Prevalence and impact of potentially inappropriate medication on community-dwelling older adults
Abstract
Introduction: Potentially inappropriate medication is associated with adverse health and functional outcomes, as well as increased health care costs.
Objective: To estimate the prevalence and types of potentially inappropriate medication according to the Beers criteria in community-dwelling older persons and to identify the major clinical and functional consequences of potentially inappropriate medication during two years of following.
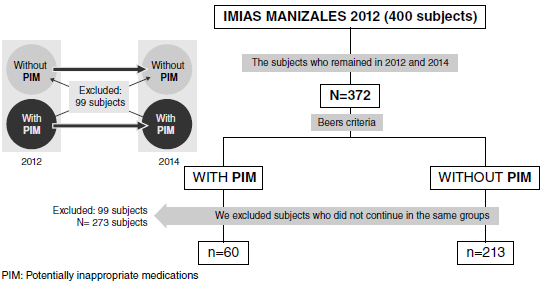
Materials and methods: We conducted a longitudinal, descriptive, and observational study that included 400 65-year or older community-dwelling people (48% women) selected by simple random sampling in 2012. In 2014, 372 people were re-evaluated and classified into two groups based on the presence or absence of potentially inappropriate medication through the follow-up period.
Results: In total, 31% had polypharmacy (5-9 medications) and 1,8% had excessive polypharmacy (10 or more medications). The mean of the number of medications was higher in the potentially inappropriate medication group (3 vs. 5.78; p<0.001) and 21.9% still had the potentially inappropriate medication status during the follow-up; of them, 75% had one potentially inappropriate medication and 23% two. The presence of potentially inappropriate medication was more frequent among frail and depressed male individuals with a bad health self-assessment and comorbidities, especially diabetes mellitus and chronic obstructive pulmonary disease. In the group with sustained potentially inappropriate medication, we found a worsening health self-assessment, increased frailty, a higher incidence of recurrent falls and prevalence of depression, as well as a higher hospital admission rate, ambulatory medical consultation, and more prescribed medications. We did not find an impact on functional capacity.
Conclusions: We validated the negative effects of potentially inappropriate medication in the long run for the health of older people and, therefore, potentially inappropriate medications should be monitored in primary care services to avoid greater risks.
Downloads
References
Ferrer A, Badía T, Formiga F, Almeda J, Fernández C, Pujol R. Diferencias de género en el perfil de salud de una cohorte de 85 años. Estudio Octabaix, Aten Primaria. 2011;43:577-84. https://doi.org/10.1016/j.aprim.2010.09.029
United Nations, Department of Economic and Social Affairs. Population Division. World Population Prospects. 2017;2-24.
Simonson W. Polypharmacy, MRPs, PIMs and deprescribing. Geriatr Nurs. 2015;36:467-8. https://doi.org/10.1016/j.gerinurse.2015.10.009
Shah BM, Hajjar ER. Polypharmacy, adverse drug reactions, and geriatric síndromes. Clin Geriatr Med. 2012;28:173-86. https://doi.org/10.1016/j.cger.2012.01.002
Mera F, Mestre D, Almeda J, Ferrer A, Formiga F, Rojas S. Paciente anciano y medicación crónica inapropiada en la comunidad ¿somos conscientes de ello? Rev Esp Geriatr Gerontol. 2011;46:125-30. https://doi.org/10.1016/j.regg.2010.12.008
