Loneliness as a predictor of mortality in cancer patients, a cohort study
Abstract
Introduction. Some studies have indicated that loneliness may be associated with an increased risk of mortality in cancer patients, as it can weaken treatment response and the immune system, and promote harmful behaviors, worsening the prognosis and increasing the likelihood of death. Addressing loneliness in public health is essential to provide social support and improve outcomes in cancer patients.
Objective. To obtain an estimator of the unwanted loneliness-mortality association.
Materials and methods. We followed a prospective cohort of 400 patients for two years (exposure=loneliness levels; outcome=mortality; sociodemographic and clinical control variables were included). A parametric survival model (log normal) was used.
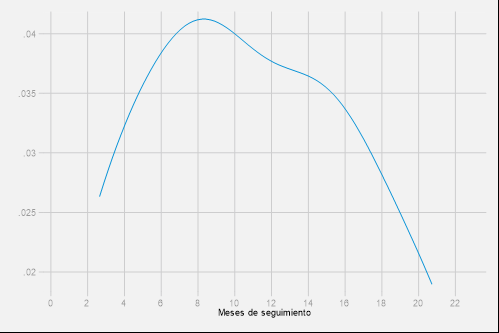
Results. The cohort had a median survival of 20.2 months and a mortality rate of 3.2 deaths/100 patient-months (95% CI: 2.8 to 3.7). The survival model found the following time ratios (TR): moderate level/low level: TR=0.55; 95% CI: 0.39 to 0.77; moderately high level/low level: TR=0.62; 95% CI: 0.41 to 0.93; high level/low level: TR=1.17; 95% CI: 0.31 to 4.42.
Conclusion. Compared to patients with low levels of loneliness, patients with moderate or moderately high levels reach death more quickly (statistically significant TRs, adjusted for the effect of other variables in the model); this highlights the need for interventions to mitigate loneliness and promote social support in patients having cancer.
Downloads
References
International Agency for Research on Cancer. Cancer incidence in five continents, volume XI (electronic version). Lyon, France: International Agency for Research on Cancer; 2022.
Ministerio de Salud y Protección Social. Incidencia del cáncer se redujo en los últimos 3 años. Fecha de consulta: 3 de junio del 2023. Disponible en: https://www.minsalud.gov.co/Paginas/Incidencia-del-cancer-se-redujo-en-los-ultimos-3-anos.aspx
International Agency for Research on Cancer. GLOBOCAN 2020: Estimated cancer incidence, mortality and prevalence worldwide in 2020. International Agency for Research on Cancer, 2021 Fecha de consulta: 3 de junio del 2023. Disponible en: https://gco.iarc.fr/today/data/factsheets/populations/900-world-fact-sheets.pdf
Organización Panamericana de la Salud. Enfermedades no transmisibles. Fecha de consulta: 3 de junio del 2023. Disponible en: https://www.paho.org/es/temas/enfermedadesno-transmisibles
Organización Mundial de la Salud. Cáncer: datos y cifras 2022. Fecha de consulta: 3 de junio del 2023. Disponible en: https://www.who.int/es/news-room/fact-sheets/detail/cancer
De Massachusetts G, Israel B, Nutrición SZ, do Sul CdRG. La planificación del control del cáncer en América Latina y el Caribe. The Lancet Oncology Comisión. 2013;14:391-436. Fecha de consulta: 11 de junio del 2023. Disponible en: https://www.thelancet.com/pb/assets/raw/Lancet//pdfs/tlo-commission/tlo-commission-series-spanish.pdf
Antoni MH, Lutgendorf SK, Cole SW, Dhabhar FS, Sephton SE, McDonald PG, et al. The influence of bio-behavioural factors on tumour biology: Pathways and mechanisms. Nat Rev Cancer. 2006;6:240-8. https://doi.org/10.1038/nrc1820
Lutgendorf SK, Sood AK. Biobehavioral factors and cancer progression: Physiological pathways and mechanisms. Psychosom Med. 2011;73:724-30. https://doi.org/10.1097/PSY.0b013e318235be76
Nausheen B, Carr NJ, Peveler RC, Moss-Morris R, Verrill C, Robbins E, et al. Relationship between loneliness and proangiogenic cytokines in newly diagnosed tumors of colon and rectum. Psychosom Med. 2010;72:912-6. https://doi.org/10.1097/PSY.0b013e3181f0bc1c
Butow PN, Hiller JE, Price MA, Thackway SV, Kricker A, Tennant CC. Epidemiological evidence for a relationship between life events, coping style, and personality factors in the development of breast cancer. J Psychosom Res. 2000;49:169-81. https://doi.org/10.1016/s0022-3999(00)00156-2
Chida Y, Hamer M. Chronic psychosocial factors and acute physiological responses to laboratory-induced stress in healthy populations: A quantitative review of 30 years of investigations. Psychol Bull. 2008;134:829-85. https://doi.org/10.1037/a0013342
van Tuijl LA, Voogd AC, de Graeff A, Hoogendoorn AW, Ranchor AV, Pan KY, et al. Psychosocial factors and cancer incidence (PSY-CA): Protocol for individual participant data meta-analyses. Brain Behav. 2021;11:e2340. https://doi.org/10.1002/brb3.2340
Antoni MH, Lutgendorf S. Psychosocial factors and disease progression in cancer. Current Directions in Psychological Science. 2007;16:42-6. https://doi.org/10.1111/j.1467-8721.2007.00472.x
Cheung WY, Barmala N, Zarinehbaf S, Rodin G, Le LW, Zimmermann C. The association of physical and psychological symptom burden with time to death among palliative cancer outpatients. J Pain Symptom Manage. 2009;37:297-304. https://doi.org/10.1016/j.jpainsymman.2008.03
Peplau LA, Perlman D. Loneliness: A sourcebook of current theory, research and therapy. New York: John Wiley & Sons Incorporated; 1982.
