Vigilancia centinela de neumonías y meningitis bacterianas en menores de 5 años en un hospital pediátrico de tercer nivel en Colombia - 2016
Resumen
Introducción. La neumonía y la meningitis bacterianas son enfermedades inmunoprevenibles; la vigilancia centinela aporta información relevante acerca de su comportamiento.
Objetivo. Presentar los resultados de la vigilancia centinela de neumonía y meningitis llevada a cabo en la HOMI, Fundación Hospital Pediátrico La Misericordia.
Materiales y métodos. Se hizo un estudio descriptivo entre el 1 de enero y el 31 diciembre del 2016, de la vigilancia diaria de pacientes menores de 5 años con diagnóstico de neumonía o meningitis bacteriana, según las definiciones de la Organización Panamericana de la Salud (OPS). Los microorganismos fueron identificados usando el sistema automatizado VITEK TM2. Los aislamientos se enviaron al grupo de microbiología del Instituto Nacional de Salud para confirmación, serotipificación, y caracterización genotípica y fenotípica. Asimismo, se establecieron los perfiles de sensibilidad antimicrobiana.
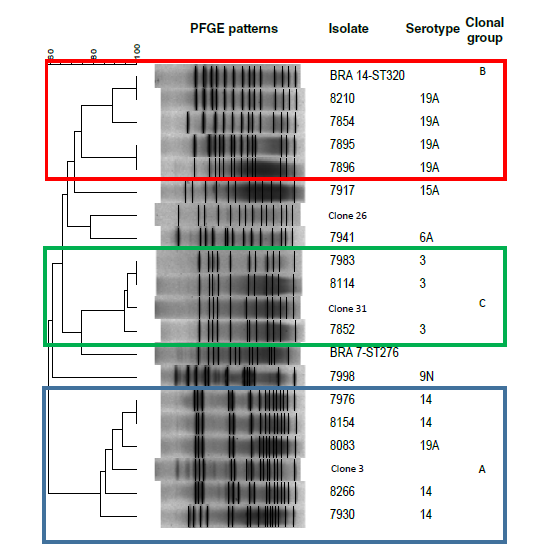
Resultados. De 1.343 casos sospechosos de neumonía bacteriana, 654 (48,7 %) fueron probables, el 84 % tenía el esquema de vacunación completo para la edad contra Haemophilus influenzae de tipo b, y el 87 %, contra neumococo. En 619 (94,6 %) pacientes se hizo hemocultivo y 41 (6,6 %) fueron positivos. S. pneumoniae se aisló en 17 (41 %) casos. El serotipo más frecuente fue el 19A, en cinco pacientes (29,4 %), en tanto que cuatro aislamientos de spn19A fueron relacionados con el clon ST320. La tasa de incidencia de neumonía bacteriana probable fue de 7,3 casos/100 pacientes hospitalizados. La letalidad fue de 2,1 %. Hubo 22 casos sospechosos de meningitis bacteriana, 12 (54 %) probables, y cuatro (33 %) confirmados: dos por Escherichia coli y dos por Neisseria meningitidis del grupo C. La incidencia de meningitis bacteriana probable fue de 0,14/100 pacientes hospitalizados.
Conclusión. Los serotipos 19A y 3 de S. pneumoniae fueron la causa más frecuente de neumonía. El Spn19A se relacionó con el clon ST320 mulitirresistente. El fortalecimiento continuo de la vigilancia centinela permitirá entender el impacto de la vacunación.