Guthrie B, Makubate B, Hernández-Santiago V, Dreischulte T. The rising tide of polypharmacy and drug-drug interactions: Population database analysis 1995-2010. BMC Med. 2015;13:1-10. https://doi.org/10.1186/s12916-015-0322-7
Sönnichsen A, Trampisch US, Rieckert A, Piccoliori G, Vögele A, Flamm M. Polypharmacy in chronic diseases–Reduction of inappropriate medication and adverse drug events in older populations by electronic decision support (PRIMA-eDS): Study protocol for a randomized controlled trial. Trials. 2016;17:57. https://doi.org/10.1186/s13063-016-1177-8
Renom-Guiteras A, Meyer G, Thürmann PA. The EU-PIM list: A list of potentially inappropriate medications for older people consented by experts from seven European countries. Eur J Clin Pharmacol. 2015;71:861-75. https://doi.org/10.1007/s00228-015-1860-9
Levy HB. Polypharmacy reduction strategies: Tips on incorporating American Geriatrics Society Beers and Screening Tool of Older People’s Prescriptions Criteria. Clin Geriatr Med. 2017;33:177-87. https://doi.org/10.1016/j.cger.2017.01.007
Nicieza-García ML, Salgueiro-Vázquez MR, Jimeno-Demuth FJ, Manso G. Beers versus STOPP criteria in polypharmacy community-dwelling older patients. Farm Hosp. 2016;40:150-64. https://doi.org/10.7399/fh.2016.40.3.9706
Cano-Gutiérrez C, Samper-Ternent R, Cabrera J, Rosselli D. Uso de medicamentos en adultos mayores de Bogotá, Colombia. Rev Peru Med Exp Salud Pública. 2016;33:419. https://doi.org/10.17843/rpmesp.2016.333.2292
Robert L. Maher Jr, Hanlon JT, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13:1-11. https://doi.org/10.1517/14740338.2013.827660.Clinical
Gómez F, Zunzunegui MV, Alvarado B, Curcio CL, Pirkle CM, Guerra R. et al. Cohort profile: The international mobility in aging study (IMIAS). Int J Epidemiol. 2018;47:1393. https://doi.org/10.1093/ije/dyy074
WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC classification and DDD assignment 2020. Oslo: WHO; 2019. p. 48-225.
Fick DM, Mion LC, Beers MH, Waller JL. Health outcomes associated with potentially inappropriate medication use in older adults. Res Nurs Heal. 2008;31:42-51. https://doi.org/10.1002/nur.20232
Pastor J, Aranda A, Gascón JJ, Rausell VJ, Tobaruela M. Adaptación española de los criterios Beers. An Sist Sanit Navar. 2015;38:375-85. https://doi.org/10.4321/s1137-66272015000300002
González-Colaço M, Aldea-Perona AM, Boada-Fernández C, Areosa-Sastre A, Rodríguez-Jiménez C, García Sánchez-Colomer M, et al. Spanish list of potentially inappropriate drugs in the elderly (ES-PIA project), Eur J Clin Pharmacol. 2019;75:1161-76. https://doi.org/10.1007/s00228-019-02684-3
Gandek B, WareJE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, et al. Cross-validation of item selection and scoring for the SF-12 health survey in nine countries: Results from the IQOLA Project. J Clin Epidemiol. 1998;51:1171-8. https://doi.org/10.1016 / s0895-4356 (98) 00109-7
Miller GE, Sarpong EM, Davidoff AJ, Yang EY, Brandt NJ, Fick DM. Determinants of potentially inappropriate medication use among community-dwelling older adults. Health Serv Res. 2017;52:1534-9. https://doi.org/10.1111/1475-6773.12562
WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC classification and DDD assignment. 14th Edition. Oslo: WHO; 2011. p. 48-247.