Victor CR, Scambler SJ, Bowling A, Bond J. The prevalence of, and risk factors for loneliness in later life: A survey of older people in Great Britain. Ageing & Society. 2005;25:357-75. https://doi.org/10.1017/S0144686X04003332
Tzouvara V, Papadopoulos C, Randhawa G. A narrative review of the theoretical foundations of loneliness. Br J Community Nurs. 2015;20:329-34. https://doi.org/10.12968/bjcn.2015.20.7.329
Peplau LA. Perspective on loneliness. Lonelinss: a sourcebook of current theory, research and therapy. New York: Wiley Interscience; 1982.
Gardiner C, Geldenhuys G, Gott M. Interventions to reduce social isolation and loneliness among older people: an integrative review. Health Soc Care Community. 2018;26:147-157. https://doi.org/10.1111/hsc.12367
Ernst M, Niederer D, Werner AM, Czaja SJ, Mikton C, Ong AD, et al. Loneliness before and during the COVID-19 pandemic: A systematic review with meta-analysis. Am Psychol. 2022;77:660-77. https://doi.org/10.1037/amp0001005
Russell DW. UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. J Pers Assess. 1996;66:20-40. https://doi.org/10.1207/s15327752jpa6601_2
Ditommaso E, Brannen C, Best L. Measurement and validity characteristics of the short version of the social and emotional loneliness scale for adults. Educ Psychol Meas. 2004;64:99-119.
De Jong Gierveld J, van Tilburg T. The De Jong Gierveld short scales for emotional and social loneliness: Tested on data from 7 countries in the UN generations and gender surveys. Eur J Ageing. 2010;7:121-30. https://doi.org/10.1007/s10433-010-0144-6
Deckx L, van den Akker M, Buntinx F. Risk factors for loneliness in patients with cancer: A systematic literature review and meta-analysis. Eur J Oncol Nurs. 2014;18:466-77. https://doi.org/10.1016/j.ejon.2014.05.002
Cacioppo JT, Hawkley LC. Loneliness. Handbook of individual differences in social behavior. New York, NY: The Guilford Press; 2009. p. 227-40.
Hawkley LC, Cacioppo JT. Loneliness and pathways to disease. Brain Behav Immun. 2003;17(Suppl.1):S98-105. https://doi.org/10.1016/s0889-1591(02)00073-9
Luo Y, Hawkley LC, Waite LJ, Cacioppo JT. Loneliness, health, and mortality in old age: A national longitudinal study. Soc Sci Med. 2012;74:907-14. https://doi.org/10.1016/j.socscimed.2011.11.028
Yildirim Y, Kocabiyik S. The relationship between social support and loneliness in Turkish patients with cancer. J Clin Nurs. 2010;19:832-9. https://doi.org/10.1111/j.1365-2702.2009.03066.x
D’ippolito S, Ambrosini E, Shams M, Calì G, Pastorelli D. The effect of loneliness on cancer mortality. J Clin Oncol. 2017;35(15Suppl.):vi82-8. https://doi.org/10.1093/annonc/mdx434
Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10:227-37. https://doi.org/10.1177/1745691614568352
Dahlberg L, Andersson L, McKee KJ, Lennartsson C. Predictors of loneliness among older women and men in Sweden: A national longitudinal study. Aging Ment Health. 2015;19:409-17. https://doi.org/10.1080/13607863.2014.944091
Rico-Uribe LA, Caballero FF, Martín-María N, Cabello M, Ayuso-Mateos JL, Miret M. Association of loneliness with all-cause mortality: A meta-analysis. PLoS One. 2018;13:e0190033. https://doi.org/10.1371/journal.pone.0190033
You L-F, Yeh J-R, Su M-C. Expression profiles of loneliness-associated genes for survival prediction in cancer patients. Asian Pac J Cancer Prev. 2014;15:185-90. https://doi.org/10.7314/apjcp.2014.15.1.185
Henriksen J, Larsen ER, Mattisson C, Andersson NW. Loneliness, health and mortality. Epidemiol Psychiatr Sci. 2019;28:234-9. https://doi.org/10.1017/S2045796017000580