Descargas
Referencias bibliográficas
Jakhar SK, Pandey M, Shah D, Ramachandran VG, Saha R, Gupta GP. Etiology and riskfactors determining poor outcome of severe pneumonia in under-five children. Indian J Pediatr. 2018;85:20-4. https://doi.org/10.1007/s12098-017-2514-y
Wahl B, O’Brien KL, Greenbaum A, Majumder A, Liu L, Chu Y, et al. Burden of Streptococcus pneumoniae and Haemophilus influenzae type b disease in children in the era of conjugate vaccines: Global, regional, and national estimates for 2000-15. Lancet Glob Health. 2018;6:e744–57. https://doi.org/10.1016/S2214-109X(18)30247-X
Nascimento-Carvalho AC, Ruuskanen O, Nascimento-Carvalho CM. Comparison of the frequency of bacterial and viral infections among children with community-acquired pneumonia hospitalized across distinct severity categories: A prospective cross-sectional study. BMC Pediatr. 2016;22:105. https://doi.org/10.1186/s12887-016-0645-3
Das A, Patgirl SJ, Saikia L, Dowerah P, Nath R. bacterial pathogens associated with community-acquired pneumonia in children aged below five years. Indian Pediatr. 2016;53:225-7. https://doi.org/10.1007/s13312-016-0825-0
Instituto Nacional de Salud. Informe de evento de meningitis bacteriana y enfermedad meningocócica. 2018. Accessed on: June 5, 2019. Available from: https://www.ins.gov.co/buscador-eventos/Informesdeevento/MENINGITIS%20BACTERIANA_2018.pdf
Instituto Nacional de Salud. Protocolo de vigilancia en salud pública: meningitis bacteriana y enfermedad meningocóccica Código 535. Accessed on: June 5, 2019. Available from: https://www.ins.gov.co/buscador-eventos/Lineamientos/Pro_Meningitis.pdf
Instituto Nacional de Salud. Protocolo de vigilancia en salud pública: infección respiratoria aguda IRA. Códigos 345,348, 591,995. Accessed on: May 10, 2018. Available from: https://www.ins.gov.co/BibliotecaDigital/PRO-Infecci%C3%B3n-respiratoria-aguda.pdf
World Health Organization. Estimating meningitis hospitalization rates for sentinel hospitals conducting surveillance of invasive bacterial vaccine preventable diseases. Wkly Epidemiol Rec. 2013;43:471-6.
Wysocki J, Sluzewski W, Gutterman E, Jouve S, Moscariello M, Balter I. Active hospitalbased surveillance of invasive pneumococcal disease and clinical pneumonia in infants and young children in two Polish counties. Arch Med Sci. 2016;12:629-38. https://doi.org/10.5114/aoms.2016.59936
Ellis SM, Flowers C. The WHO manual of diagnostic imaging: Radiographic anatomy and interpretation of the chest and the pulmonary system 2006. Accessed on: November 14, 2018. Available from: http://apps.who.int/iris/bitstream/10665/43293/1/9
Clinical Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing: Twenty-sixth Informational Supplement. CLSI document M100-S21. Wayne, PA: CLSI; 2016.
Vela MC, Fonseca N, Di Fabio JL, Castañeda E. Presence of international multiresistant clones of Streptococcus pneumoniae in Colombia. Microb Drug Resist. 2001;7:153-64. https://doi.org/10.1089/10766290152045020
Instituto Nacional de Salud. Informe Nacional SIREVA II Colombia 2006-2015. Accessed on: March 17, 2016. Available from: http://www.ins.gov.co/tramites-y-servicios/examenesde-inter%C3%A9s-en-salud-ublica/Microbiologa/Informe%20Web%20S%20%20pneumoniae%202006-2015.pdf
World Health Organization. Invasive bacterial vaccine preventable disease sentinel hospital surveillance network: Summary of a strategic review and next steps, 2008-2014. Wkly Epidemiol Rec. 2014;89:545-60.
