Abandonment of therapy in multidrug-resistant tuberculosis: Associated factors in a region with a high burden of the disease in Perú
Abstract
Introduction: In the context of multidrug-resistant tuberculosis, abandonment of therapy represents a serious public health problem that affects the quality of life of patients, families, and communities. Managing this phenomenon places a burden on health systems since it causes free sources of transmission in the community, thereby increasing prevalence and mortality. Thus, there is a need to study factors associated with this problem.
Objective: This study sought to identify risk factors associated with the abandonment of therapy by patients with multidrug-resistant tuberculosis in the Peruvian region of Callao.
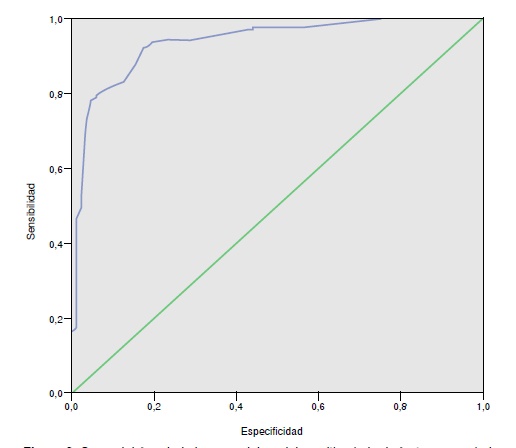
Materials and methods: We conducted an analytical case-control study (cases=80; controls=180) in patients under treatment from January 1st, 2010, to December 31, 2012. Risk factors were identified using logistic regression; odds ratios (OR) and 95% confidence intervals (CI) were calculated.
Results: The multivariate analysis identified the following risk factors: Being unaware of the disease (OR=23.10; 95% CI 3.6-36.79; p=0.002); not believing in healing (OR=117.34; 95% CI 13.57-124.6; p=0.000); not having social support (OR=19.16; 95% CI 1.32-27.77; p=0.030); considering the hours of attention to be inadequate (OR=78.13; 95% CI 4.84-125.97; p=0.002), and not receiving laboratory reports (OR=46.13; 95% CI 2.85-74.77; p=0.007).
Conclusion: Health services must focus on the early detection of conditions that may represent risk factors to proactively implement effective, rapid and high-impact interventions.
Downloads
References
World Health Organization - WHO. Global Tuberculosis Report, 2017. Fecha de consulta: 2 de mayo de 2018. Disponible en: http://apps.who.int/medicinedocs/es/d/Js23360en/
World Health Organization - WHO. Tuberculosis country profiles, 2016. Fecha de consulta: 19 de abril de 2018. Disponible en: http://www.who.int/tb/country/data/profiles/en/
Ministerio de Salud. Situación de la TBC en el Perú: normatividad, cobertura, casos y esquema de tratamiento. Lima: Ministerio de Salud; 2018. Fecha de consulta: 2 de mayo de 2018. Disponible en: ftp://ftp.minsa.gob.pe/sismed/ftp_carga/REUNION%20FORTALECIMIENTO%20SISMED%20EN%20EL%20MARCO%20DE%20LAS%20ESTRATEGIAS%20DEL%2012%20AL%2015%20MARZO%202018/REUNION%20TECNICA%2012%20_15%20MARZO%202018/REUNION%20DEL%2012_15_03_18/Dia%201/TBC.pdf
Bonilla C. Situación de la tuberculosis en el Perú. Acta Med Per. 2008;25:163-70.
Caminero J. Origen, presente y futuro de las resistencias en tuberculosis. Arch Bronconeumol. 2001;37:35-42. https://doi.org/10.1016/S0300-2896(01)75005-3
Rieder H. Bases epidemiológicas del control de la tuberculosis. Primera edición. Paris: Unión Internacional contra la Tuberculosis y Enfermedades Respiratorias; 1999. p. 172
Farga V, Torres Z, Herrera M. Perfil del paciente con tuberculosis que abandona el tratamiento en Chile. Rev Chil Enf Respir. 2015;31:52-7. https://doi.org/10.4067/S0717-73482015000100008
Brito D, Sales M, Silva M, Silva S, Gomez L, Souza V. Fatores de adesao e risco de abandono ao tratamento. R Interd. 2015;8:169-79.
Culquí D, Munayco C, Grijalvac C, Cayla JA, Horna O, Kenedy A, et al. Factores asociados al abandono de tratamiento antituberculoso convencional en Perú. Arch Bronconeumol. 2012;48:150-5. https://doi.org/10.1016/j.arbres.2011.12.008
Ministerio de Salud. Norma técnica de salud para la atención integral de las personas afectadas por tuberculosis. Lima: MINSA; 2013.