Kraav SL, Awoyemi O, Junttila N, Vornanen R, Kauhanen J, Toikko T, et al. The effects of loneliness and social isolation on all-cause, injury, cancer, and CVD mortality in a cohort of middle-aged Finnish men. A prospective study. Aging Ment Health. 2021;25:2219-28. https://doi.org/10.1080/13607863.2020.1830945
Cacioppo JT, Cacioppo S. The growing problem of loneliness. Lancet. 2018;391:426. https://doi.org/10.1016/S0140-6736(18)30142-9
Rentscher KE, Zhou X, Small BJ, Cohen HJ, Dilawari AA, Patel SK, et al. Loneliness and mental health during the COVID-19 pandemic in older breast cancer survivors and noncancer controls. Cancer. 2021;127:3671-3679. https://doi.org/10.1002/cncr.33687
Gallagher S, Bennett KM, Roper L. Loneliness and depression in patients with cancer during COVID-19. J Psychosoc Oncol. 2021;39:445-51. https://doi.org/10.1080/07347332.2020.1853653
Clifton K, Gao F, Jabbari J, van Aman M, Dulle P, Hanson J, et al. Loneliness, social isolation, and social support in older adults with active cancer during the COVID-19 pandemic. J Geriatr Oncol. 2022;13:1122-31. https://doi.org/10.1016/j.jgo.2022.08.003
Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017:152:157-71. https://doi.org/10.1016/j.puhe.2017.07.035
Instituto Nacional de Cancerología. Anuario estadistico 2022. Bogotá: Instituto Nacional de Cancerología; 2023.
Hertz N. El siglo de la soledad: recuperar los vínculos humanos en un mundo dividido. Buenos Aires: Ediciones Paidós; 2021.
Valdelamar Jiménez A, Parra-Alfonso AM, Sánchez-Pedraza R, De La Hoz-Restrepo F. Adaptación transcultural de la versión colombiana de la Escala de Soledad de UCLA en pacientes con diagnóstico de cáncer. Revista Colombiana de Cancerología. 2022;26:97-110. https://doi.org/10.35509/01239015.764
Zarei S, Memari AH, Moshayedi P, Shayestehfar M. Validity and reliability of the UCLA loneliness scale version 3 in Farsi. Educational Gerontology. 2016;42:49-57.
McWhirter BT. Factor analysis of the revised UCLA loneliness scale. Current Psychology. 1990;9:56-68.
Valdelamar Jiménez A, Parra-Alfonso AM, De La Hoz-Restrepo F, Sánchez-Pedraza R. Validation of the UCLA loneliness scale in colombian patients diagnosed with cancer. Rev Heliyon. 2023.
Oliveros H, Buitrago G. Validation and adaptation of the Charlson Comorbidity Index using administrative data from the Colombian health system: retrospective cohort study. BMJ Open. 2022;12:e054058. https://doi.org/10.1136/bmjopen-2021-054058
Yates JW, Chalmer B, McKegney FP. Evaluation of patients with advanced cancer using the Karnofsky performance status. Cancer. 1980;45:2220-4. https://doi.org/10.1002/1097-0142(19800415)45:8<2220::aid-cncr2820450835>3.0.co;2-q
Elovainio M, Lumme S, Arffman M, Manderbacka K, Pukkala E, Hakulinen C. Living alone as a risk factor for cancer incidence, case-fatality and all-cause mortality: A nationwide registry study. SSM Popul Health. 2021:15:100826. https://doi.org/10.1016/j.ssmph.2021.100826
Instituto Nacional de Cancerología. Cáncer en cifras 2022. Bogotá: Instituto Nacional de Cancerología; 2022.
Hsieh FY, Lavori PW. Sample-size calculations for the Cox proportional hazards regression model with nonbinary covariates. Control Clin Trials. 2000;21:552-60. https://doi.org/10.1016/s0197-2456(00)00104-5
Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol. 2007;165:710-8. https://doi.org/10.1093/aje/kwk052
Schenfield D. Partial residuals for the proportional hazards regression model. Biometrika. 1982;69:239-41.
