B-cell lymphocytosis in relatives of Colombian patients with chronic B-cell lymphoproliferative disorders
Abstract
Introduction. Monoclonal B-cell lymphocytosis generally precedes chronic lymphocytic leukemia, affecting about 12% of the healthy adult population. This frequency increases in relatives of patients with chronic B-cell lymphoproliferative disorders.
Objective. To determine the frequency of monoclonal B-cell lymphocytosis in relatives of patients with chronic B-cell lymphoproliferative disorders, their immunophenotypic/cytogenetic characteristics, a possible relationship with infectious agents, and short-term follow-up in the Colombian population.
Materials and methods. Fifty healthy adults with a family history of chronic B-cell lymphoproliferative disorders were studied using multiparametric flow cytometry,
cytogenetic/serological testing, lifestyle survey, and 2-year follow-up.
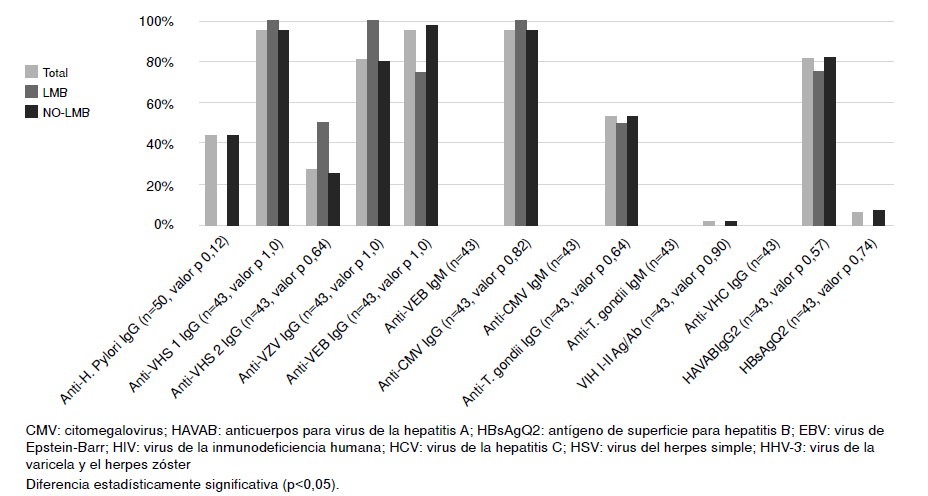
Results. The frequency of monoclonal B-cell lymphocytosis found was 8%, with a predominance of female gender and advanced age, increasing to 12.5% for individuals with
a family history of chronic lymphocytic leukemia. Three out of four individuals presented chronic lymphocytic leukemia-type immunophenotype, all with low counts. In turn, a significantly higher number of cells/μl is observed in these individuals in T lymphocyte subpopulations, together with a greater predisposition to the disease. The described clonal populations increase over time in a non-significant manner.
Conclusions. The frequency and behavior of monoclonal B-cell lymphocytosis in patients with family history of chronic B-cell lymphoproliferative disorders are like those found in related studies, which suggests that there is no involvement of more relevant genes that can trigger uncontrolled clonal proliferation, but that generates immunological deregulation that could justify a greater risk of serious infection in these individuals.
Downloads
References
Li YY, Hu DZ, Tian C. Research progress on diagnosis and treatment of B cell chronic lymphoproliferative disease--review. Zhongguo Shi Yan Xue Ye Xue Za Zhi. 2018;26:1220-4. https://doi.org/10.7534/j.issn.1009-2137.2018.04.046
Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375-90. https://doi.org/10.1182/blood-2016-01-643569
Strati P, Shanafelt TD. Monoclonal B-cell lymphocytosis and early-stage chronic lymphocytic leukemia: Diagnosis, natural history, and risk stratification. Blood. 2015;126:454-62. https://doi.org/10.1182/blood-2015-02-585059
Slager SL, Lanasa MC, Marti GE, Achenbach SJ, Camp NJ, Abbasi F, et al. Natural history of monoclonal B-cell lymphocytosis among relatives in CLL families. Blood. 2021;137:2046-56. https://doi.org/10.1182/blood.2020006322
Shanafelt TD, Kay NE, Parikh SA, Achenbach SJ, Lesnick CE, Hanson CA, et al. Risk of serious infection among individuals with and without low count monoclonal B-cell lymphocytosis (MBL). Leukemia. 2021;35:239-44. https://doi.org/10.1038/s41375-020-0799-8
Villegas-Gracia R, Franco-Alzate C, Rendón-Henao J, Torres-Hernández JD, Jaramillo-Arbeláez PE. Frequency of monoclonal B-cell lymphocytosis in relatives of patients with chronic lymphocytic leukemia. Colomb Med. 2016;47:81-6.