Acuerdo 366 del Consejo Nacional de Seguridad Social en Salud (CNSSS). Accessed on: November 14, 2018. Available from: http://fapp.saludcapital.gov.co/estadisticos/pai/BASES/DOCUMENTOS%20PAI/STAND%20POLITICO-NORMATIVO/Acuerdos/Acuerdo%20366%20de%202007.pdf
Ministerio de Salud de Colombia. Resolución 1736 del 20 de mayo de 2010. Accessed on: November 14, 2018. Available from: https://www.icbf.gov.co/cargues/avance/docs/resolucion_minproteccion_1736_2010.htm
Liu L, Oza S, Hogan D, Perin J, Rudan I, Lawn JE, et al. Global, regional, and national causes of child mortality. Lancet. 2015;385:430-40. https://doi.org/10.1016/S0140-6736(14)61698-6
Kim GL, Seon SH, Rhee Dk. Pneumonia and Streptococcus pneumoniae vaccine. Arch Pharm Res. 2017;40:885-93. https://doi.org/10.1007/s12272-017-0933-y
Benavides JA, Ovalle OO, Salvador GR, Gray S, Isaacman D, Rodgers GL. Populationbased surveillance for invasive pneumococcal disease and pneumonia in infants and young children in Bogotá , Colombia. Vaccine. 2015;30:5886-92. https://doi.org/10.1016/j.vaccine.2012.03.054
Pombo-March MDFB, Sant’Anna CC. Signs and symptoms indicative of community-acquired pneumonia in infants under six months. Braz J Infect Dis. 2005;9:150-5. https://doi.org/10.1590/s1413-86702005000200005
Shah SN, Bachur RG, Simel DL, Neuman MI. Does this child have pneumonia? The rational linical examination systematic review. JAMA. 2017;318:462-71. https://doi.org/ 10.1001/jama.2017.9039
Mahomed N, Madhi SA. Radiologic diagnosis of chest infection in children: WHO end-point consolidation. Pediatr Radiol. 2014;44:685-6. https://doi.org/10.1007/s00247-014-2933-0
Lakhani D, Muley P. The association of positive chest radiograph and laboratory parameters with community acquired pneumonia in children. J Clin Diagn Res. 2013;7:1629-31. https://doi.org/10.7860/JCDR/2013/5132.3222
Ferrero F, Torres F, Noguerol E, González N, Lonegro L, Chiolo MJ, et al. Evaluation of two standarized methods for chest radiographs interpretation in children with pneumonia. Arch Argent Pediatr. 2008;106:510-4. https://doi.org/10.1590/S0325-00752008000600007
Wingerter SL, Bachur RG, Monuteaux MC, Neuman MI. Application of the World Health Organization criteria to predict radiographic pneumonia in a US-based pediatric emergency department. Pediatr Infect Dis J. 2012;31:561-4. https://doi.org/10.1097/INF.0b013e31824da716
Cherian T, Mulholland EK, Carlin JB, Ostensen H, Amin R, De Campo M, et al. Standardized interpretation of paediatric chest radiographs for the diagnosis of pneumonia in epidemiological studies. Bull World Health Organ. 2005;83:353-9.
Fancourt N, Deloria-Knoll M, Barger-Kamate B, de Campo J, de Campo M, Diallo M, et al. Standardized interpretation of chest radiographs in cases of pediatric pneumonia from the PERCH Study. Clin Infect Dis. 2017;64(Suppl.3):S253-61. https://doi.org/10.1093/cid/cix082
Ben Shimol S, Dagan R, Givon-Lavi N, Tal A, Aviram M, Bar-Ziv J, et al. Evaluation of the World Health Organization criteria for chest radiographs for pneumonia diagnosis in children. Eur J Pediatr. 2012;171:369-74. https://doi.org/10.1007/s00431-011-1543-1
Fancourt N, Deloria Knoll M, Baggett HC, Brooks WA, Feikin DR, Hammitt LL, et al. Chest radiograph findings in childhood pneumonia cases from the multisite PERCH Study. Clin Infect Dis. 2017;64(Suppl.3):S262-70. https://doi.org/10.1093/cid/cix089
Jain S, Williams DJ, Arnold SR, Ampofo K, Bramley AM, Reed C, et al. Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med. 2015;372:835-45. https://doi.org/10.1056/NEJMoa1405870
