Epidemiology of congenital heart diseases in Bogotá, Colombia, from 2001 to 2014: Improved surveillance or increased prevalence?
Abstract
Introduction: Congenital heart diseases are functional and structural alterations of the heart, circulatory system, and large vessels, which develop during cardiac embryogenesis. These defects are significant causes of morbidity and mortality in children worldwide.
Objective: To determine the prevalence of congenital heart diseases in Bogotá, Colombia, through the period 2001 to 2014 and evaluate the trend in time.
Materials and methods: We analyzed 405,408 births from the Programa de Vigilancia y Seguimiento de Niños con Anomalías Congénitas de la Secretaría Distrital de Salud de Bogotá. We calculated the prevalence of congenital heart diseases through a daily registry of births, the clinical evaluation, and the work-up. Congenital heart diseases were classified as isolated, complex or associated. We estimated the prevalence per year and the mortality in the first hours of life.
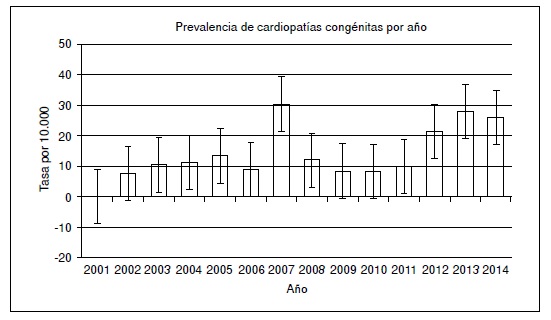
Results: The total prevalence of congenital heart diseases was 15.1 per 10,000 newborns; however, we obtained values above 20 per 10,000 newborns in the previous 3 years. Of the newborns analyzed, 46% were females, 53.16% were males, and 0.33% undetermined. Out of the newborns with congenital anomalies, 397 had congenital heart diseases, 142 of which were classified as associated and 74 as complex.
Conclusion: Congenital heart diseases have a significant impact on childhood morbidity and mortality. Although the prevalence continues to be low compared to other countries, this could be due to under registry nationwide. There was an increase in prevalence during the previous three years, which might be explained by the implementation of local and national programs. Therefore, we suggest continuing the development and promotion of such programs aimed at increasing screening and registration of these anomalies.
Downloads
References
van der Linde D, Konings EE, Slager MA, Witsenburg M, Helbing WA, Takkenberg JJ, et al. Birth prevalence of congenital heart disease worldwide: A systematic review and meta-analysis. J Am Coll Cardiol. 2011;58:2241-7. https://doi.org/10.1016/j.jacc.2011.08.025
Bosi G, Garani G, Scorrano M, Calzolari E. Temporal variability in birth prevalence of congenital heart defects as recorded by a general birth defects registry. J Pediatr. 2003;142:690-8. https://doi.org/10.1067/mpd.2003.243
Edler I, Lindstrom K. The history of echocardiography. Ultrasound Med Biol. 2004;30:1565-644. https://doi.org/10.1016/S0301-5629(99)000563
Borghi A, Ciuffreda M, Quattrociocchi M, Preda L. The grown-up congenital cardiac patient. J Cardiovasc Med (Hagerstown). 2007;8:78-82. https://doi.org/10.2459/01.JCM.0000247441.79644.4b
Barros TL, Dias Mde J, Nina RV. Congenital cardiac disease in childhood x socioeconomic conditions: A relationship to be considered in public health? Rev Bras Cir Cardiovasc. 2014;29:448-54. https://doi.org/10.5935/1678-9741.20140042
Pinto Júnior VC, Branco KM, Cavalcante RC, Carvalho Junior W, Lima JR, Freitas SM, et al. Epidemiology of congenital heart disease in Brazil. Rev Bras Cir Cardiovasc. 2015;30:219-24. https://doi.org/10.5935/1678-9741.20150018
Nazer HJ, Cifuentes OL. Congenital malformations in Latin America in the period 1995-2008. Rev Med Chil. 2011;139: 72-8. https://doi.org/10.4067/S003498872011000100010
Zarante I, Franco L, López C, Fernández N. Frecuencia de malformaciones congénitas: evaluación y pronóstico de 52.744 nacimientos en tres ciudades colombianas. Biomédica.
;30:65-71. https://doi.org/10.7705/biomedica.v30i1.154
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095-128. https://doi.org/10.1016/S0140673612617280
Samanek M. Children with congenital heart disease: Probability of natural survival. Pediatr Cardiol.1992;13:152-8. https://doi.org/10.1007/BF00793947
Ministerio de Salud de Colombia. Guía de detección de anomalías congénitas. Fecha de consulta: 12 de mayo de 2016. Disponible en: http://gpc.minsalud.gov.co/guias/Pages/Gu%C3%ADa-de-anomal%C3%ADascong%C3%A9nitas.aspx
Sandoval N. Congenital heart disease in Colombia and Worldwide. Rev Col Cardiol. 2015;22:1-2. https://doi.org/10.1016/j.rccar.2015.03.005
Christianson A, Howson C, Modell B. March of Dimes Global report on birth defect: The hidden toll of dying and disabled children. White Plains, New York: March of Dimes; 2006. p. 2-65.