Goldin LR, Lanasa MC, Slager SL, Cerhan JR, Vachon CM, Strom SS, et al. Common occurrence of monoclonal B-cell lymphocytosis among members of high-risk CLL families. Br J Haemato. 2010;151:152-8. https://doi.org/10.1111/j.1365-2141.2010.08339.x
Nieto WG, Almeida J, Romero A, Teodosio C, López A, Henriques AF, et al. Increased frequency (12%) of circulating chronic lymphocytic leukemia–like B-cell clones in healthy subjects using a highly sensitive multicolor flow cytometry approach. Blood. 2009;114:33-7. https://doi.org/10.1182/blood-2009-01-197368
van Dongen JJM, Lhermitte L, Böttcher S, Almeida J, van der Velden VHJ, Flores-Montero J, et al. EuroFlow antibody panels for standardized n-dimensional flow cytometric immunophenotyping of normal, reactive and malignant leukocytes. Leukemia. 2012;26:1908-75. https://doi.org/10.1038/leu.2012.120
Kalina T, Flores-Montero J, van Der Velden VHJ, Martin-Ayuso M, Böttcher S, Ritgen M, et al. EuroFlow standardization of flow cytometer instrument settings and immunophenotyping protocols. Leukemia. 2012;26:1986-2010. https://doi.org/10.1038/leu.2012.122
De Faria-Moss M, Yamamoto M, Arrais-Rodrigues C, Criado I, Gomes CP, de Lourdes Chauffaille M, et al. High frequency of chronic lymphocytic leukemia-like low-count monoclonal B-cell lymphocytosis in Japanese descendants living in Brazil. Haematologica. 2020;105:e298. https://doi.org/10.3324/haematol.2019.230813
Criado I, Nieto WG, Oliva-Ariza G, Fuentes-Herrero B, Teodosio C, Lecrevisse Q, et al. Ageand sex-matched normal leukocyte subset ranges in the general population defined with the euroflow lymphocyte screening tube (LST) for monoclonal b-cell lymphocytosis (MBL) vs. non-MBL subjects. Cancers. 2022;15:58. https://doi.org/10.3390/cancers15010058
Doody GM, Dempsey PW, Fearon DT. Activation of B lymphocytes: Integrating signals from CD19, CD22 and Fc gamma RIIb1. Curr Opin Immunol. 1996;8:378-82. https://doi.org/10.1016/S0952-7915(96)80128-2
Han X, Jorgensen JL, Brahmandam A, Schlette E, Huh YO, Shi Y, et al. Immunophenotypic study of basophils by multiparameter flow cytometry. Arch Pathol Lab Med. 2008;132:813-9. https://doi.org/10.5858/2008-132-813-ISOBBM
Kleinstern G, Weinberg JB, Parikh SA, Braggio E, Achenbach SJ, Robinson DP, et al. Polygenic risk score and risk of monoclonal B-cell lymphocytosis in caucasians and risk of chronic lymphocytic leukemia (CLL) in African Americans. Leukemia. 2022;36:119-25. https://doi.org/10.1038/s41375-021-01344-9
Kaastrup K, Grønbæk K. The impact of sedentary lifestyle, high-fat diet, tobacco smoke, and alcohol intake on the hematopoietic stem cell niches. HemaSphere. 2021;5:e615. https://doi.org/10.1097/HS9.0000000000000615
Criado I, Rodríguez-Caballero A, Gutiérrez ML, Pedreira CE, Alcoceba M, Nieto W, et al. Low-count monoclonal B-cell lymphocytosis persists after seven years of follow up and is associated with a poorer outcome. Haematologica. 2018;103:1198. https://doi.org/10.3324/haematol.2017.183954