Da Fonseca P, Silva G, Mendes A. Fatores asociados ao abandono do tratamento da tuberulose pulmonar no Maranhao, Brasil, no periodo de 2001 a 2010. Cad Saúde Pública. 2014;30:1745-54. https://doi.org/10.1590/0102-311X00124513
Calsin N, Horner B. Fatores associados ao abandon do tratamiento tuberculose: Uma revisao integrative. Texto Contexto Enferm. 2011;20:599-606.
Mitnick C, Bayona J, Palacios E, Shin S, Furin J, Alcántara F, et al. Community-based therapy for multidrug-resistant tuberculosis in Lima, Perú. N Engl J Med. 2003;348:119-28. https://doi.org/ 10.1056/NEJMoa022928
Comolet TM, Rakotomalala R, Rajaonarioa H. Factors determining compliance with tuberculosis treatment in an urban environment, Tamatave, Madagascar. Int J Tuberc Lung Dis. 1998;2:891-7.
Gelmanova I, Keshavjee S, Golubchikova VT. Barriers to successful tuberculosis treatment in Tomsk, Russian Federation: Non-adherence, default and the acquisition of multidrug resistance. Bull World Health Organ. 2007;85:703-11. https://doi.org/ 10.2471/BLT.06.038331
Soza NI, Pereira SM, Barreto ML. Abandono del tratamiento de la tuberculosis en Nicaragua: resultados de un estudio comparativo. Rev Panam Salud Pública. 2005;17:271-8.
Arrosi S, Herrero MB, Greco A, Ramos S. Factores asociados a la no adherencia al tratamiento de la tuberculosis: revisión de la literatura. Buenos Aires: CEDES; 2011. p. 37
Sánchez E, Marquer C, Kalon S, Qayyum S, Hayrapetyan A, Varaine F, et al. Reasons for defaulting from drug-resistant tuberculosis treatment in Armenia: A quantitative and qualitative study. Int J Tuberc Lung Dis. 2014;18:160-7. https://doi.org/ 10.5588/ijtld.13.0369
Toczek A, Cox H, du Cros P, Cooke G, Ford N. Strategies for reducing treatment default in drug-resistant tuberculosis: Systematic review and meta-analysis. Int J Tuberc Lung Dis. 2013;17:299-307. https://doi.org/10.5588/ijtld.12.0537
Maciel E, Amancio J, Castro D, Braga J. Social determinants of pulmonary tuberculosis treatment non-adherence in Rio de Janeiro, Brazil. PLoS One. 2018;13:e0190578. https://doi.org/10.1371/journal.pone.0190578
Sobral F, Fernanda A. Educacão para a competitividade ou para a cidadania social? São Paulo Em Perspect. 2000;14:3-11. https://doi.org/10.1590/S0102-88392000000100002
Vijay S, Kumar P, Chauhan LS, Vollepore BH, Kizhakkethil UP, Rao SG. Risk factors associated with default among new smear positive TB patients treated under DOTS in India. PLoS One. 2010;5:e10043. https://doi.org/0.1371/journal.pone.0010043
Dick J, Lombard C. Shared vision--a health education project designed to enhance adherence to anti-tuberculosis treatment. Int J Tuberc Lung Dis. 1997;1:181-6.
Comolet TM, Rakotomalala R, Rajaonarioa H. Factors determining compliance with tuberculosis treatment in an urban environment, Tamatave, Madagascar. Int J Tuberc Lung Dis. 1998;2:891-7.
Sabates R, Feinstein L. The role of education in the uptake of preventative health care: The case of cervical screening in Britain. Soc Sci Med. 2006;62:2998-3010. https://doi.org/10.1016/j.socscimed.2005.11.032
Farga V. Tuberculosis lo que hay que saber. Rev Chil Enf Respir. 2008;24:317-22. https://doi.org/10.4067/S0717-73482008000400008
World Health Organization - WHO. Primera Conferencia Ministerial Mundial. Fecha de consulta: 20 de octubre de 2018. Disponible en: http://www.who.int/tb/tb-factsheetconference-es.pdf?ua=1
Laframboise HL. Health policy: Breaking the problem down into more manageable segments. Can Med Assoc J. 1973;108:388-91.
Lalonde M. A new perspective on the health of Canadians. Otawa: Minister of Supply and Services Canada; 1974.
Leimane V, Riekstina V, Holtz TH, Zarovska E, Skripconoka V, Thorpe L, et al. Clinical outcome of individualised treatment of multidrugresistant tuberculosis in Latvia: A retrospective cohort study. Lancet. 2005;365:318-26. https://doi.org/10.1016/S0140-6736(05)17786-1
Álvarez GC, Álvarez JF, Dorantes JE, Halperin D. Percepciones y prácticas relacionadas con la tuberculosis y la adherencia al tratamiento en Chiapas, México. Salud Pública Mex. 2000;42:520-8.