Shah SS, Dugan MH, Bell LM, Grundmeier RW, Florin TA, Hines EM, et al. Blood culture in the emergency department evaluation of childhood pneumonia. Ped Infect Dis J. 2011;6:475-9. https://doi.org/10.1097/INF.0b013e31820a5adb
Obaro SK, Monteil MA, Henderson DC. The pneumococcal problem. BMJ. 1996;312:1521-55. https://doi.org/10.1136/bmj.312.7045.1521
Davis TR, Evans HR, Murtas J, Weisman A, Francis JL, Khan A. Utility of blood cultures in children admitted to hospital with community-acquired pneumonia. J Paediatr Child Health. 2017;53:232-6. https://doi.org/10.1111/jpc.13376
Tiewsoh K, Lodha R, Pandey RM, Broor S, Kalaivani M, Kabra SK. Factors determining the outcome of children hospitalized with severe pneumonia. BMC Pediatr. 2009;9:1-8. https://doi.org/10.1186/1471-2431-9-15
Ministerio de Salud y Protección Social. Dirección de epidemiologia y demografía. Análisis de la situación en salud Colombia 2017. Accessed on: September 5, 2019. Available from: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/ED/PSP/asisnacional-2017.pdf
Andrade AL, Oliveira R, Vieira MA, Minamisava R, Pessoa V, Brandileone MC, et al. Population-based surveillance for invasive pneumococcal disease and pneumonia in infants and young children in Goiânia, Brazil. Vaccine. 2012;30:1901-9. https://doi.org/10.1016/j.vaccine.2011.12.012
Secretaría de Salud de Bogotá. Infecciones respiratorias agudas menor 5 años. Accessed on: June 5, 2019. Availaible from: https://saludata.saludcapital.gov.co/osb/index.php/datosde-salud/enfermedades-trasmisibles/mortalidad-ira/
Cilloniz C, Martin-Loeches I, García-Vidal C, San José A, Torres A. Microbial Etiology of pneumonia: Epidemiology, diagnosis and resistance patterns. Int J Mol Sci. 2016;17:2120. https://doi.org/10.3390/ijms17122120
Parra EL, Ramos V, Sanabria O Moreno J. Serotype and genotype distribution among invasive Streptococcus pneumoniae isolates in Colombia, 2005-2010. PLoS One. 2014;9:e84993. https://doi.org/10.1371/journal.pone.0084993
Instituto Nacional de Salud. Streptococcus pneumoniae. Distribución de los aislamientos invasores por año de vigilancia, departamento, grupos de edad, serotipos y sensibilidad antimicrobiana 2006-2016. Accessed on: November 14, 2018. Available from: https://www.ins.gov.co/buscador-eventos/Informacin%20de%20laboratorio/Informe%20Nacional%20SIREVA%20II%20S.%20pneumoniae%202006-2016.docx.pdf
Mackenzie GA, Hill PC, Jeffries DJ, Hossain I, Uchendu U, Ameh DE, et al. Effect of the introduction of pneumococcal conjugate vaccination on invasive pneumococcal disease in The Gambia: A population-based surveillance study. Lancet Infect Dis. 2016;16:703-11. https://doi.org/10.1016/S1473-3099(16)00054-2
Cassiolato AP, Almeida SCG, Andrade AL, Minamisava R, Brandileone MC. Expansion of the multidrug-resistant clonal complex 320 among invasive Streptococcus pneumoniae serotype 19A after the introduction of a ten-valent pneumococcal conjugate vaccine in Brazil. PLoS ONE. 2018;13:e0208211. https://doi.org/10.1371/journal.pone.0208211
Balsells E, Guillot L, Nair H, Kyaw MH. Serotype distribution of Streptococcus pneumoniae causing invasive disease in children in the post-PCV era: A systematic review and metaanalysis. PLoS ONE. 2017;12:e0177113. https://doi.org/10.1371/journal.pone.0177113
Camacho G, Imbachi LF, Leal Al, Moreno VM, Patiño J, Gutiérrez I, et al. Emergence of Streptococcus pneumoniae serotype 19 A (Spn 19A) in the pediatric population in Bogotá, Colombia as the main cause of invasive pneumococcal disease after the introduction of PCV10. Hum Vaccin Immunother. 2020;16:2300-6.
