Worldwide evidence about infant stunting from a public health perspective: A systematic review
Abstract
Introduction: According to the World Health Organization (WHO) global estimates for 2017, 9.6% of children under 5 years old are stunted. Worldwide evidence shows that actions for preventing stunting and catching-up growth are relevant if addressed by all the sectors involved. Therefore, there is a need to identify ‘intersectoral actions’ to address the risk of stunting during pregnancy and the first 2 years of life.
Objective: To identify and describe worldwide evidence for prevention, nutritional interventions, and ‘intersectoral collaboration’ efforts against stunting in infants.
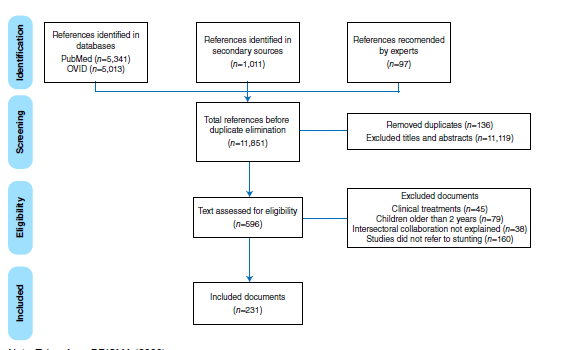
Materials and methods: We conducted a systematic review in 2019 (PROSPERO CRD42019134431). The search included PubMed, OVID, and Web of Science, as well as WHO and the Food and Agriculture Organization of the United Nations (FAO) official documents and expert recommendations.
Results: We selected 231 studies: 86.1% described prevention-related factors, 30.7%, nutritional interventions, and 52.8% intersectoral collaboration efforts; 36.4% of the studies were conducted in multiple regions; 61% of the studies described the importance of interventions during pregnancy, 71.9% from birth up to 6 months old, and 84.8% from 6 months up to 2 years old. The most frequent variables described were antenatal care, nutritional counseling for the mother and the newborn, and counseling on micronutrient supplementation.
Conclusions: Evidence-based understanding of actions geared towards monitoring the risk of stunting-associated factors from pregnancy up to 2 years old is critical.
Downloads
References
World Health Organization. Use of new World Health Organization child growth standards to assess how infant malnutrition relates to breastfeeding and mortality. Access: May 20, 2020. Available from: https://www.who.int/bulletin/volumes/88/1/08-057901/en/
Ministerio de Salud y Protección Social. Resolución 2465 de 2016. Bogotá, D.C.: Minsalud; 2016. p. 1-47.
World Health Organization. Malnutrición. Geneva: WHO; 2010. p. 1.
World Health Organization. Enfermedades diarreicas. Geneva: WHO; 2017. p. 1.
Walters DE. Reaching the global target to increase exclusive breastfeeding: How much will it cost and how can we pay for it? Breastfeed Med. 2016;11:413-5. https://doi.org/10.1089/bfm.2016.0128
Comisión Económica para América Latina y el Caribe-CEPAL, Programa Mundial de Alimentos. El costo de la doble carga de la malnutrición. Santiago de Chile: PNU, CEPAL; 2017. p. 101.
Grantham-McGregor S, Cheung YB, Cueto S, Glewwe P, Richter L, Strupp B, et al. Developmental potential in the first 5 years for children in developing countries. Lancet. 2007;369:60-70. https://doi.org/10.1016/S0140-6736(07)60032-4
Black R, Walker S, Bhutta Z, Christian P, De Onis M. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427-51. https://doi.org/10.1016/S0140-6736(13)60937-X
UNICEF. UNICEF’s approach to scaling up nutrition for mothers and their children. Geneva: UNICEF; 2015. p. 16.
