Severe malaria in pregnant women hospitalized between 2010 and 2014 in the Department of Antioquia (Colombia)
Abstract
Introduction: Malaria during pregnancy has a negative impact on maternal-neonatal health, with a high risk of clinic complications and mortality. High endemic areas are specially characterized by maternal anaemia and low birth weight. The clinical spectrum is little known in low endemic areas.
Objective: To clinically and epidemiologically characterize malaria episodes in hospitalized pregnant women in the Department of Antioquia (Colombia) in the period 2010-2014.
Materials and methods: Retrospective, cross-sectional, descriptive study with medical records of pregnant women with P. falciparum and P. vivax malaria. The WHO severe malaria diagnostic criteria and the Colombian Guía para la atención clínica integral del paciente con malaria (guidelines for comprehensive malaria treatment) were used.
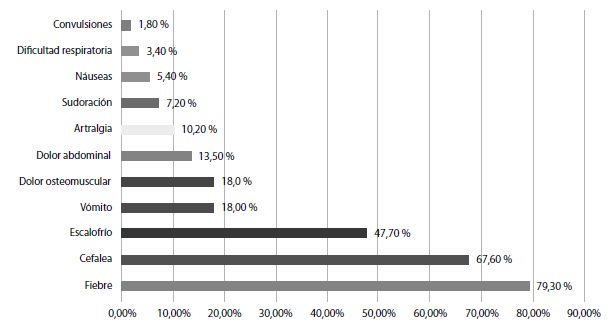
Results: We analyzed 111 cases, out of which 13.5% were classified as severe malaria according to the WHO criteria. Following the Colombian Guidelines, the proportion increased to 23.4%. Identified complications included hepatic dysfunction, anaemia, acidosis, and severe thrombocytopenia. No difference in the frequency of complications by Plasmodium species was observed; 39.4% of the cases presented general danger signs, pallor and jaundice being the most frequent; 40.5% showed danger signs for pregnancy, such as persistent headache, abdominal pain, and vaginal bleeding.
Conclusions: Severe malaria is a highly frequent event in pregnant women, without differences by Plasmodium species. It shows early recognizable dangers signs. Hospital under-reporting was identified in 88% of severe cases as well as a lack of laboratory tests for a more comprehensive diagnosis. A protocol for the clinical diagnosis of pregnant women with malaria is required.
Downloads
References
World Health Organization. World malaria report, 2015. Geneva. WHO; 2016. Fecha de consulta: 5 de marzo de 2018. Disponible en: http://apps.who.int/iris/bitstream/handle/10665/205559/WHO_HTM_GMP_2016.2_spa.pdf;jsessionid=DD8C013034924EE5A4599CEE0C450615?sequence=1
Dellicour S, Tatem AJ, Guerra CA, Snow RW, ter Kuile FO. Quantifying the number of pregnancies at risk of malaria in 2007: A demographic study. PLoS Med. 2010;7:e1000221. https://doi.org/10.1371/journal.pmed.1000221
Menéndez C, Mayor A. Congenital malaria: The least known consequence of malaria in pregnancy. Semin Fetal Neonatal Med. 2007:12:207-13. https://doi.org/10.1016/j.siny.2007.01.018
Desai M, ter Kuile FO, Nosten F, McGready R, Asamoa K, Brabin B, et al. Epidemiology and burden of malaria in pregnancy. Lancet Infect Dis. 2007;7:93-104. https://doi.org/10.1016/S1473-3099(07)70021-X
Steketee RW, Nahlen BL, Parise ME, Menéndez C. The burden of malaria in pregnancy in malaria-endemic areas. Am J Trop Med Hyg. 2001;64(Suppl.1):28-35.
Geertruyden JV, Ntakirutimana D, Erhart A, Rwagacondo C, Kabano A, D’Alessandro U. Malaria infection among pregnant women attending antenatal clinics in six Rwandan districts. Trop Med Int Health. 2005;10:681-8. https://doi.org/10.1111/j.1365-3156.2005.01431.x
World Health Organization. Severe falciparum malaria. Trans R Soc Trop Med Hyg. 2000;94(Suppl.1):1-90.