https://doi.org/10.1080/21645515.2019.1710411
Leal AL, Montanez AM, Buitrago G, Patiño J, Camacho G, Moreno V. Impact of ten-valent pneumococcal conjugate vaccine introduction on serotype distribution trends in Colombia: An interrupted time-series analysis. Open Forum Infect Dis. 2017:4(Suppl.1):S463. https://doi.org/10.1093/ofid/ofx163.1182
Agudelo CI, De Antonio R, Castañeda E. Streptococcus pneumoniae serotype 19A in Latin America and the Caribbean 2010-2015: A systematic review and a time series analysis. Vaccine. 2018;36:4861-74. https://doi.org/10.1016/j.vaccine.2018.06.068
Waight PA, Andrews NJ, Ladhani SN, Sheppard CL, Slack MPE, Miller E. Effect of the 13-valent pneumococcal conjugate vaccine on invasive pneumococcal disease in England and Wales 4 years after its introduction: An observational cohort study. Lancet Infect Dis. 2015;15:535-43. https://doi.org/10.1016/S1473-3099(15)70044-7
Demczuk WHB, Martin I, Griffith A, Lefebvre B, McGeer A, Lovgren M, et al. Serotype distribution of invasive Streptococcus pneumoniae in Canada after the introduction of the 13-valent pneumococcal conjugate vaccine, 2010-2012. Can J Microbiol. 2013;59:778-88. https://doi.org/10.1139/cjm-2013-0614
Harboe ZB, Dalby T, Weinberger DM, Benfield T, Molbak K, Slotved HC, et al. Impact of 13-valent pneumococcal conjugate vaccination in invasive pneumococcal disease incidence and mortality. Clin Infect Dis. 2014;59:1066-73. https://doi.org/10.1093/cid/ciu524
Ben-Shimol S, Greenberg D, Givon-Lavi N, Schlesinger Y, Somekh E, Aviner S, et al. Early impact of sequential introduction of 7-valent and 13-valent pneumococcal conjugate vaccine on IPD in Israeli children <5 years: An active prospective nationwide surveillance. Vaccine. 2014;32:3452-9. https://doi.org/10.1016/j.vaccine.2014.03.065
Lepoutre A, Varon E, Georges S, Dorléans F, Janoir C, Gutmann L, et al. Impact of the pneumococcal conjugate vaccines on invasive pneumococcal disease in France, 2001-2012. Vaccine. 2015;33:359-66. https://doi.org/10.1016/j.vaccine.2014.11.011
Alarcón-Rodríguez ZK, Duarte C, Sanabria O, Moreno J. Genotipos de Streptococcus pneumoniae serotipo 3 en aislamientos invasivos en Colombia. Biomédica. 2021;41:338-46.https://doi.org/10.7705/biomedica.5407
Isozumi R, Ito Y, Ishida T, Hirai T, Ito I, Maniwa K, et al. Molecular characteristics of serotype 3 Streptococcus pneumoniae isolates among community-acquired pneumonia patients in Japan. J Infect Chemother. 2008;14:258-61. https://doi.org/ 10.1007/s10156-008-0600-9
Ramachandran P, Fitzwater SP, Aneja S, Verghese VP, Kumar V, Neduchelian K, et al. Prospective multi-centre sentinel surveillance for Haemophilus influenzae type b & other bacterial meningitis in Indian children. Indian J Med Res. 2013;137:712–20.