EUROCAT. European surveillance of congenital anomalies. Fecha de consulta: 23 de mayo de 2016. Disponible en: http://www.eurocat-network.eu/accessprevalencedata/prevalencetables
Reller MD, Strickland MJ, Riehle-Colarusso T, Mahle WT, Correa A. Prevalence of congenital heart defects in metropolitan Atlanta, 1998-2005. J Pediatr. 2008;153:807-13. https://doi.org/10.1016/j.jpeds.2008.05.059
Baird PA, Sadovnick AD, Yee IM. Maternal age and birth defects: A population study. Lancet.1991;337:527-30. https://doi.org/10.1016/0140-6736(91)91306-F
Mocumbi AO, Lameira E, Yaksh A, Paul L, Ferreira MB, Sidi D. Challenges on the management of congenital heart disease in developing countries. Int J Cardiol. 2011;148:285-8. https://doi.org/10.1016/j.ijcard.2009.11.006
García A, Caicedo M, Moreno K, Sandoval N, Ronderos M, Dennis R. Diferencias regionales en cardiopatías congénitas. Rev Col Cardiol. 2017;24:161-8. https://doi.org/10.1016/j.rccar.2016.06.012
Villacis C, Becerra D, Negrete L. Adherencia al control prenatal en la clínica de gestantes adolescentes del Hospital de Engativá de Bogotá (tesis). Bogotá: Universidad Nacional de Colombia; 2012. p. 1-65.
Hunter LE, Simpson JM. Prenatal screening for structural congenital heart disease. Nat Rev Cardiol. 2014;11:323-34. https://doi.org/10.1038/nrcardio.2014.34
Guía JM, Bosch V, Castro FJ, Téllez C, Mercader B, Gracián M. Factores influyentes en la evolución de la mortalidad de las cardiopatías congénitas. Estudio sobre 1.216 niños en la Comunidad Autónoma de Murcia. Rev Esp Cardiol. 2001;54:299-306. https://doi.org/10.1016/S0300-8932(01)76312-9
Egbe A, Uppu S, Lee S, Ho D, Srivastava S. Changing prevalence of severe congenital heart disease: A populationbased study. Pediatr Cardiol. 2014;35:1232-8. https://doi.org/10.1007/s00246-014-0921-7
Silva KP, Rocha LA, Leslie AT, Guinsburg R, Silva CM, Nardozza LM, et al. Newborns with congenital heart diseases: Epidemiological data from a single reference center in Brazil. J Prenat Med. 2014;8:11-6.
Rittler M, López-Camelo J, Castilla EE. Sex ratio and associated risk factors for 50 congenital anomaly types: Clues for causal heterogeneity. Birth Defects Res A Clin Mol Teratol. 2004;7013-9. https://doi.org/10.1002/bdra.10131
Khairy P, Ionescu-Ittu R, MacKie AS, Abrahamowicz M, Pilote L, Marelli AJ. Changing mortality in congenital heart disease. J Am Coll Cardiol. 2010;56:1149-57. https://doi.org/10.1016/j.jacc.2010.03.085
Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002;39:1890-900. https://doi.org/10.1016/S0735-1097(02)01886-7
Bialkowski J, Glowacki J, Zabal C, García-Montes A, Bermúdez-Cañete R, Flores-Arizmendi R, et al. Patent ductus arteriosus at low and high altitudes: Anatomical and haemodynamic features and their implications for transcatheter closure. Kardiol Pol. 2011;69:431-6.
Roncancio CP, Misnaza SP, Peña IC, Prieto FE, Cannon MJ, Valencia D. Trends and characteristics of fetal and neonatal mortality due to congenital anomalies, Colombia
-2008. J Matern Fetal Neonatal Med. 2017;1-8. https://doi.org/10.1080/14767058.2017.1326901
Khairy P, Ionescu-Ittu R, MacKie AS, Abrahamowicz M, Pilote L, Marelli AJ. Changing mortality in congenital heart disease. J Am Coll Cardiol. 2010;56:1149-57. https://doi.org/10.1016/j.jacc.2010.03.085
Bower C, Ramsay JM. Congenital heart disease: A 10-year cohort. J Paediatr Child Health. 1994;30:414-8. https://doi.org/10.1111/j.1440-1754.1994.tb00691
Baltaxe E, Zarante I. Prevalencia de malformaciones cardíacas congénitas en 44,985 nacimientos en Colombia. Arch Cardiol Mex. 2006;76:263-8.
