Characterization of patients with bacteremia by methicillin-resistant Staphylococcus aureus in a high-complexity military hospital
Abstract
Introduction: In Colombia, there are about 500,000 members in the national armed forces who consult military health institutions. In this population, methicillin-resistant Staphylococcus aureus (MRSA) has become a high-incidence pathogen.
Objective: The aim of this study was to characterize patients with MRSA bacteremia in the Hospital Militar Central between 2012 and 2015.
Materials and methods: This was an observational descriptive study with a retrospective review of clinical histories of hospitalized patients older than 18 years of age with positive blood cultures for methicillin-resistant S. aureus. The identification of the patients was made using the Whonet system, version 5.6.
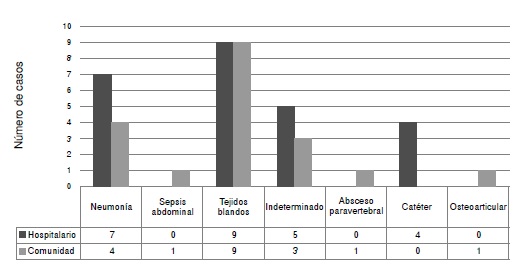
Results: From cultures positive for S. aureus, 24.8% were methicillin-resistant strains, with a higher prevalence in active military personnel. A similar frequency was observed for community-acquired MRSA bacteremias and those acquired at the hospital, with the community phenotype being the most frequent in both groups. The main infectious focus related to the development of bacteremia was soft tissue, followed by pulmonary tissue.
There were higher complication rates in nosocomial bacteremias; 34.9% of the patients had prolonged stays attributable to complications triggered by the bacteremia.
Conclusions: Active military personnel was the most affected population by MRSA, with a similar frequency in community-acquired and nosocomial bacteremias. The main infectious focus was soft tissue. Taking into account these data, studies that establish the prevalence of skin infections by MRSA should be carried out.
Downloads
References
Wang JT, Wang JL, Fang CT, Chie WC, Lai MS, Lauderdale TL, et al. Risk factors for mortality of nosocomial methicillin-resistant Staphylococcus aureus (MRSA) bloodstream infection: With investigation of the potential role of community-associated MRSA strains. J Infect. 2010;61:449-57. https://doi.org/10.1016/j.jinf.2010.09.029
Grupo para el Control de la Resistencia Bacteriana de Bogotá (GREBO). Resultados de la vigilancia de la resistencia bacteriana, año 2016. Componente pediátrico y adulto. Análisis de percentiles marcadores de resistencia 2016. Tendencias de los principales marcadores de resistencia, 2008-2016. Boletín GREBO. 2017;9:1-23.
Jiménez JN, Ocampo AM, Vanegas JM, Rodríguez EA, Mediavilla JR, Chen L, et al. A comparison of methicillin-resistant and methicillin-susceptible Staphylococcus aureus reveals no clinical and epidemiological but molecular differences. Int J Med Microbiol. 2013;303:76-83. https://doi.org/10.1016/j.ijmm.2012.12.003
Gasch O, Camoez M, Domínguez MA, Padilla B, Pintado V, Almirante B, et al. Predictive factors for mortality in patients with methicillin-resistant Staphylococcus aureus bloodstream infection: Impact on outcome of host, microorganism and therapy. Clin Microbiol Infect. 2013;19:1049-57. https://doi.org/10.1111/1469-0691.12108
Naber CK. Staphylococcus aureus bacteremia: Epidemiology, pathophysiology, and management strategies. Clin Infect Dis. 2009;48(Suppl.4):S231-7. https://doi.org/10.1086/598189
Chong YP, Park S, Kim HS, Kim ES, Kim M, Park K, et al. Persistent Staphylococcus aureus bacteremia, a prospective analysis of risk factors, outcomes and microbiologic and genotypic characteristics of isolates. Medicine (Baltimore). 2013;92:98-108. https://doi.org/10.1097/MD.0b013e318289ff1e
Lam SW, Bauer SR, Neuner EA. Predictors of septic shock in patients with methicillin resistant Staphylococcus aureus bacteremia. Int J Infect Dis. 2012;16:e453-6. https://doi.org/10.1016/j.ijid.2012.02.007
Taylor AR. Methicillin-resistant Staphylococcus aureus infections. Prim Care. 2008;16:637-54. https://doi.org/10.1016/j.pop.2013.06.002
Pastagia M, Kleinman LC, Lacerda EG, Cruz D, Jenkins SG. Predicting risk for death from MRSA bacteriemia. Emerg Infect Dis. 2012;18:1072-80. https://doi.org/10.3201/eid1807.101371
Corey GR. Staphylococcus aureus bloodstream infections: Definitions and treatment. Clin Infect Dis. 2009;27715(Suppl.4):S254-9. https://doi.org/10.1086/598186.11
Naves SK, Vaz N, Pinto P, Filho G. Methicillin-resistant Staphylococcus aureus bloodstream infection: Risk factors and clinical outcome in non-intensive-care units. Rev Soc Bras Med Trop. 2012;45:189-93. https://doi.org/10.1590/S0037-86822012000200010
Popovich K, Hota B, Rice T, Aroutcheva A, Weinstein RA. Phenotypic prediction rule for community-associated methicillin-resistant Staphylococcus aureus. J Clin Microbiol. 2007;45:2293-5. https://doi.org/10.1128/JCM.00044-07