Deshmukh RD, Dhande DJ, Sachdeva KS, Sreenivas AN, Kumar AM, Parmar M. Social support a key factor for adherence to multidrug-resistant tuberculosis treatment. Indian J Tuberc. 2018;65:41-7. https://doi.org/10.1016/j.ijtb.2017.05.003
Barnhoorn F, Adriaanse H. In search of factors responsible for noncompliance among tuberculosis patients in Wardha District, India. Soc Sci Med. 1992;34:291-306.
Jakubowiak WM, Bogorodskaya EM, Borisov SE, Danilova ID, Kourbatova EV. Risk factors associated with default among new pulmonary TB patients and social support in six Russian regions. Int J Tuberc Lung Dis. 2007;11:46-53.
Sengupta S, Pungrassami P, Balthip Q, Strauss R, Kasetjaroen Y, Chongsuvivatwong V, et al. Social impact of tuberculosis in southern Thailand: Views from patients, care providers and the community. Int J Tuberc Lung Dis. 2006;10:1008-12.
Ananthakrishnan R, Jeyaraj A, Palanil G, Sathiyasekaran B. Socio-economic impact of TB on patients registered within RNTCP and their families in the year 2007 in Chennai, India. Lung India. 2012;29:221-6. https://doi.org/10.4103/0970-2113.99103
Kaulagekar-Nagarkar A, Dhake D, Jha P. Perspective of tuberculosis patients on family support and care in rural Maharashtra. Indian J Tuberc. 2012;59:224-30.
Wendling A, Barbosa AP, Módena CM, Torres V. O abandono do tratamento da tuberculose sob a perspectiva dos gerentes de diferentes centros de saúde de Belo Horizonte-MG, Brasil. Text Context Enferm. 2012;21:77-85 https://doi.org/10.1590/S0104-07072012000100009
Some similar items:
- María Consuelo Garzón, Dailyn Yorledy Angée, Claudia Llerena, Dora Leticia Orjuela, Jorge Ernesto Victoria, Surveillance of Mycobacterium tuberculosis resistance to antituberculosis drugs , Biomedica: Vol. 28 No. 3 (2008)
- Claudia Llerena, Raquel Medina, Description of Mycobacterium tuberculosis mutations conferring resistance to rifampicin and isoniazid detected by GenoType® MTBDRplus V.2 in Colombia , Biomedica: Vol. 37 No. 1 (2017)
- Lorena González, Ricardo Sánchez, Martha Isabel Murcia, The usefulness of the nitrate reductase assay for detecting drug-resistant Mycobacterium tuberculosis , Biomedica: Vol. 34 (2014): Abril, Suplemento 1, Resistencia bacteriana
- John-Leonardo Torres-Castiblanco, Jorge Alberto Carrillo, Daniel Hincapié-Urrego, Adriana Rojas-Villarraga, Tuberculosis in the era of anti-TNF-alpha therapy: Why does the risk still exist? , Biomedica: Vol. 38 No. 1 (2018)
- Leandro Galvis, Ángel Y. Sánchez, Leonardo F. Jurado, Martha I. Murcia, Tuberculosis associated with tumor necrosis factor-α antagonists, case description and analysis of reported cases in Colombia , Biomedica: Vol. 38 No. 1 (2018)
- Leidy González, Jorge Alberto Cortés, Systematic review of antimicrobial resistance in Enterobacteriaceae isolates from Colombian hospitals , Biomedica: Vol. 34 No. 2 (2014)
- Nelson José Alvis-Zakzuk, María de los Ángeles Carrasquilla, Verónica Jhajaira Gómez, Jaime Robledo, Nelson Rafael Alvis-Guzmán, José Mauricio Hernández, Diagnostic accuracy of three technologies for the diagnosis of multi-drug resistant tuberculosis , Biomedica: Vol. 37 No. 3 (2017)
- Fernanda Abilleira, Clarice Brum, Andrea von Groll, Pedro Eduardo da Silva, Evaluation of direct microplate nitrate reductase assay as a rapid method for the detection of multiple and extensively tuberculosis drug resistance , Biomedica: Vol. 35 No. 2 (2015)
- Manzour Hernando Hazbón, Recent advances in molecular methods for early diagnosis of tuberculosis and drug-resistant tuberculosis. , Biomedica: Vol. 24 (2004): Suplemento 1
- Claudia Llerena, Santiago Elías Fadul, María Consuelo Garzón, Graciela Mejía, Dora Leticia Orjuela, Luz Mary García, Hilda Beatriz Álvarez, Fernando Javier Ruiz, Drug-resistant Mycobacterium tuberculosis in children under 15 years , Biomedica: Vol. 30 No. 3 (2010)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