Bhutta Z, Rizvi A, Gaffey M, Walker N, Horton S. Evidence-based interventions for improvement of maternal and child nutrition: What can be done and at what cost? Lancet. 2013;382:452-77. https://doi.org/10.1016/S0140-6736(13)60996-4
Casanovas M, Lutter C, Mangasaryan N, Mwadime R, Hajeebhoy N, Aguilar A, et al. Multisectoral interventions for healthy growth. Matern Child Nutr. 2013;9(Suppl.2):46-57. https://doi.org/10.1111/mcn.12082
Onis M, Branca F. Childhood stunting: A global perspective. Matern Child Nutr. 2016;12(Suppl.1):12-26. https://doi.org/10.1111/mcn.12231
World Health Organization. Global nutrition targets 2025: Anaemia policy brief. Geneva: WHO; 2014. p. 2.
Chase C, Ngure F. Multisectoral approaches to improving nutrition: Water, sanitation, and hygiene. Washington, D.C.: World Bank Group; 2016. p. 6.
Higgins-Steele A, Mustaphi P, Varkey S, Ludin H, Safi N, Bhutta ZA. Stop stunting: Situation and way forward to improve maternal, child and adolescent nutrition in Afghanistan. Matern Child Nutr. 2016;12(Suppl.1):237-41. https://doi.org/10.1111/mcn.12288
Mackintosh U, Marsh D, Schroeder D. Sustained positive deviant child care practices and their effects on child growth in Viet Nam. Food Nutr Bull. 2002;23(Suppl.):18-27.
Sunguya B, Ong K, Dhakal S, Mlunde L, Shibanuma A, Yasuoka J, et al. Strong nutrition governance is a key to addressing nutrition transition in low and middle-income countries: Review of countries’ nutrition policies. Nutr J. 2014;13:65. https://doi.org/10.1186/1475-2891-13-65
World Bank. When water becomes a hazard: A diagnostic report on the state of water supply, sanitation and poverty in Pakistan and its impact on child stunting. Washington, D.C.: World Bank; 2018. p. 81.
Universidad de los Andes, Institute for Fiscal Studies (Reino Unido), Fundación Éxito; ICBF. Evaluación del impacto de la implementación de un currículo de estimulación con capacitación y acompañamiento de madres comunitarias y mejoramiento nutricional en hogares comunitarios FAMI. Bogotá, D.C.: Universidad de los Andes, Institute for Fiscal Studies, Fundación Éxito; ICBF. 2017. p. 46.
Roberfroid D, Huybregts L, Lanou H, Ouedraogo L, Henry M, Meda N. Impact of prenatal multiple micronutrients on survival and growth during infancy: A randomized controlled trial. Am J Clin Nutr. 2012;95:916-24. https://doi.org/10.3945/ajcn.111.029033
Muldiasman M, Kusharisupeni K, Laksminingsih E, Besral B. Can early initiation to breastfeeding prevent stunting in 6-59 months old children? J Health Res. 2018;32:334-41. https://doi.org/10.1108/JHR-08-2018-038
Kadiyala S, Morgan EH, Cyriac S, Margolies A, Roopnaraine T. Adapting agriculture platforms for nutrition: A case study of a participatory, video-based agricultural extension platform in India. PLoS ONE. 2016;11:e0164002. https://doi.org/10.1371/journal.pone.0164002
Kuhnt J, Vollmer S. Antenatal care services and its implications for vital and health outcomes of children: Evidence from 193 surveys in 69 low-income and middle-income countries. BMJ Open. 2017;7:e017122. https://doi.org/10.1136/bmjopen-2017-017122
Nisar Y, Dibley M, Aguayo V. Iron-folic acid supplementation during pregnancy reduces the risk of stunting in children less than 2 years of age: A retrospective cohort study from Nepal. Nutrients. 2016;8:67. https://doi.org/10.3390/nu8020067
Dzed L, Wangmo K. Reducing stunting in Bhutan: An achievable national goal. Matern Child Nutr. 2016;12(Suppl.1):246-8. https://doi.org/10.1111/mcn.12287
Baye K, Faber M. Windows of opportunity for setting the critical path for healthy growth. Public Health Nutr. 2015;18:1715-7. https://doi.org/10.1017/S136898001500186X
U.S. Agency for International Development. Multi-sectoral nutrition strategy monitoring & learning plan. Washington, D.C.: USAID; 2018.