Fried LP, Seeman T, Newman AB, Walston J, Tangen CM, Tracy R. Frailty in older adults: Evidence for a phenotype. J Gerontol Ser A Biol Sci Med Sci. 2001;56:M146–57. https://doi.org/10.1093/gerona/56.3.m146
Gomes CS, Pirkle CML, Zunzunegui MV, Taurino D, Fernandes De Souza J, Hwang P, et al. Frailty and life course violence: The international mobility in aging study. Arch Gerontol Geriatr. 2018;76:26-33. https://doi.org/10.1016/j.archger.2018.02.002
Bazargan M, Smith JL, King EO. Potentially inappropriate medication use among hypertensive older African-American adults. BMC Geriatr. 2018;18:1-9. https://doi.org/10.1186/s12877-018-0926-9
Berdot S, Bertrand M, Dartigues JF, Fourrier A, Tavernier B, Ritchie K, et al. Inappropriate medication use and risk of falls - A prospective study in a large community-dwelling elderly cohort, BMC Geriatr. 2009;9:1-10. https://doi.org/10.1186/1471-2318-9-30
Lechevallier-Michel N, Gautier-Bertrand M, Alpérovitch A, Berr C, Belmin J, Legrain S. Frequency and risk factors of potentially inappropriate medication use in a communitydwelling elderly population: Results from the 3C Study. Eur J Clin Pharmacol. 2005;60: 813-9. https://doi.org/10.1007/s00228-004-0851-z
Roadolff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385. https://doi.org/10.1063/1.4932809
Campo-Arias A, Díaz-Martínez LA, Rueda-Jaimes GA, Cadena-Afanador L de P, Hernández NL. Psychometric properties of the CES-D scale among Colombian adults from the general population. Rev Colomb Psiquiatr. 2007;36:664-74.
Caldas VV, Zunzunegui MV, Freire A, Guerra RO. Translation, cultural adaptation and psychometric evaluation of the Leganés cognitive test in a low educated elderly Brazilian population. Arq Neuropsiquiatr. 2012;70:22-7. https://doi.org/10.1590/s0004-282x2012000100006
Rosso AL, Eaton CB, Wallace R, Stefanick ML, Ockene JK, David J, et al. Results from the women´s health initiative observational study. J Am Geriatr Soc. 2014;61:371-9. https://doi.org/10.1111/jgs.12147
Gómez JF, CurcioC-L, Alvarado B, Zunzunegui MV, Guralnik J. Validity and reliability of the Short Physical Performance Battery (SPPB): A pilot study on mobility in the Colombian Andes. Colomb Médica. 2013;44:165-71. https://doi.org/10.25100/cm.v44i3.1181
Bin Chang C, Chen JH, Wen CJ, Kuo HK, Lu IS, Chiu LS. Potentially inappropriate medications in geriatric outpatients with polypharmacy: Application of six sets of published explicit criteria. Br J Clin Pharmacol. 2011;72:482-9. https://doi.org/10.1111/j.1365-2125.2011.04010.x
Martins GA, Acurcio FA, Franceschini SC, Priore SE, Ribeiro AQ. Uso de medicamentos potencialmente inadequados entre idosos do Município de Viçosa, Minas Gerais, Brasil: um inquérito de base populacional. Cad Saúde Pública. 2015;31:2401-12. https://doi.org/10.1590/0102-311X00128214
Hanlon JT, Artz MB, Pieper CF, Lindblad CI, Sloane RJ, Ruby CM, et al. Inappropriate medication use among frail elderly inpatients. Ann Pharmacother. 2004;38:9-14. https://doi.org/10.1345/aph.1D313
Herr M, Sirven N, Grondin H, Pichetti S, Sermet C. Frailty, polypharmacy, and potentially nappropriate medications in old people: Findings in a representative sample of the French population. Eur J Clin Pharmacol. 2017;37:1165-72. https://doi.org/10.1007/s00228-017-2276-5
Lai HY, Hwang SJ, Chen YC, Chen TJ, Lin MH, Chen LK. Prevalence of the prescribing of potentially inappropriate medications at ambulatory care visits by elderly patients covered by the Taiwanese National Health Insurance program. Clin Ther. 2009;31:1859-70. https://doi.org/10.1016/j.clinthera.2009.08.023