Aiello A, Lowy E, Wright FD, Larson L. Methicillin-resistant Staphylococcus aureus among US prisoners and military personnel: Review and recommendations for future studies. Lancet Infect Dis. 2006;6:335-41. https://doi.org/10.1016/S1473-3099(06)70491-1
Zinderman C, Conner B, Malakooti M, LaMar J, Armstrong A, Bohnker B. Communityacquired methicillin-resistant Staphylococcus aureus among military recruits. Emerg Infect Dis. 2004;10:941-4. https://doi.org/10.3201/eid1005.030604
Washington MA, Agee WA 3rd, Kajiura L, Staege CM, Uyehara CF, Barnhill JC. An analysis of Staphylococcus aureus infections at a military medical center using the PLEX-ID combined polymerase chain reaction-mass spectrometry system. Mil Med. 2014;179:445-50. https://doi.org/10.7205/MILMED-D-13-00472
Vento T, Calvano T, Cole D, Mende K, Rini E, Tully CH, et al. Staphylococcus aureus colonization of healthy military service members in the United States and Afghanistan. BMC Infect Dis. 2013;13:325. https://doi.org/10.1186/1471-2334-13-325
Hospenthal D, Green A, Crouch H, English J, Pool J, Yun H, et al. Infection prevention and control in deployed military medical treatment facilities. J Trauma. 2011;71:S290-8. https://doi.org/10.1097/TA.0b013e318227add8
Braun L, Craft D, Williams R, Tuamokumo F, Ottolini M. Increasing clindamycin resistance among methicillin-resistant Staphylococcus aureus in 57 Northeast United States Military treatment facilities. Pediatr Infect Dis J. 2005;24:622-6. https://doi.org/10.1097/TA.0b013e318227add8
Landrum M, Neumann CH, Cook C, Chukwuma U, Ellis M, Hospenthal D, et al. Epidemiology of Staphylococcus aureus blood and skin and soft tissue infections in the US Military Health System, 2005-2010. JAMA. 2012;308:50-9. https://doi.org/10.1001/jama.2012.7139
Roberts S, Kazragis R. Methicillin-resistant Staphylococcus aureus infections in U.S. service members deployed to Iraq. Mil Med. 2009;174:408.
Sherwood J, Park M, Robben P, Whitman T, Ellis M. USA 300 Methicillin-resistant Staphylococcus aureus. Emerging as a cause of bloodstream infections at military medical centers. Infect Control Hosp Epidemiol. 2013;34:393-9. https://doi.org/10.1086/669866
Whitman TJ, Herlihy RK, Schlett CD, Murray P. Chlorhexidine-impregnated cloths to prevent skin and soft-tissue infection in marine recruits: A cluster-randomized, double-blind, controlled effectiveness trial. Infect Control Hosp Epidemiol. 2010;31:1207-15. https://doi.org/10.1086/657136
Ganesan A, Crawford K, Mende K, Murray C, Lloyd B, Ellis M, et al. Evaluation for a novel methicillin resistance (mecC) homologue in methicillin-resistant Staphylococcus aureus isolates obtained from injured military personnel. J Clin Microbiol. 2013;51:3073-5. https://doi.org/10.1128/JCM.01516-13
Paul M, Kariv G, Goldberg E, Raskin M, Shaked H, Hazzan R, et al. Importance of appropriate empirical antibiotic therapy for methicillin-resistant Staphylococcus aureus bacteraemia. J Antimicrob Chemother. 2010:2658-65. https://doi.org/10.1093/jac/dkq373
Laupland KB, Ross T, Gregson DB. Staphylococcus aureus bloodstream infections: Risk factors, outcomes, and the influence of methicillin resistance in Calgary, Canada, 2000-2006. J Infect Dis. 2008;198:336-43. https://doi.org/10.1086/589717
Arias-Ortiz PM, del Pilar-Calderón L, Castillo JS. Factores de riesgo de la resistencia a meticilina de Staphylococcus aureus causante de bacteriemia: Un estudio multicéntrico de casos y controles emparejados. Biomédica. 2016;36:612-8. https://doi.org/10.7705/biomedica.v36i4.3193
Holland TL, Arnold C, Fowler VG. Clinical management of Staphylococcus aureus bacteremia. JAMA. 2014;312:1330. https://doi.org/10.1001/jama.2014.9743
International Working Group on the Classification of Staphylococcal Cassette Chromosome Elements (IWG-SCC). Classification of Staphylococcal cassette chromosome mec (SCCmec): Guidelines for reporting novel SCCmec elements. Antimicrob Agents Chemother. 2009;53:4961-7. https://doi.org/10.1128/AAC.00579-09
Wang WY, Chiueh TS, Sun JR, Tsao SM, Lu JJ. Molecular typing and phenotype characterization of methicillin-resistant Staphylococcus aureus isolates from blood in Taiwan. PLoS One. 2012;7:e30394. https://doi.org/10.1371/journal.pone.0030394
Gradelski E, Valera L, Aleksunes A, Bonner D, Fung-Tomc J. Correlation between genotype and phenotypic categorization of Staphylococci based on methicillin susceptibility and resistance. J Clin Microbiol. 2001;39: 2961-3. https://doi.org/10.1128/JCM.39.8.2961-2963.2001
Clinical and Laboratory Standards Institute. CLSI Guidelines. Performance Standards for Antimicrobial Susceptibility Testing; Sixteenth Informational Supplement to CLSI Approved Standard M2-A8, Performance Standards for Antimicrobial Disk Susceptibility Tests. Wayne, PA: CLSI; 2016.
