez T, Gregoire V, Schmitz S, et al. Advances in the management of squamous cell carcinoma of the head and neck. F1000prime Rep. 2014;6:44. http://dx.doi.org/10.12703/P6-44
Ndiaye C, Mena M, Alemany L, Arbyn M, Castellsagué X, Laporte L, et al. HPV DNA, E6/E7 mRNA, and p16INK4a detection in head and neck cancers: A systematic review and meta-analysis. Lancet Oncol. 2014;15:1319-31. http://dx.doi.org/ 10.1016/S1470-2045(14)70471-1
Quintero K, Giraldo GA, Uribe ML, Baena A, López C, Alvarez E, et al. Human papillomavirus types in cases of squamous cell carcinoma of head and neck in Colombia. Braz J Otorhinolaryngol. 2013;79:375-81. http://dx.doi.org/10.5935/1808-8694.20130065
Schmitt M, Dondog B, Waterboer T, Pawlita M. Homogeneous amplification of genital human alpha papillomaviruses by PCR using novel broad-spectrum GP5+ and GP6+ primers. J Clin Microbiol. 2008;46:1050-9. http://dx.doi.org/10.1128/JCM.02227-07
Muñoz N, Bosch FX, de San José S, Herrero R, Castellsagué X, Shah KV, et al. Epidemiologic classifica-tion of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003;348:518-27. http://dx.doi.org/10.1056/NEJMoa021641
de Villiers EM, Fauquet C, Broker TR, Bernard HU, zur Hausen H. Classification of papillomaviruses. Virology. 2004;324:17-27. http://dx.doi.org/10.1016/j.virol. 2004.03.033
Marklund L, Hammarstedt L. Impact of HPV in Oropharyngeal Cancer. J Oncol. 2011;2011:1-6. http://dx.doi.org/10.1155/2011/509036
Betiol J, Villa LL, Sichero L. Impact of HPV infection on the development of head and neck cancer. Braz J Med Biol Res. 2013;46:217-26. http://dx.doi.org/10.1590/1414-431X20132703
Wittekindt C, Wagner S, Mayer CS, Klussmann JP. Basics of tumor development and importance of human papilloma virus (HPV) for head and neck cancer. GMS Curr TopOtorhinolaryngol Head Neck Surg. 2012;11:1-29. http://dx.doi.org/10.3205/cto000091
Castillo A. HPV infection and carcinogenesis in the upper aero-digestive tract. Colomb Med. 2011;42:233-42.
Feller L, Wood NH, Khammissa NA, Lemmer J. Human papillomavirus mediated carcinogenesis and HPV-associated oral and oropharyngeal squamous cell carcinoma. Part 1: Human papillomavirus-mediated carcinogenesis. Head Face Med. 2010;6:1-5. http://dx.doi.org/10.1186/1746-160X-6-15.
Narisawa-Saito M, Kiyono T. Basic mechanisms of high-risk human papillomavirus-induced carcinogenesis: Roles of E6 and E7 proteins. Cancer Sci. 2007;98:1505-11. http://dx.doi.org/10.1111/j.1349-7006.2007.00546.x
Bisht M, Bist SS. Human papilloma virus: A new risk factor in a subset of head and neck cancers. J Cancer Res Ther. 2011;7:251-5. http://dx.doi.org/10.4103/0973-1482.87004
Montalvo M, Resendiz M, Santos G, Vallejo V, Reyes J, Hernández J. Estandarización de un método de detección molecular del virus influenza (H5N1) de alta patogenicidad. Acta Bioquím Clín Latinoam. 2009;43:49-52.
Lukaszuk K, Liss J, Wozniak I, Emerich J, Wójcikowski C. Human papillomavirus type 16 status in cervical carcinoma cell DNA assayed by multiplex PCR. J Clin Microbiol. 2003;41:608-12. http://dx.doi.org/10.1128/JCM.41.2.608-612.2003
Shukla S, Mahata S, Shishodia G, Pande S, Verma G, Hedau S, et al. Physical state & copy number of high risk human papillomavirus type 16 DNA in progression of cervical cancer. Indian J Med Res. 2014;139:531-43.
