Epidemiology of bacterial infections in patients with liver cirrhosis. Experience in a Spanish tertiary health center
Abstract
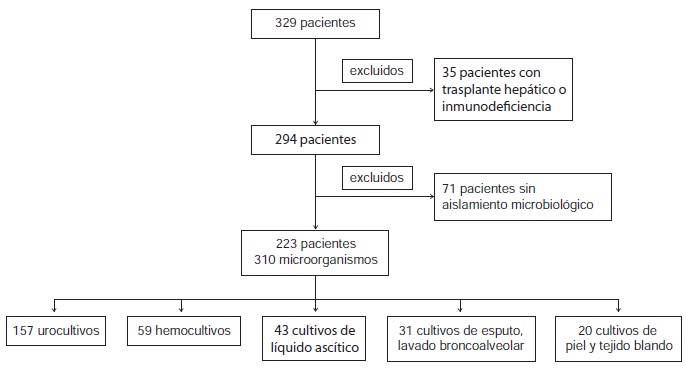
Introduction: Bacterial infections represent a serious complication of liver cirrhosis. Traditionally, Gram negative bacteria have been described as the microorganisms responsible for the majority of the infections. However, in the past few years, changes in the microbiological spectrum have been described, and multiresistant bacteria are observed more frequently. Objective: To assess the proportion of patients with infections caused by multiresistant bacteria admitted to our hospital, and to obtain information about their epidemiology, risk factors and clinical impact. Materials and methods: We performed a retrospective evaluation of 294 cirrhotic patients admitted to our unit due to infection between June, 2011, and June, 2013. Results: We isolated 310 microorganisms from 294 patients; 109 (35.2%) were Gram positive, 167 (53.9%), Gram negative, and 34, fungi (11%). As for the microbiological agents, the most frequent was Escherichia coli (98 isolations). The infection was community-acquired in 22.9% of cases, healthcareassociated in 38.1% and nosocomial in 39%. Worse liver infections and septic shock were more frequent among patients with multiresistant isolates (p=0.05); and intrahospital mortality was also higher among them (p=0.017). Previous hospital admission, antibiotic treatment 60 days before, nosocomial or healthcare-associated acquisition and bacterial isolation in control cultures were identified as possible risk factors for the development of multiresistant infection. Discussion: The results of our study confirm that important changes have ocurred in the microbiological spectrum of bacterial infections in patients with liver cirrhosis. Multiresistant bacteria are associated with high morbidity and mortality, as well as failure of traditional antibiotic treatment. Successfull control of the infection requires an early identification of patients at risk.
Downloads
References
Gustot T, Durand F, Lebrec D, Vincent JL, Moreau R. Severe sepsis in cirrhosis. Hepatology. 2009;50:2022-33. http://dx.doi.org/10.1002/hep.23264
Jalan R, Fernández J, Wiest R, Schnabl B, Moreau R, Angeli P, et al . Bacterial infections in cirrhosis: A position statement based on the EASL Special Conference 2013. Hepatology. 2014;60:1310-24. http://dx.doi.org/10.1016/j.jhep.2014.08.010
Borzio M, Salerno F, Piantoni L, Cazzaniga M, Angeli P, Bissoli F, et al . Bacterial infection in patients with advanced cirrhosis: A multicentre prospective study. Dig Liver Dis. 2001;33:41-8. http://dx.doi.org/10.1016/S1590-8658(01)80134-1
Bauer TM, Steinbruckner B, Brinkmann FE, Ditzen AK, Schwacha H, Aponte JJ, et al . Small intestinal bacterial overgrowth in patients with cirrhosis: Prevalence and relation with spontaneous bacterial peritonitis. Am J Gastroenterol. 2001;96:2962-7. http://dx.doi.org/10.1111/j.1572-0241.2001.04668
Caly WR, Strauss E. A prospective study of bacterial infections in patients with cirrhosis. J Hepatol. 1993;18: 353-8. http://dx.doi.org/10.1016/S0168-8278(05)80280-6
Pleguezuelo M, Benítez JM, Jurado J, Montero JL, De la Mata M. Diagnosis and management of bacterial infections in descompensated cirrhosis. World J Hepatol. 2013;5:16-25. http://dx.doi.org/10.4254/wjh.v5.i1.16
Fernández J, Navasa M, Gómez J, Colmenero J, Vila J, Arroyo V, et al . Bacterial infections in cirrhosis: Epidemiological changes with invasive procedures and norfloxacin prophylaxis. Hepatology. 2002;35:140-8. http://dx.doi.org/10/S0270913902984429
Fernández J, Acevedo J, Castro M, García O, Rodríguez-de Lope C, Roca D, et al . Prevalence and risk factors of infections by multiresistant bacteria in cirrosis: A prospective study. Hepatology. 2012;55:1551-61. http://dx.doi.org/10.1002/hep.25532
Tandon P, Delisle A, Topal JE, García-Tsao G. High prevalence of antibiotic-resistant bacterial infections among patients with cirrhosis at a US Liver Center. Clin Gastroenterol Hepatol. 2012;10:1291-8. http://dx.doi.org/10.1016/j.cgh.2012.08.017
European Association for the Study of the Liver. EASL clinical practice guidelines on the management of ascites, spontanous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53:397-417. http://dx.doi.org/10.1016/j.jhep.2010.05.004
Mandell GL, Bennet JE, Dolin R. Principles and Practice of Infectious Diseases. 7th edition. Philadelphia, PA: Churchill Livingstone Elsevier; 2010.