Yuan S, Zaidi S, Brueckner M. Congenital heart disease: Emerging themes linking genetics and development. Curr Opin Genet Dev. 2013;23:352-9. https://doi.org/10.1016/j.gde.2013.05.004.
Trevisan P, Rosa RF, Koshiyama DB, Zen TD, Paskulin GA, Zen PR. Congenital heart disease and chromosomopathies detected by the karyotype. Rev Paul Pediatr. 2014;32:262-71. https://doi.org/10.1590/0103-0582201432213213
García MA, Imbachí L, Hurtado PM, Gracia G, Zarante I. Detección ecográfica de anomalías congénitas en 76.155 nacimientos en Bogotá y Cali, 2011-2012. Biomédica. 2014;34:379-86. https://doi.org/10.7705/biomedica.v34i3.2259
Rodríguez-Páez F, Jiménez-Barbosa W, Jiménez-González C, Coral-Córdoba Á, Ramírez-Solano P, Ramos-Navas N. Efecto de las barreras de acceso sobre la asistencia a citas de programa de control prenatal y desenlaces perinatales. Rev Gerenc Polit Salud. 2014;13:212-27. https://doi.org/10.11144/Javeriana.rgyps13-27.ebas
Ministerio de Salud y Protección Social. Lineamiento para la implementación de la Atención Integral en Salud a la primera infancia, infancia y adolescencia. Bogotá: Ministerio
de Salud y Protección Social; 2014. p. 20-6.
Rueda JD, Otálora M, Roselli D. Implicaciones y costoefectividad del alta temprana del binomio madre-hijo después de un parto normal. Revista Medicina. 2015;37:8-16.
Sistema Nacional de Vigilancia en Salud Pública. Programa Nacional de Vigilancia de Defectos Congénitos. Fecha de consulta: 12 de mayo de 2016. Disponible en:
http://www.ins.gov.co/lineas-de-accion/Subdireccion-Vigilancia/sivigila/Paginas/protocolos.aspx
Some similar items:
- Gloria Liliana Porras-Hurtado, Olga Mercedes León-Castañeda, Jaime Molano-Hurtado, Sandra Lorena Quiceno, Harry Pachajoa, Juan José Montoya, Prevalence of birth defects in Risaralda, 2010-2013 , Biomedica: Vol. 36 No. 4 (2016)
- Estephania Candelo, Gabriela Caicedo, Max Feinstein, Harry Pachajoa, Microcephaly in Colombia before the Zika outbreak: A systematic literature review , Biomedica: Vol. 38 No. Sup. 2 (2018): Suplemento 2, Medicina tropical
- Luisa F. Imbachi, Lina M. Ibañez , Paula Hurtado-Villa, Health status and barriers in health care for children with birth defects born between 2011 and 2017 in two institutions in Cali , Biomedica: Vol. 40 No. 1 (2020)
- Sandra Patricia Misnaza, Claudia Patricia Roncancio, Isabel Cristina Peña, Franklin Edwin Prieto, Geographic distribution of perinatal mortality due to congenital malformations in Colombia, 1999-2008: An analysis of vital statistics data , Biomedica: Vol. 36 No. 3 (2016)
- Mary A. García, Luisa Imbachí, Paula M. Hurtado, Gloria Gracia, Ignacio Zarante, Ultrasound detection of congenital anomalies in 76,155 births in the cities of Bogotá and Cali, 2011-2012 , Biomedica: Vol. 34 No. 3 (2014)
- Albenia Lurán, Elizabeth López, Consuelo Pinilla, Pedro Sierra, Mortality by avoidable causes in preschool children , Biomedica: Vol. 29 No. 1 (2009)
- Ligia Inés Moncada, Sandra Milena Rios, Julián Alfredo Fernández, Fabio Rivas, María Luz Sáenz, Pediculosis prevalence and associated risk factors in a nursery school, Bogotá, Colombia , Biomedica: Vol. 28 No. 2 (2008)
- Francisca Monsalve, Leonor Chacín Bonilla, Ricardo José Atencio, Leticia Denys Porto, Luciana Ana Costa León, Jesús Enrique Estévez, Diana Estela Callejas Valero, Low prevalence of hepatitis C virus infection in a prisoner population from Maracaibo, Venezuela , Biomedica: Vol. 29 No. 4 (2009)
- Ignacio Zarante, Liliana Franco, Catalina López, Nicolás Fernández, Frequencies of congenital malformations: assessment and prognosis of 52,744 births in three cities of Colombia , Biomedica: Vol. 30 No. 1 (2010)
- Harry Pachajoa, Arelis Barragán, Javier Torres, Carolina Isaza, Pentalogy of Cantrell: report of a case with consanguineous parents , Biomedica: Vol. 30 No. 4 (2010)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