Manoharan A, Manchanda V, Balasubramanian S, Lalwani S, Modak M, Bai S, et al. Invasive pneumococcal disease in children aged younger than 5 years in India: A surveillance study. Lancet Infect Dis. 2017;17:305-12. https://doi.org/ 10.1016/S1473-3099(16)30466-2
Instituto Nacional de Salud. Informe del evento meningitis aguda bacteriana (MBA), hasta el periodo epidemiológico XIII, Colombia, 2016. Accessed on: November 10, 2018. Available from: https://www.ins.gov.co/buscador-eventos/Informesdeevento/Meningitis 2016.pdf
Algunos artículos similares:
- Eliana Parra, Elizabeth Castañeda, Jaime Moreno, Identificación de Haemophilus influenzae, Streptococcus pneumoniae y Neisseria meningitidis por reacción en cadena de la polimerasa , Biomédica: Vol. 27 Núm. 3 (2007)
- Daniel Echeverri, María de los Ángeles Vargas, Lorena Matta, Fernando Rosso, Janier Daniel Segura, Infección invasiva por Streptococcus pneumoniae: reporte de caso de un paciente con síndrome de Austrian , Biomédica: Vol. 35 Núm. 1 (2015)
- Claudia Calderón, Rodolfo Dennis, Costos económicos de neumonía adquirida en comunidad, meningitis y bacteriemia por Streptococcus pneumoniae en una población adulta que requirió hospitalización en Bogotá, Colombia , Biomédica: Vol. 34 Núm. 1 (2014)
- Carolina Firacative, Jaime Moreno, Elizabeth Castañeda, Caracterización molecular de aislamientos invasores colombianos de Streptococcus pneumoniae serotipo 5 recuperados entre 1994 y 2004. , Biomédica: Vol. 26 Núm. 2 (2006)
- Clara Inés Agudelo, Jaime Moreno, Olga Marina Sanabria, María Victoria Ovalle, José Luis Di Fabio, Elizabeth Castañeda, Streptococcus pneumoniae: evolución de los serotipos y los patrones de susceptibilidad antimicrobiana en aislamientos invasores en 11 años de vigilancia en colombia (1994 -2004). , Biomédica: Vol. 26 Núm. 2 (2006)
- César A. Arias, Marylin Hidalgo, Jinnethe Reyes, Ana María Cárdenas, Lorena Díaz, Sandra Ríncon, Natasha Vanegas, Paula Lucía Díaz, Elizabeth Castañeda, Perfiles de resistencia a fluoroquinolonas en aislamientos clínicos de cocos Gram positivos provenientes de hospitales colombianos, 1994-2004 , Biomédica: Vol. 28 Núm. 2 (2008)
- Zonia Katerin Alarcón , Carolina Duarte, Olga Sanabria, Jaime Moreno, Genotipos del serotipo 3 de Streptococcus pneumoniae en aislamientos invasivos en Colombia , Biomédica: Vol. 41 Núm. 2 (2021)
- Lucía Carolina Leal-Esteban, Jessica Lineth Rojas, Andrea Lizeth Jaimes, Juan David Montoya, Nilton Edu Montoya, Lily Leiva, Claudia Milena Trujillo-Vargas, Estandarización en Colombia de una prueba ELISA para la evaluación de los niveles séricos de anticuerpos IgG contra diez serotipos de Streptococcus pneumoniae , Biomédica: Vol. 32 Núm. 1 (2012)
- lngrid J. Peñuela, Aura Lucía Leal, Elizabeth Castañeda, Colonización nasofaríngea y resistencia antimicrobiana de Streptococcus pneumoniae en niños de una guardería en Santa Fe de Bogotá. , Biomédica: Vol. 19 Núm. 3 (1999)
- Jaime Moreno, Elizabeth Castañeda, Caracterización molecular de aislamientos invasores de Streptococcus pneumoniae resistentes a la penicilina recuperados de pacientes adultos. , Biomédica: Vol. 23 Núm. 1 (2003)
Datos de los fondos
| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |

