Kandpal E, Alderman H, Friedman J, Filmer D, Onishi J, Avalos J. A conditional cash transfer program in the Philippines reduces severe stunting. J Nutr. 2016;146:1793-800. https://doi.org/10.3945/jn.116.233684
Shekar KJ, Dayton J, Kweku J, Pereira A, D’Alimonte M. An investment framework for meeting the global nutrition target for stunting. Washington, D.C.: The World Bank; 2017.
World Health Organization. Reducing stunting in children. Equity considerations for achieving the Global Nutrition Targets 2025. Geneva: World Health Organization; 2018. p. 10.
Kalimbira AA, MacDonald C, Simpson JR. The impact of an integrated community-based micronutrient and health programme on stunting in Malawian preschool children. Public Health Nutr. 2010;13:720-9. https://doi.org/10.1017/S1368980009991753
Smuts M, Malan L, Kruger H, Rothman M, Kvalsvig J, Covic N, et al. Effect of small-quantity lipid-based nutrient supplements on growth, psychomotor development, iron status, and morbidity among 6- to 12-mo-old infants in South Africa: A randomized controlled trial. Am J Clin Nutr. 2019;109:55-68. https://doi.org/10.1093/ajcn/nqy282
Wang J, Chang S, Zhao L, Yu W, Zhang J, Man Q, et al. Effectiveness of community-based complementary food supplement (Yingyangbao) distribution in children aged 6-23 months in poor areas in China. PLoS ONE. 2017;12:e0174302. https://doi.org/10.1371/journal.pone.0174302
Mchome Z, Bailey A, Darak S, Haisma H. A child may be tall but stunted. Meanings attached to childhood height in Tanzania. Matern Child Nutr. 2019;15:e12769. https://doi.org/10.1111/mcn.12769
World Health Organization. Composition of a multi-micronutrient supplement to be used in pilot programmes among pregnant women in developing countries: Report of a United Nations Children’s Fund (UNICEF), World Health Organization (WHO) and United Nations University workshop. Geneva: World Health Organization; 1999. p. 10.
Aguayo VM, Nair R, Badgaiyan N, Krishna V. Determinants of stunting and poor linear growth in children under 2 years of age in India: An in-depth analysis of Maharashtra’s comprehensive nutrition survey. Matern Child Nutr. 2016;12(Suppl.1):121-40. https://doi.org/10.1111/mcn.12259
Khan A, Kabir I, Ekstrom E, Asling-Monemi K, Alam D. Effects of prenatal food and micronutrient supplementation on child growth from birth to 54 months of age: A randomized trial in Bangladesh. Nutr J. 2011;10:134. https://doi.org/10.1186/1475-2891-10-134
van der Kam S, Roll S, Swarthout T, Edyegu-Otelu G, Matsumoto A, Kasujja FX, et al. Effect of short-term supplementation with ready-to-use therapeutic food or micronutrients for children after illness for prevention of malnutrition: A randomised controlled trial in Uganda. PLoS Med. 2016;13:e1001951. https://doi.org/10.1371/journal.pmed.1001951
Menon P, Nguyen PH, Saha KK, Khaled A, Sanghvi T, Baker J, et al. Combining intensive counseling by frontline workers with a nationwide mass media campaign has large differential impacts on complementary feeding practices but not on child growth: Results of a cluster-randomized program evaluation in Bangladesh. J Nutr. 2016;146:2075-84. https://doi.org/10.3945/jn.116.232314
Kodish S, Aburto N, Hambayi MN, Kennedy C, Gittelsohn J. Identifying the sociocultural barriers and facilitating factors to nutrition-related behavior change: Formative research for a stunting prevention program in Ntchisi, Malawi. Food Nutr Bull. 2015;36:138-53. https://doi.org/10.1177/0379572115586784
Akombi B, Agho K, Hall J, Wali N, Renzaho A, Merom D. Stunting, wasting and underweight in Sub-Saharan Africa: A systematic review. Int J Environ Res Public Health. 2017;14:863. https://doi.org/10.3390/ijerph14080863
Hoddinott J, Gillespie S, Yosef S. Public-private partnerships and undernutrition: Examples and future prospects. World Rev Nutr Diet. 2016;115:233-8. https://doi.org/10.1159/000442110
Marini A, Rokx C. Standing Tall Peru’s success in overcoming its stunting crisis. Washington, D.C.: World Bank Group; 2017. p. 11.