Cacioppo S, Grippo AJ, London S, Goossens L, Cacioppo JT. Loneliness: Clinical import and interventions. Perspect Psychol Sci. 2015;10:238-49. https://doi.org/10.1177/1745691615570616
Iovino P, Vellone E, Cedrone N, Riegel B. A Middle-Range Theory of social isolation in chronic illness. Int J Environ Res Public Health. 2023;20:4940. https://doi.org/10.3390/ijerph20064940
Holt-Lunstad J, Robles TF, Sbarra DA. Advancing social connection as a public health priority in the United States. Am Psychol. 2017;72:517-30. https://doi.org/10.1037/amp0000103
Departamento Administrativo Nacional de Estadistica. “Soledad” en Colombia, una aproximación desde las estadisticas oficiales. Series Notas Estadísticas. Fecha de consulta: 11 de junio del 2023. Disponible en: https://www.dane.gov.co/files/investigaciones/notasestadisticas/ago-2020-soledad-en-colombia.pdf
Parra Gómez CE, García S, Insuasty Enriquez J. Experiencias de vida en mujeres con cáncer de mama en quimioterapia. Revista Colombiana de Psiquiatría. 2011;40:65-84.
Lafaurie MM. Mujeres con cáncer de seno: experiencias y significados. Revista Colombiana de Enfermería. 2012;7:12-21.
David LPB, Duque MÁC. Pacientes con cáncer en fase terminal-una mirada fenomenológica existencial. International Journal of Psychological Research. 2008;1:13-20.
Amaya Cocunubo IF, Duque Cajamarca P, Gómez Verano LE, Saavedra Guzmán LR. Nivel de soledad social en personas mayores de Bogotá. Tabula Rasa. 2022;44:303-23.
Cardona JL, Villamil MM, Henao E, Quintero A. Concepto de soledad y percepción que de su momento actual tiene el adulto mayor en el municipio de Bello, Colombia, 2007. Revista Facultad Nacional de Salud Pública. 2009;27:153-63.
Barcelo A, Duffett-Leger L, Pastor-Valero M, Pereira J, Colugnati FAB, Trapido E. The role of education on Cancer amenable mortality among non-Hispanic blacks & non-Hispanic whites in the United States (1989-2018). BMC Cancer. 2021;21:907. https://doi.org/10.1186/s12885-021-08633-7
Some similar items:
- Liliana Villa, Iván Mauricio Trompa, Fernando Nicolás Montes, Joaquín Guillermo Gómez, Carlos Andrés Restrepo, Analysis of mortality caused by tuberculosis in Medellín, Colombia, 2012 , Biomedica: Vol. 34 No. 3 (2014)
- Sandra Lorena Girón, Julio César Mateus, Fabián Méndez, Impact of an open waste disposal site on the occurrence of respiratory symptoms and on health care costs of children , Biomedica: Vol. 29 No. 3 (2009)
- María Carolina Sanabria, Gerardo Muñoz, Clara Inés Vargas, Mutations in the BRCA1 gene (185delAG and 5382insC) are not present in any of the 30 breast cancer patients analyzed from eastern Colombia , Biomedica: Vol. 29 No. 1 (2009)
- Erika Santamaría, Olga Lucía Cabrera, Yaneth Zipa, Cristina Ferro, Martha Liliana Ahumada, Raúl Hernando Pardo, Preliminary evaluation of the Culicoides biting nuisance (Diptera: Ceratopogonidae) in the province of Boyacá, Colombia , Biomedica: Vol. 28 No. 4 (2008)
- Andrés Leonardo González, Ruth Aralí Martínez, Luis Ángel Villar, Clinical evolution of dengue in hospitalized patients , Biomedica: Vol. 28 No. 4 (2008)
- Helena Luisa Brochero, Martha L. Quiñones, Challenges of the medical entomology for the surveillance in public health in Colombia: reflections on the state of malaria , Biomedica: Vol. 28 No. 1 (2008)
- Carlos Humberto Torres, Marcela E. Varona, Angélica Lancheros, Rosa Isabel Patiño, Helena Groot, DNA damage assessment and biological monitoring of occupational exposure to organic solvents, 2006 , Biomedica: Vol. 28 No. 1 (2008)
- Juan José Alava, Pedro J. Jiménez, Gnathostoma (Spirurida: Gnathostomatidae) infection in the tigerfish Hoplias microlepis: prevalence, correlation with fish size, hosts, and public health implications , Biomedica: Vol. 29 No. 4 (2009)
- Oscar Fernando Herrán, María F. Ardila, Categories of alcohol consumers and the criteria for classification , Biomedica: Vol. 29 No. 4 (2009)
- Karen Melissa Ordóñez, Odismar Andrea Hernández, Jorge Alberto Cortés, María José López, Gladys Alfonso, Alejandro Junca, Left-sided infective endocarditis caused by Pseudomonas aeruginosa treated medically , Biomedica: Vol. 30 No. 2 (2010)
Copyright (c) 2024 Biomedica

This work is licensed under a Creative Commons Attribution 4.0 International License.
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























