Synchronization between videofluoroscopic swallowing study and surface electromyography in patients with neurological involvement presenting symptoms of dysphagia
Abstract
Introduction: Dysphagia is defined as the difficulty in transporting food and liquids from the mouth to the stomach. The gold standard to diagnose this condition is the videofluoroscopic swallowing study. However, it exposes patients to ionizing radiation. Surface electromyography is a non-radioactive alternative for dysphagia evaluation that records muscle electrical activity during swallowing.
Objective: To evaluate the relationship between the relative activation times of the muscles involved in the oral and pharyngeal phases of swallowing and the kinematic events detected in the videofluoroscopy.
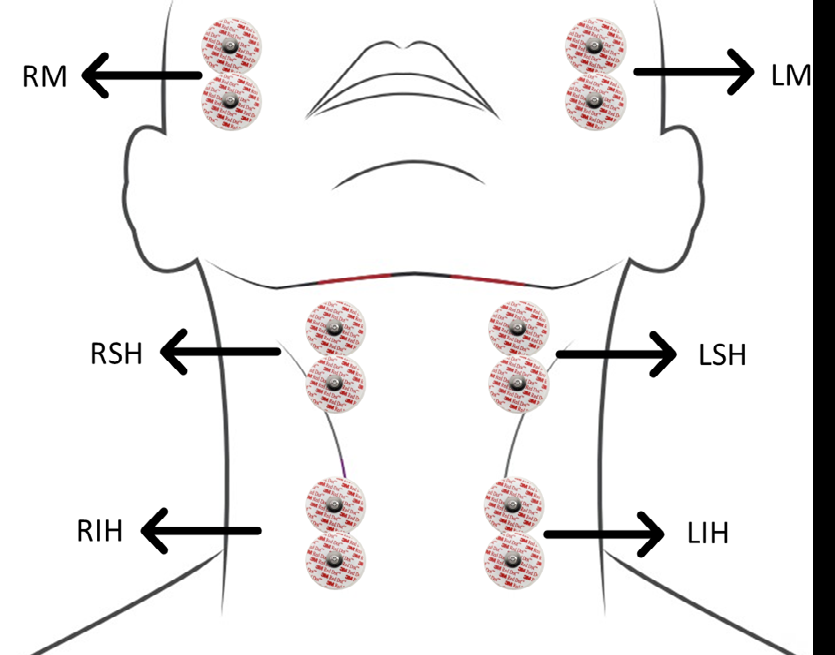
Materials and methods: Electromiographic signals from ten patients with neurological involvement who presented symptoms of dysphagia were analyzed simultaneously with
videofluoroscopy. Patients were given 5 ml of yogurt, 10 ml of water, and 3 g of crackers. Masseter, suprahyoid, and infrahyoid muscle groups were studied bilaterally. The bolus transit through the mandibular line, vallecula, and the cricopharyngeus muscle was analyzed in relation to the onset and offset times of each muscle group activation.
Results: The average time of the pharyngeal phase was 0.89 ± 0.12 s. Muscle activation was mostly observed prior to the bolus transit through the mandibular line and vallecula. The end of the muscle activity suggested that the passage of the bolus through the cricopharyngeus muscle was almost complete.
Conclusión: The muscle activity times, duration of the pharyngeal phase, and sequence of the muscle groups involved in swallowing were determined using sEMG validated with the videofluoroscopic swallowing study.
Downloads
References
Baijens LWJ, Clavé P, Cras P, Ekberg O, Forster A, Kolb GF, et al. European society for swallowing disorders - European union geriatric medicine society white paper: Oropharyngeal dysphagia as a geriatric syndrome. Clin Interv Aging. 2016;11:1403-28. https://doi.org/10.2147/CIA.S107750
Cámpora HL, Falduti AL. Evaluación y tratamiento de las alteraciones de la deglución. Rev Am Med Respir Rev Am Med Resp. 2012;12:98-107.