Nosten F, Rogerson SJ, Beeson JG, McGready R, Mutabingwa TK, Brabin B. Malaria in pregnancy and the endemicity spectrum: What can we learn? Trends Parasitol. 2004;20:425-32. https://doi.org/10.1016/j.pt.2004.06.007
Greenwood B, Alonso P, ter Kuile FO, Hill J, Steketee RW. Malaria in pregnancy: Priorities for research. Lancet Infect Dis. 2007;7:169-74. https://doi.org/10.1016/S1473-3099(07)70028-2
Ramal C, Pinedo P. Malaria en gestantes entre marzo del 2002 y julio del 2003: experiencia en el Hospital Regional de Loreto, Perú. Acta Med Peruana. 2008;25:220-3.
Chagas EC, do Nascimento CT, de Santana Filho FS, Bôtto-Menezes CH, Martínez-Espinosa FE. Impact of malaria during pregnancy in the Amazon region. Rev Panam Salud Pública. 2009;26:203-8.
Piñeros JG. Epidemiología de la malaria durante el embarazo. Med UIS. 2008;21:142-57.
Piñeros JG, Tobón A, Álvarez G, Portilla C, Blair S. Maternal clinical findings in malaria in pregnancy in a region of northwestern Colombia. Am J Trop Med Hyg. 2013;89:520-6. https://doi.org/10.4269/ajtmh.12-0205
Dirección Seccional de Salud, Departamento de Antioquia. Indicadores básicos de salud 2014. Fecha de consulta: 5 de marzo de 2018. Disponible en: http://diagnosticosalud.dssa.gov.co/#
World Health Organization. Tratamiento del paludismo grave. Manual Práctico. 3a edición. Ginebra: WHO; 2014. Fecha de consulta: 5 de abril de 2018. Disponible en: http://apps.who.int/medicinedocs/documents/s20170es/s20170es.pdf
Organización Panamericana de la Salud. Guía para atención clínica integral del paciente con malaria. Bogotá: Ministerio de Protección Social; 2010. Fecha de consulta: 23 de marzo de 2018. Disponible en: https://www.paho.org/coL/index.php?option=com_docman&view=download&category_slug=publicaciones-ops-oms-colombia&alias=1220-guia-para-la-atencion-clinica-integral-del-paciente-con-malaria&Itemid=688
Tobón A. Signos de peligro en el paciente con malaria. Biomédica. 2009;29:320-9. https://doi.org/10.7705/biomedica.v29i2.33
Menéndez C, D’Alessandro U, ter Kuile FO. Reducing the burden of malaria in pregnancy by preventive strategies. Lancet Infect Dis. 2007;7:126-35. https://doi.org/10.1016/S1473-3099(07)70024-5
Fernández RD, García Y, Alger J. Malaria y embarazo: observaciones clínicoepidemiológicas en dos zonas geográficas de Honduras. Rev Med Hondur. 2001;69:8-18.
Cottrell G, Moussiliou A, Luty AJ, Cot M, Fievet N, Massougbodji A, et al. Submicroscopic Plasmodium falciparum infections are associated with maternal anemia, premature births, and low birth weight. Clin Infect Dis. 2015;60:1481-8. https://doi.org/10.1093/cid/civ122
Gavina K, Gnidehou S, Arango E, Hamel-Martineau C, Mitran C, Agudelo O, et al. Clinical outcomes of submicroscopic infections and correlates of protection of VAR2CSA antibodies in a longitudinal study of pregnant women in Colombia. Infect Immun. 2018;86. https://doi.org/10.1128/IAI.00797-17.
Uneke CJ. Impact of placental Plasmodium falciparum malaria on pregnancy and perinatal outcome in sub-Saharan Africa: I: Introduction to placental malaria. Yale J Biol Med. 2007;80:39-50.