Republic of Mozambique. Multisectoral plan for chronic malnutrition reduction in Mozambique 2011 – 2014. Maputo: Prime Minister; 2010.
Prentice AM. Stunting in developing countries. World Rev Nutr Diet. 2019;119:171-83. https://doi.org/10.1159/000494315
Powell C, Baker-Henningham H, Walker S, Gernay J, Grantham-McGregor S. Feasibility of integrating early stimulation into primary care for undernourished Jamaican children: Cluster randomised controlled trial. BMJ. 2004;329:89. https://doi.org/10.1136/bmj.38132.503472.7C
Moench-Pfanner R, van Ameringen M. The Global Alliance for Improved Nutrition (GAIN): A decade of partnerships to increase access to and affordability of nutritious foods for the poor. Food Nutr Bull. 2012;33(Suppl.):S373-80. https://doi.org/10.1177/15648265120334S313
Some similar items:
- Gloria Alcaraz, Carlos Bernal, William Cornejo, Natalia Figueroa, Margarita Múnera, Nutritional status and living conditions in children in an urban area of Turbo, Antioquia, Colombia , Biomedica: Vol. 28 No. 1 (2008)
- Blair Ortiz, Diego A. Herrera, Sergio Vargas, Clinical application of diffusion tensor imaging and tractography in a child with holoprosencephaly , Biomedica: Vol. 31 No. 2 (2011)
- Sandra Lorena Girón, Julio César Mateus, Carlos Enrique Castellar, Cost-effectiveness analysis of two strategies for malaria control in the urban area of , Biomedica: Vol. 26 No. 3 (2006)
- Stella Carrasco Rodríguez, Myriam Sanchez Gómez, Serum IGF-I and IGFBP-3 levels in pregnant adolescents in an economically depressed community , Biomedica: Vol. 21 No. 4 (2001)
- Adriana Umaña, Stella Carrasco, Myriam Sánchez, Role of the cytokine-3 signaling suppressor protein (SOCS 3) in growth hormone resistance induced by malnutrition. , Biomedica: Vol. 23 No. 3 (2003)
- Wilson Mejía-Naranjo, Myriam Sánchez-Gomez, Protein malnutrition up-regulates growth hormone receptor expression in rat splenic B lymphocytes. , Biomedica: Vol. 24 No. 4 (2004)
- María Victoria Benjumea, José Hernán Parra, Juan Felipe Jaramillo, How to intervene and prevent stunting of children from homes belonging to the Sisbén in Caldas , Biomedica: Vol. 37 No. 4 (2017)
- Magda Ginnette Rodríguez, Elba Giomar Sichacá, Mortality due to malnutrition in older adults, Colombia, 2014-2016 , Biomedica: Vol. 39 No. 4 (2019)
- Andres Felipe Villaquiran, Diana María Rivera , Enmanuel Fernando Portilla, Sandra Jimena Jácome, Vastus lateralis and medialis muscular activation during frontal and sagittal single-leg jumps in sportswomen , Biomedica: Vol. 40 No. 1 (2020)
- Lorena Alexandra Maldonado-Maldonado, Sandra Patricia Misnaza-Castrillón, Carlos Andrés Castañeda-Orjuela, Inequalities in dental prenatal control in Colombia: An analysis based on the IV National Oral Health Study, 2013-2014 , Biomedica: Vol. 41 No. 2 (2021)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