Matsuo K, Palmer JB. Anatomy and physiology of feeding and swallowing: Normal and abnormal. Phys Med Rehabil Clin N Am. 2008;19:691-707. https://doi.org/10.1016/j.pmr.2008.06.001
Wirth R, Dziewas R, Beck AM, Clavé P, Hamdy S, Heppner HJ, et al. Oropharyngeal dysphagia in older persons – from pathophysiology to adequate intervention: A review and summary of an international expert meeting. Clin Interv Aging. 2016;11:189-208. https://doi.org/10.2147/CIA.S97481
Hey C, Pluschinski P, Pajunk R, Almahameed A, Girth L, Sader R, et al. Penetration–aspiration: Is their detection in FEES® reliable without video recording? Dysphagia. 2015;30:418-22. https://doi.org/10.1007/s00455-015-9616-3
Roy N, Stemple J, Merrill RM, Thomas L. Dysphagia in the elderly: Preliminary evidence of prevalence, risk factors, and socioemotional effects. Ann Otol Rhinol Laryngol. 2007;116:858-65. https://doi.org/10.1177/000348940711601112
Kawashima K, Motohashi Y, Fujishima I. Prevalence of dysphagia among communitydwelling elderly individuals as estimated using a questionnaire for dysphagia screening. Dysphagia. 2004;19:266-71. https://doi.org/10.1007/s00455-004-0013-6
Suárez-Escudero JC, Rueda-Vallejo ZV, Orozco-Duque AF. Disfagia y neurología: ¿una unión indefectible? Acta Neurológica Colomb. 2018;34:92-100.
Dudik JM, Coyle JL, Sejdic E. Dysphagia screening: Contributions of cervical auscultation signals and modern signal-processing techniques. IEEE Trans Human-Machine Syst. 2015;45:465-77. https://doi.org/10.1109/THMS.2015.2408615
Rommel N, Hamdy S. Oropharyngeal dysphagia: Manifestations and diagnosis. Nat Rev Gastroenterol Hepatol. 2016;13:49-59. https://doi.org/10.1038/nrgastro.2015.199
Azola A, Greene L, Taylor-kamora I, Macrae P, Anderson C, Humbert IA. The relationship between submental surface electromyography and Hyo-Laryngeal kinematic measures of Mendelsohn maneuver duration. J Speech Lang Hear Res. 2015;24:1-14. Rev Gastroenterol Hepatol. 2016;13:49-59. https://doi.org/10.1044/2015_JSLHR-S-14-0203
Chen DF. Dysphagia in the hospitalized patient. Hosp Med Clin. 2017;6:38-52. https://doi.org/10.1016/j.ehmc.2016.07.004
Fattori B, Giusti P, Mancini V, Grosso M, Barillari MR, Bastiani L, et al. Comparison between videofluoroscopy, fiberoptic endoscopy and scintigraphy for diagnosis of oro-pharyngeal dysphagia. Acta Otorhinolaryngol Ital. 2016;36:395-402. https://doi.org/10.14639/0392-100X-829
Ertekin C, Aydogdu I. Neurophysiology of swallowing. Clin Neurophysiol. 2003;114:2226-44. https://doi.org/10.1016/s1388-2457(03)00237-2
Archer SK, Smith CH, Newham DJ. Surface electromyographic biofeedback and the effortful swallow exercise for stroke-related dysphagia and in healthy ageing. Dysphagia. 2021;36:281-92. https://doi.org/10.1007/s00455-020-10129-8
Nazmi N, Rahman MAA, Yamamoto SI, Ahmad SA, Zamzuri H, Mazlan SA. A review of classification techniques of EMG signals during isotonic and isometric contractions. Sensors (Basel). 2016;16:1-28. https://doi.org/10.3390/s16081304
Restrepo-Agudelo S. Methodology of sequential classification of non-invasive multichannel biosignals, oriented to automatic diagnosis of dysphagia (tesis). Medellín: Instituto Tecnológico Metropolitano; 2019.
Poorjavad M, Talebian S, Nakhostin Ansari N, Soleymani Z. Surface electromyographic assessment of swallowing function. Iran J Med Sci. 2017;42:194-200.