Sarwar MR, Dar A. Assessment of prescribing potentially inappropriate medications listed in Beers criteria and its association with the unplanned hospitalization: A cross-sectional study in Lahore, Pakistan. Clin Interv Aging. 2018;13:1485-95. https://doi:10.2147/cia.s173942
Johnell K. The controversies surrounding polypharmacy in old age–where are we? Expert Rev Clin Pharmacol. 2018;11:825-7. https://doi.org/10.1080/17512433.2018.1510313
Magaziner J, Cadigan DA, Fedder DO, Hebel JR. Medication use and functional decline among community-dwelling older women. J Aging Health. 1989;1:470–84. https://doi.org/10.1177/089826438900100404
Ocampo J. Autoevaluación de la salud: importancia de su uso en adultos mayores. Colomb Med. 2010;41:275-89. https://doi.org/10.25100/cm.v41i3.715
Gnjidic D, Hilmer SN. Potential contribution of medications to frailty. J Am Geriatr Soc. 2012;60:401. https://doi:10.1111/j.1532-5415.2011.03810.x
Kojima T, Akishita M, Nakamura T, Nomura K, Ogawa S, Iijima K. Association of polypharmacy with fall risk among geriatric outpatients. Geriatr Gerontol Int. 2011;11:438-44. https://doi.org/10.1111/j.1447-0594.2011.00703.x
Some similar items:
- Edison Pineda, Alejandra Fernández, Carmen Lucía Curcio, Juliana Fernandes de Souza, Afshin Vafaei, José Fernando Gómez, Potentially inappropriate medication on community-dwelling older adults: Longitudinal analysis of IMIAS study , Biomedica: Vol. 44 No. 2 (2024): Publicación anticipada, junio
- Paola Andrea Filigrana, Olga Lucía Gómez, Fabián Méndez, Impact of a waste disposal site on adult respiratory health , Biomedica: Vol. 31 No. 3 (2011)
- Alejandro Estrada, Doris Cardona, Ángela María Segura, Lina Marcela Chavarriaga, Jaime Ordóñez, Jorge Julián Osorio, Quality of life in institutionalized elderly people of Medellín , Biomedica: Vol. 31 No. 4 (2011)
- Ricardo Pineda-Tamayo, Giovanna Arcila, Patricia Restrepo, Juan Manuel Anaya, Impact of cardiovascular illness on hospitalization costs in patients with rheumatoid arthritis. , Biomedica: Vol. 24 No. 4 (2004)
- Margarita Arboleda, Mónica Campuzano, Berta Nelly Restrepo, Gladys Cartagena, The clinical behavior of dengue in patients hospitalized in the Antonio Roldán Betancur Hospital of Apartadó, Antioquia, 2000. , Biomedica: Vol. 26 No. 2 (2006)
- Carlos Alberto Cano, Miguel Germán Borda, Antonio J. Arciniegas, Juan Sebatián Parra, Hearing disorders in elderly people, associated factors and quality of life: SABE Study, Bogotá, Colombia , Biomedica: Vol. 34 No. 4 (2014)
- Ángela Quintero, María Eucaris Henao, María Mercedes Villamil, Jairo León, Changes in depression and loneliness after laughter therapy in institutionalized elders , Biomedica: Vol. 35 No. 1 (2015)
- Julián Alfredo Fernández-Niño, Eduardo Bustos-Vázquez, Multimorbidity: conceptual basis, epidemiological models and measurement challenges , Biomedica: Vol. 36 No. 2 (2016)
- Pedro Á. Latorre-Román, Juan Manuel Arévalo-Arévalo, Felipe García-Pinillos, Association between leg strength and muscle cross-sectional area of the quadriceps femoris with the physical activity level in octogenarians , Biomedica: Vol. 36 No. 2 (2016)
- Fernando Rosso, Sara Vanegas, Sarita Rodríguez, Robinson Pacheco, Prevalence and clinical course of dengue infection in elderly patients with acute febrile illness in a tertiary care hospital in Cali, Colombia , Biomedica: Vol. 36 (2016): Suplemento 2, Enfermedades virales
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