Popp HD, Flach J, Brendel S, Ruppenthal S, Kleiner H, Seifarth W, et al. Accumulation of DNA damage and alteration of the DNA damage response in monoclonal B-cell lymphocytosis and chronic lymphocytic leukemia. Leuk Lymphoma. 2019;60:795-804. https://doi.org/10.1080/10428194.2018.1498494
El Chaer F, Keng M, Ballen KK. MLL-rearranged acute lymphoblastic leukemia. Curr Hematol Malig Rep. 2020;15:83-9. https://doi.org/10.1007/s11899-020-00582-5
Kostopoulos IV, Paterakis G, Pavlidis D, Kastritis E, Terpos E, Tsitsilonis OE, et al. Clonal evolution is a prognostic factor for the clinical progression of monoclonal B-cell lymphocytosis. Blood Cancer J. 2017;7:e597. https://doi.org/10.1038/bcj.2017.77
Küppers R. Mechanisms of B-cell lymphoma pathogenesis. Nat Rev Cancer. 2005;5:251-62. https://doi.org/10.1038/nrc1589
Some similar items:
- Vanihamín Domínguez, Itzen Aguiñiga, Leticia Moreno, Beatriz Torres, Edelmiro Santiago-Osorio, Sodium caseinate increases the number of B lymphocytes in mouse , Biomedica: Vol. 37 No. 4 (2017)
- Juan Carlos Villa-Camacho, Juan Camilo Vargas-Zambrano, John Mario González, Flow cytometry model for the detection of neutralizing antibodies against of IFN-β , Biomedica: Vol. 32 No. 4 (2012)
- Yeny Zulay Castellanos, Zulma Milena Cucunubá, Astrid Carolina Flórez, Luis Carlos Orozco-Vargas, Reproducibility of serological tests for the diagnosis of Trypanosoma cruzi infection in pregnant women in an endemic area of Santander, Colombia , Biomedica: Vol. 34 No. 2 (2014)
- Viviana Marcela Rodríguez, Adriana Cuéllar, Lyda Marcela Cuspoca, Carmen Lucía Contreras, Marcela Mercado, Alberto Gómez, Phenotypical determinants of stem cell subpopulations derived from human umbilical cord blood. , Biomedica: Vol. 26 No. 1 (2006)
- Cristian Vallejo, Yolanda Cifuentes, Characterization and six-month follow-up on a cohort of newborns with congenital syphilis , Biomedica: Vol. 36 No. 1 (2016)
- Lina Marcela Barrera, León Darío Ortiz, Hugo Grisales, Mauricio Rojas, Mauricio Camargo, Flow cytometry in peripheral blood reticulocytes as a marker of chromosome instability in highgrade glioma patients , Biomedica: Vol. 38 No. 3 (2018)
- Liliana Fernández, Mauricio Velásquez, Luz Fernanda Sua, Indira Cujiño, Martha Giraldo, Diego Medina, Mauricio Burbano, Germán Torres, Carlos Munoz-Zuluaga, Leidys Gutiérrez-Martínez, The porcine biomodel in translational medical research: From biomodel to human lung transplantation , Biomedica: Vol. 39 No. 2 (2019)
- Ana María Arrunátegui, Daniel S. Ramón, Luz Marina Viola, Linda G. Olsen, Andrés Jaramillo, Technical and clinical aspects of the histocompatibility crossmatch assay in solid organ transplantation , Biomedica: Vol. 42 No. 2 (2022)
Copyright (c) 2023 Biomedica

This work is licensed under a Creative Commons Attribution 4.0 International License.
Funding data
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