Sakai K, Nakayama E, Rogus-Pulia N, Takehisa T, Takehisa Y, Urayama KY, et al. Submental muscle activity and its role in diagnosing sarcopenic dysphagia. Clin Interv Aging. 2020;15:1991-9. https://doi.org/10.2147/CIA.S278793
Wang CM, Chen JY, Chuang CC, Tseng WC, Wong AM, Pei YC. Aging-related changes in swallowing, and in the coordination of swallowing and respiration determined by novel noninvasive measurement techniques. Geriatr Gerontol Int. 2015;15:736-44. https://doi.org/10.1111/ggi.12343
Suzuki M, Sasaki M, Kamata K, Nakayama A, Shibamoto I, Tamada Y. Swallowing pattern classification method using multichannel surface EMG signals of suprahyoid and infrahyoid muscles. Adv Biomed Eng. 2020;9:10-20. https://doi.org/10.14326/abe.9.10
Shieh WY, Wang CM, Chang CS. Development of a portable non-invasive swallowing and respiration assessment device. Sensors (Basel). 2015;15:12428-53. https://doi.org/10.3390/s150612428
Shieh W-Y, Wang C-M, Cheng H-YK, Wang C-H. Using wearable and non-invasive sensors to verification, and clinical application. Sensors (Basel). 2019;19:2624. https://doi.org/10.3390/s19112624
Sejdic E, Malandraki GA, Coyle JL. Computational deglutition: Using signal- and imageprocessing methods to understand swallowing and associated disorders. IEEE Signal Process Mag. 2019;36:138-46. https://doi.org/10.1109/MSP.2018.2875863
Giraldo-Cadavid LF, Gutiérrez-Achury AM, Ruales-Suárez K, Rengifo-Varona ML, Barros C, Posada A, et al. Validation of the Spanish version of the Eating Assessment Tool-10 (EAT-10spa) in Colombia. A blinded prospective cohort study. Dysphagia. 2016;31:398-406. https://doi.org/10.1007/s00455-016-9690-1
Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, et al. Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol. 2008;117:919-24. https://doi.org/10.1177/000348940811701210
Newman R, Vilardell N, Clavé P, Speyer R. Effect of bolus viscosity on the safety and efficacy of swallowing and the kinematics of the swallow response in patients with oropharyngeal dysphagia: White Paper by the European Society for Swallowing Disorders (ESSD). Dysphagia. 2016:31;232-49. https://doi.org/10.1007/s00455-016-9696-8
Barrett KE, Barman SM, Boitano S, Brooks HL, editors. Gastrointestinal motility. En: Ganong’s Review of Medical Physiology. Twenty-fifth ed. New York, NY: McGraw Hill; 2018. https://accesspharmacy.mhmedical.com/content.aspx?bookid=1587§ionid=97165321
Restrepo-Agudelo S, Roldán-Vasco S, Ramírez-Arbeláez L, Cadavid-Arboleda S, Pérez-Giraldo E, Orozco-Duque AF. Improving surface EMG burst detection in infrahyoid muscles during swallowing using digital filters and discrete wavelet analysis. J Electromyogr Kinesiol. 2017;35:1-8. https://doi.org/10.1016/j.jelekin.2017.05.001
Prosiegel M, Schelling A, Wagner-Sonntag E. Dysphagia and multiple sclerosis. Int MS J. 2004;11:22-31.
Daroff R, Jankovic J, Mazziotta J, Pomeroy S. Bradley’s neurology in clinical practice. 7th edition. Elsevier Inc.; 2015.
Pfeiffer RF. Gastrointestinal dysfunction in Parkinson’s disease. Lancet Neurol. 2003;2:107-16. https://doi.org/10.1016/s1474-4422(03)00307-7
Clavé P, Kraa M, Arreola V, Girvent M, Farré R, Palomera E, et al. The effect of bolus viscosity on swallowing function in neurogenic dysphagia. Aliment Pharmacol Ther. 2006;24:1385-94. https://doi.org/10.1111/j.1365-2036.2006.03118.x
Guzmán MJ, Dulbecco M. Abordaje del paciente con disfagia. ACTA Gastroenterológica Latinoam. 2020;50:42-50.