Tandon P, García-Tsao G. Bacterial infections, sepsis, and multiorgan failure in cirrhosis. Semin Liver Dis. 2008;28:26-42. http://dx.doi.org/10.1055/s-2008-1040319
Hawkey PM, Jones AM. The changing epidemiology of resistance. J Antimicrob Chemother. 2009;64(Suppl.1):i3-10. http://dx.doi.org/10.1093/jac/dkp256
Rodríguez-Baño J, Alcalá J, Cisneros JM, Grill F, Oliver A, Horcajada JP. Escherichia coli producing SHV-type extended-spectrum beta-lactamase is a significant cause of community-acquired infection. J Antimicrob Chemother. 2009;63:781-4. http://dx.doi.org/10.1093/jac/dkp028
Umgelter A, Reindl W, Miedanes M, Schmid RM, Huber W. Failure of current antibiotic first-line regimens and mortality in hospitalized patiens with spontaneous bacterial peritonitis. Infection. 2009;37:2-8. http://dx.doi.org/10.1007/s15010-008-8060-9
Rodríguez-Baño J, Pascual A. Clinical significance of extended-spectrum-beta-lactamases. Expert Rev Anti Infect Ther. 2008;6:671-83. http://dx.doi.org/10.1586/14787210.6.5.671
Martínez-Martínez L, Calvo J. El problema creciente de la resistencia antibiótica en bacilos gramnegativos: situación actual. Infecc Microbiol Clin. 2010;28(Supl.2):25-31. http://dx.doi.org/10.1016/S0213-005X(10)70027-6
Kalambokis GN, Mouzaki A, Tsianos EV. Rifaximin for the prevention of spontaneous bacterial peritonitis. World J Gastroenterol. 2012;18:1700-2. http://dx.doi.org/10.3748/wjg.v18.i14.1700
Kalambokis GN, Mouzaki A, Rodi M, Pappas K, Fotopoulos A, Xourgia X, et al . Rifaximin improves systemic hemodynamic and renal function in patients with alcohol related cirrhosis. Clin Gastroenterol Hepatol. 2012;10:815-8. http://dx.doi.org/10.1016/j.cgh.2012.02.025
Some similar items:
- Carlos Carvajal, Carlos Pacheco, Fabián Jaimes, Clinical and demographic profile and risk factors for Clostridium difficile infection , Biomedica: Vol. 37 No. 1 (2017)
- Mauricio Beltrán, María Cristina Navas, María Patricia Arbeláez, Jorge Donado, Sergio Jaramillo, Fernando De la Hoz, Cecilia Estrada, Lucía del Pilar Cortés, Amalia de Maldonado, Gloria Rey, Seroprevalence of hepatitis B virus and human immunodeficiency virus infection in a population of multiply-transfused patients in Colombia , Biomedica: Vol. 29 No. 2 (2009)
- Ligia Inés Moncada, Sandra Milena Rios, Julián Alfredo Fernández, Fabio Rivas, María Luz Sáenz, Pediculosis prevalence and associated risk factors in a nursery school, Bogotá, Colombia , Biomedica: Vol. 28 No. 2 (2008)
- Alicia Norma Alayón, Saudith Ariza, Karen Baena, Lina Lambis, Lina Martínez, Lourdes Benítez, Active search and assessment of cardiovascular risk factors in young adults, Cartagena de Indias, 2007 , Biomedica: Vol. 30 No. 2 (2010)
- María del Pilar Chaves, Julián Alfredo Fernández, Isabel Ospina, Myriam Consuelo López, Ligia Moncada, Patricia Reyes, Giardia duodenalis prevalence and associated risk factors in preschool and school-age children of rural Colombia , Biomedica: Vol. 27 No. 3 (2007)
- Elpidia Poveda, Alexandra Cuartas, Saralicia Guarín, Yibby Forero, Elsa Villarreal, Iron and vitamin A micronutrient status, risk factors for their deficiencies and anthropometric assessment in preschool child from Funza municipality, Colombia , Biomedica: Vol. 27 No. 1 (2007)
- Richard Hoyos, Lisandro Pacheco, Luz Adriana Agudelo, German Zafra, Pedro Blanco, Omar Triana, Seroprevalence of Chagas disease and associated risk factors in a population of Morroa, Sucre , Biomedica: Vol. 27 No. 1esp (2007): Enfermedad de Chagas
- Hollman Miller, Germán Gallego, Gerzaín Rodríguez, Clinical evidence of trachoma in Colombian Amerindians of the Vaupés Province , Biomedica: Vol. 30 No. 3 (2010)
- Constanza Pardo, Marion Piñeros, Teenage tobacco consumption in five Colombian cities , Biomedica: Vol. 30 No. 4 (2010)
- Gladys Acuña-González, Carlo E. Medina-Solís, Gerardo Maupomé, Mauricio Escoffie-Ramírez, Jesús Hernández-Romano, María de L. Márquez-Corona, Arturo J. Islas-Márquez, Juan J. Villalobos-Rodelo, Family history and socioeconomic risk factors for non-syndromic cleft lip and palate: A matched case-control study in a less developed country , Biomedica: Vol. 31 No. 3 (2011)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