Steinau M, Saraiya M, Goodman MT, Peters ES, Watson M, Cleveland JL, et al. Human papillomavirus prevalence in oropharyngeal cancer before vaccine introduction, United States. Emerg Infect Dis. 2014;20:822-8. http://dx.doi.org/10.3201/eid2005.131311
Marur S, D’Souza G, Westra WH, Forastiere AA. HPV-associated head and neck cancer: A virus-related cancer epidemic. Lancet Oncol. 2010;11:781-9. http://dx.doi.org/10.1016/S1470-2045(10)70017-6
D’Souza G, Kreimer A, Viscidi R, Pawlita M, Fakhry C, Koch WM, et al. Case-control study of human papillomavirus and oropharyngeal cancer. N Eng J Med. 2007;356:1944-56. http://dx.doi.org/10.1056/NEJMoa065497
Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tân PF, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Eng J Med. 2010;363:24-35. http://dx.doi.org/10.1056/NEJMoa 0912217
Kreimer AR, Clifford GM, Boyle P, Franceschi S. Human papillomavirus types in head and neck squamous cell carcinomas worldwide: A systematic review. Cancer Epidemiol Biomarkers Prev. 2005;14:467-75. http://dx.doi.org/10.1158/1055-9965.EPI-04-0551
Badaracco G, Rizzo C, Mafera B, Pichi B, Giannarelli D, Rahimi SS, et al. Molecular analyses and prognostic relevance of HPV in head and neck tumours. Oncol Rep. 2007;17:931-9. http://dx.doi.org/10.3892/or.17.4.931
Baboci L, Boscolo-Rizzo P, Holzinger D, Bertorelle R, Biasini L, Michel A, et al. Evidence of the causal role of human papillomavirus type 58 in an oropharyngeal carcinoma. Virol J. 2013;10:1-6. http://dx.doi.org/10.1186/ 1743-422X-10-334
Jung AC, Briolat J, Millon R, de Reyniès A, Rickman D, Thomas E, et al. Biological and clinical relevance of trasncriptionally active human papillomavirus (HPV) infection in oropharynx squamous cell carcinoma. Int J Cancer. 2010;126:1882-94. http://dx.doi.org/10.1002/ijc.24911
Holzinger D, Schmitt M, Dyckhoff G, Benner A, Pawlita M, Bosch FX. Viral RNA patterns and high viral load reliably define oropharynx carcinomas with active HPV16 involvement. Cancer Res. 2012;72:4993-5003. http://dx.doi.org/10.1158/0008-5472.CAN-11-3934
Rietbergen M, Braakhuis B, Moukhtari N, Bloemena E, Brink A, Sie D, et al. No evidence for active human papillomavirus (HPV) in fields surrounding HPV-positive oropharyngeal tumors. J Oral Pathol Med. 2014;43:137-42. http://dx.doi.org/10.1111/jop.12123
Lewis JS, Ukpo OC, Ma XJ, Flanagan JJ, Luo Y, Thorstad WL, et al. Transcriptionally-active high-risk human papillomavirus is rare in oral cavity and laryngeal/hypopharyngeal squamous cell carcinomas –a tissue microarray study utilizing E6⁄E7 mRNA in situ hybridization. Histopathology. 2012;60:982-91. http://dx.doi.org/10.1111/j.1365-2559.2011.04169.x
Jeon SY, Lambert PF. Integration of human papillomavirus type 16 DNA into the human genome leads to increased stability of E6 and E7 mRNAs: Implications for cervical carcinogenesis. Proc Natl Acad Sci USA. 1995;92:1654-8.
Olthof NC, Speel EM, Kolligs J, Haesevoets A, Henfling M, Ramaekers FC, et al. Comprehensive analysis of HPV16 integration in OSCC reveals no significant impact of physical status on viral oncogene and virally disrupted human gene expression. PloS One. 2014;9:1-8. http://dx.doi.org/10.1371/journal.pone.0088718
Mellin H, Dalhgren L, Munck-Wikland E, Lindholm J, Rabbani H, Kalantari M, et al. Human papillomavirus type 16 is episomal and a high viral load may be correlated to better prognosis in tonsillar cancer. Int J Cancer. 2002; 102:152-8. http://dx.doi.org/10.1002/ijc.10669
Some similar items:
- Mercedes Salcedo-Cifuentes, Jesús Cabrera, Yesid Cuesta-Astroz, Edwin Carrascal, Yoshito Eizuru, Martha C. Domínguez, Adalberto Sánchez, Felipe García-Vallejo, Clonal expansion and genomic characterization of the human T-cell lymphotropic virus type I during the integration process in adult T-cell leukemia/lymphoma , Biomedica: Vol. 29 No. 2 (2009)
- Ismael Reyes, Raj Tiwari, Jan Geliebter, Niradiz Reyes, DNA microarray analysis reveals metastasis-associated genes in rat prostate cancer cell lines , Biomedica: Vol. 27 No. 2 (2007)
- Jenniffer Rodiño, Nataly Rincón, Yudy Alexandra Aguilar, Zulma Vanessa Rueda, Mariana Herrera, Lázaro Agustín Vélez, Microscopic diagnosis of Pneumocystis jirovecii pneumonia in bronchoalveolar lavage and oropharyngeal wash samples of immunocompromised patients with pneumonia , Biomedica: Vol. 31 No. 2 (2011)
- Martha Alejandra Casallas, Carlos Mauricio Calderon, Cushing’s syndrome due to a left adrenal cortical carcinoma with metastasis to the liver and a massive vena cava tumor thrombus , Biomedica: Vol. 32 No. 4 (2012)
- Jesús Orlando Yepes, María Luz Gunturiz, Luis Felipe Henao, María Cristina Navas, Norman Balcázar, Luis Alberto Gómez, Differential display of messenger RNA and identification of selenocysteine lyase gene in hepatocellular carcinoma cells transiently expressing hepatitis C virus core protein. , Biomedica: Vol. 26 No. 2 (2006)
- Alfredo Romero-Rojas, Jario Cuervo-Martínez, Karime Osorio-Arango, Natalia Olaya, Histological variants and prognostic factors of papillary thyroid carcinoma at the Colombian Instituto Nacional de Cancerología, 2006-2012 , Biomedica: Vol. 35 No. 3 (2015)
- Marcela Gaviria-Calle, Alejandra Duque-Jaramillo, Mateo Aranzazu, Diana di Filippo, Melissa Montoya, Ingrid Roldán, Natalia Palacio, Sergio Jaramillo, Juan Carlos Restrepo, Sergio Hoyos, María Cristina Navas, Polymorphisms in alcohol dehydrogenase (ADH1) and cytochrome p450 2E1 (CYP2E1) genes in patients with cirrhosis and/or hepatocellular carcinoma , Biomedica: Vol. 38 No. 4 (2018)
- Javier Hernández , Ana Ruiz , Carolina Mesa , Lina Rodríguez , Verrucous psoriasis in a male patient with a history of vulgar psoriasis: Case report and literature review , Biomedica: Vol. 41 No. 3 (2021)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