Lee JT, Park E, Hwang JM, Jung T Du, Park D. Machine learning analysis to automatically measure response time of pharyngeal swallowing reflex in videofluoroscopic swallowing study. Sci Rep. 2020;10:1-9. https://doi.org/10.1038/s41598-020-71713-4
Park D, Lee HH, Lee ST, Oh Y, Lee JC, Nam KW, et al. Normal contractile algorithm of swallowing related muscles revealed by needle EMG and its comparison to videofluoroscopic swallowing study and high resolution manometry studies: A preliminary study. J Electromyogr Kinesiol. 2017;36:81-9. https://doi.org/10.1016/j.jelekin.2017.07.007
Koyama Y, Ohmori N, Momose H, Kondo E, Yamada S, Kurita H. Detection of swallowing disorders using a multiple channel surface electromyography sheet: A preliminary study. J Dent Sci. 2021;16:160-7. https://doi.org/10.1016/j.jds.2020.06.009
Ko JY, Kim H, Jang J, Lee JC, Ryu JS. Electromyographic activation patterns during swallowing in older adults. Sci Rep. 2021;11:1-10. https://doi.org/10.1038/s41598-021-84972-6
Poorjavad M, Talebian S, Ansari NN, Soleymani Z. Surface electromyographic assessment of swallowing function. Iran J Med Sci. 2017;42:194-200.
Ertekin C. Electrophysiological evaluation of oropharyngeal dysphagia in ALS. Handb Clin Neurophysiol. 2004;4:487-512.
Some similar items:
- Carlos Santiago Uribe, Paula Andrea Millán, María Isabel Montes, Dagoberto Cabrera, Alejandra Arboleda, Biopercular syndrome: report of two cases and literature review , Biomedica: Vol. 28 No. 2 (2008)
- Juan Carlos Villa-Camacho, Juan Camilo Vargas-Zambrano, John Mario González, Flow cytometry model for the detection of neutralizing antibodies against of IFN-β , Biomedica: Vol. 32 No. 4 (2012)
- Luis Alfonso Zarco, Sonia Patricia Millán, Darío Londoño, Ludy Parada, Alejandra Taborda, Miguel Germán Borda, The cost-effectiveness of interferon beta treatment in patients with a clinically isolated syndrome in Colombia , Biomedica: Vol. 34 No. 1 (2014)
- Jaime E. Castellanos, José I. Neissa, Sigrid J. Camacho, Dengue virus induces apoptosis in SH-SY5Y human neuroblastoma cells , Biomedica: Vol. 36 (2016): Suplemento 2, Enfermedades virales
- Julio César Martinez, Sandra Patricia Misnaza, Rare diseases mortality in Colombia, 2008-2013 , Biomedica: Vol. 38 No. 2 (2018)
- María del Pilar Olaya, Nadezdha Esperanza Vergel, José Luis López, María Dolores Viña, Mario Francisco Guerrero, Coumarin analogue 3-methyl-7H-furo[3,2-g] chromen-7-one as a possible antiparkinsonian agent , Biomedica: Vol. 39 No. 3 (2019)
- Andres Felipe Villaquiran, Diana María Rivera , Enmanuel Fernando Portilla, Sandra Jimena Jácome, Vastus lateralis and medialis muscular activation during frontal and sagittal single-leg jumps in sportswomen , Biomedica: Vol. 40 No. 1 (2020)
- Elkin Beltrán , Diana Díaz , Cindy Díaz , Luis Zarco , Quality of life in patients with multiple sclerosis and their caregivers in Colombia: One-year follow-up , Biomedica: Vol. 40 No. 1 (2020)
- Saúl Reyes-Niño , Jaime Eduardo Rodríguez-Orozco, Habib Georges Moutran-Barroso, Hellen Kreinter-Rosembaun , Mariana Gaviria-Carrillo , Vanessa Salej-Durán , Julián Mancera-Charry , Ana Claudia Villegas , David Cuellar-Giraldo , Juan Sebastián Torres-Sandoval , Ángela Gómez-Mazuera, Aristides Duque-Samper, Jaime Toro-Gómez , Controversies in neuroimmunology: multiple sclerosis, vaccination, SARS-CoV-2 and other dilemas , Biomedica: Vol. 42 No. Sp. 2 (2022): Covid-19
- Laura Estefanía Arenas-Vargas , Lorena López-Reyes, Simón Cárdenas-Robledo, Multiple sclerosis functional tests and their comparability with self-administered values: A pilot study , Biomedica: Vol. 43 No. 3 (2023)
Copyright (c) 2022 Biomedica

This work is licensed under a Creative Commons Attribution 4.0 International License.
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