Khan WA, Galagan SR, Prue CS, Khyang J, Ahmed S, Ram M, et al. Asymptomatic Plasmodium falciparum malaria in pregnant women in the Chittagong Hill Districts of Bangladesh. PLoS One. 2014;9:e98442. https://doi.org/10.1371/journal.pone.0098442
Osorio L, Todd J, Bradley D. Ausencia de malaria asintomática en escolares de Quibdó, Chocó. Biomédica. 2004;24:13-9. https://doi.org/10.7705/biomedica.v24i1.1244
Galatas B, Bassat Q, Mayor A. Malaria parasites in the asymptomatic: Looking for the hay in the haystack. Trends Parasitol. 2016;32:296-308. https://doi.org/10.1016/j.pt.2015.11.015
World Health Organization. Guidelines for the treatment of malaria. Geneva: WHO; 2015. Fecha de consulta: 19 de marzo de 2018. Disponible en: http://apps.who.int/iris/bitstream/handle/10665/162441/9789241549127_eng.pdf?sequence=1
Berry I, Walker P, Tagbor H, Bojang K, Coulibaly SO, Kayentao K, et al. Seasonal dynamics of malaria in pregnancy in West Africa: Evidence for carriage of infections acquired before pregnancy until first contact with antenatal care. Am J Trop Med Hyg. 2018;98:534-542. https://doi.org/10.4269/ajtmh.17-0620
Tobón A, Giraldo-Castro C, Blair S. Utilidad de los signos clínicos y parasitológicos en el pronóstico de la malaria grave en Colombia. Biomédica. 2012;32:79-94. https://doi.org/10.7705/biomedica.v32i0.613
Some similar items:
- Johanna Ochoa, Lyda Osorio, Epidemiology of urban malaria in Quibdo, Choco. , Biomedica: Vol. 26 No. 2 (2006)
- Liliana Jazmín Cortés, Lyda Muñoz, Martha Stella Ayala, Comparison of methodologies for microscopic malaria diagnosis , Biomedica: Vol. 38 No. 2 (2018)
- Nohora Marcela Mendoza, Marisol García, Liliana Jazmín Cortés, Claudia Vela, Rigoberto Erazo, Pilar Pérez, Olga Lucía Ospina, Javier Darío Burgos, Evaluation of two rapid diagnostic tests, NOW® ICT Malaria Pf/Pv and OptiMAL®, for diagnosis of malaria , Biomedica: Vol. 27 No. 4 (2007)
- Manuel Alberto Pérez, Liliana Jazmín Cortés, Ángela Patricia Guerra, Angélica Knudson, Carlos Usta, Rubén Santiago Nicholls, Efficacy of the amodiaquine+sulfadoxine-pyrimethamine combination and of chloroquine for the treatment of malaria in Córdoba, Colombia, 2006 , Biomedica: Vol. 28 No. 1 (2008)
- Sandra Milena Barrera, Manuel Alberto Pérez, Angélica Knudson, Rubén Santiago Nicholls, Ángela Patricia Guerra, Genotypic survery of Plasmodium falciparum based on the msp1, msp2 and glurp genes by multiplex PCR , Biomedica: Vol. 30 No. 4 (2010)
- Alberto Tobón-Castaño, Cecilia Giraldo-Castro, Silvia Blair, Prognostic value of clinical and parasitological signs for severe malaria in patients from Colombia , Biomedica: Vol. 32 (2012): Suplemento 1, Malaria
- Margarita Arboleda, María Fernanda Pérez, Diana Fernández, Luz Yaned Usuga, Miler Meza, Clinical and laboratory profile of Plasmodium vivax malaria patients hospitalized in Apartadó, , Biomedica: Vol. 32 (2012): Suplemento 1, Malaria
- Amanda Maestre, Jaime Carmona-Fonseca, Amanda Maestre, Alta frecuencia de mutaciones puntuales en pfcrt de Plasmodium falciparum y emergencia de nuevos haplotipos mutantes en Colombia , Biomedica: Vol. 28 No. 4 (2008)
- Alexandra Ríos, Gonzalo Álvarez, Silvia Blair, Ten years of chloroquine efficacy for uncomplicated Plasmodium vivax malaria treatment, Turbo, Antioquia, 2002 and 2011 , Biomedica: Vol. 33 No. 3 (2013)
- Juan Gabriel Piñeros, Margarita Arboleda, Juan Camilo Jaramillo, Silvia Blair, Report of five cases of severe neonatal Plasmodium vivax malaria in Urabá, Colombia , Biomedica: Vol. 28 No. 4 (2008)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