López-Cortés LE, de Cueto M, Rodríguez-Baño J. How should we best treat patients with bloodstream infections? Future Microbiol. 2017;12:927-30. https://doi.org/10.2217/fmb-2017-0118
Kaasch A, Fätkenheuer G, Prinz-Langenohl R, Paulus U, Hellmich M, Wei V, et al. Early oral switch therapy in low-risk Staphylococcus aureus bloodstream infection (SABATO): Study protocol for a randomized controlled trial. Trials. 2015;16:450. https://doi.org/10.1186/s13063-015-0973-x
Some similar items:
- Johanna Marcela Vanegas, Luis Felipe Higuita, Carlos Andrés Vargas, Astrid Vanessa Cienfuegos, Erika Andrea Rodríguez, Gustavo Eduardo Roncancio, Judy Natalia Jiménez, Carbapenem-resistant Acinetobacter baumannii causing osteomyelitis and infections of skin and soft tissues in hospitals of Medellín, Colombia , Biomedica: Vol. 35 No. 4 (2015)
- Óscar García , Tatiana Álvarez, Santiago Granados, Vanessa Garzón, Santiago González, Comparison of quick SOFA and SIRS scales at the bedside of patients with Staphylococcus aureus bacteremia , Biomedica: Vol. 40 No. Supl. 1 (2020): Mayo, Infecciones en el trópico
- Paola Mariana Arias-Ortiz, Libia del Pilar Calderón, Juan Sebastián Castillo, José Moreno, Aura Lucía Leal, Jorge Alberto Cortés, Carlos Arturo Álvarez, Grupo GREBO, Risk factors for methicillin-resistant Staphylococcus aureus bacteremia: A multicenter matched case-control study , Biomedica: Vol. 36 No. 4 (2016)
- Liliana I. Barrero, Juan S. Castillo, Aura L. Leal, Ricardo Sánchez, Jorge A. Cortés, Carlos A. Álvarez, Andrés L. González, Economic burden of methicillin-resistant Staphylococcus aureus bacteremia in critical care patients in hospitals in Bogotá , Biomedica: Vol. 34 No. 3 (2014)
- Aura Lucía Leal, María Victoria Ovalle, Jorge Alberto Cortés, Anita María Montañes, Zandra Rocío de la Rosa, José Yesid Rodríguez, Sandra Gualtero, Beatriz Ariza, Otto Sussman, María del Pilar Torres, In vitro activity of tedizolid and other comparator drugs in methicillin-resistant Staphylococcus aureus isolates in skin and soft tissue infections in seven Colombian hospitals , Biomedica: Vol. 38 No. 4 (2018)
- Natalia Andrea Maldonado, María Isabel Múnera, Jaime Alberto López, Patricia Sierra, Carlos Robledo, Jaime Robledo, Grupo GERMEN, Trends in antibiotic resistance in Medellín and municipalities of the Metropolitan Area between 2007 and 2012: Results of six years of surveillance , Biomedica: Vol. 34 No. 3 (2014)
- Leidy González, Jorge Alberto Cortés, Systematic review of antimicrobial resistance in Enterobacteriaceae isolates from Colombian hospitals , Biomedica: Vol. 34 No. 2 (2014)
- María Consuelo Garzón, Dailyn Yorledy Angée, Claudia Llerena, Dora Leticia Orjuela, Jorge Ernesto Victoria, Surveillance of Mycobacterium tuberculosis resistance to antituberculosis drugs , Biomedica: Vol. 28 No. 3 (2008)
- Ana María Perilla, Camilo González, Sandra Liliana Valderrama, Natasha Vanegas, Bibiana Chavarro, Luis Carlos Triana, José Roberto Támara, Carlos Arturo Álvarez, Necrotizing pneumonia by community-acquired, methicillin-resistant Staphylococcus aureus in Colombia , Biomedica: Vol. 29 No. 4 (2009)
- Narda María Olarte, Ismael Alberto Valderrama, Karlo Roberto Reyes, Martha Isabel Garzón, Javier Antonio Escobar, Betsy Esperanza Castro, Natasha Vanegas, Methicillin-resistant Staphylococcus aureus colonization in a Colombian hospital intensive care unit: phenotypic and molecular characterization , Biomedica: Vol. 30 No. 3 (2010)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























