Abdominal angiostrongyliasis, report of two cases and analysis of published reports from Colombia
Abstract
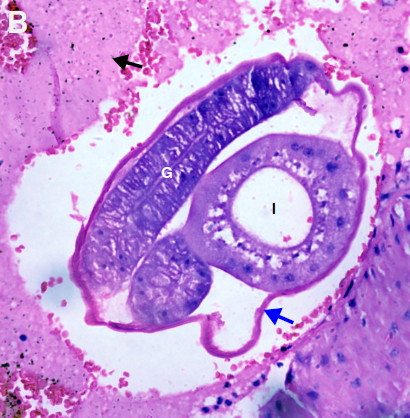
Abdominal angiostrongyliasis is a parasitic zoonosis, endemic in the American continent. Its etiological agent is Angiostrongylus costaricensis, a nematode whose definitive hosts are rats and other rodents and the intermediate hosts, slugs. Mammals acquire the infection by consuming vegetables contaminated with L3 larvae. The disease shows a heterogeneous clinical spectrum and given its low incidence its diagnosis is a great challenge.
In Colombia, the first case was reported in 1979 and until 1998, only five additional cases have been reported. However, in the last two decades, no new cases were reported. Here we discuss two cases of children from Huila and Caquetá departments who developed the disease. Both cases required long in-patient care and multiple surgical interventions. The diagnosis was achieved by histopathological observation of parasitic elements inside the mesenteric arteries. One of the children died while the other fully recovered.
We discuss the epidemiology, pathogenic cycle, clinical presentation, diagnosis, and prevention strategies of this disease paying particular attention to our patients’ features and the Colombian context.
Downloads
References
Qiao-Ping W, De-Hua L, Xing-Quan Z, Xiao-Guang C, Zhao-Rong L. Human angiostrongyliasis. Lancet Infect Dis. 2008;8:621-30. https://doi.org/10.1016/S1473-3099(08)70229-9
Morera P. Granulomas entéricos y linfáticos con intensa eosinofilia tisular producidos por un estrongilideo (Strongylata; Railliet y Henry, 1913): II. Aspecto parasitológico. Acta Médica Costarricense. 1967;10:257-65.
Morera P. Life history and redescription of Angiostrongylus costaricensis Moreira and Céspedes. Am J Trop Med Hyg. 1973;22:613-21. https://doi.org/10.4269/ajtmh.1973.22.613
Chen HT. A new pulmonary nematode of rats, Pulmonema cantonensis ng, nsp from Canton. Ann Parasitol. 1935;13:312-7.
Maldonado Jr A, Simões R, Thiengo S. Angiostrongyliasis in the Américas. In: Lorenzo-Morales J, editor. Zoonosis. Intechopen; 2012. p. 304-20. https://doi.org/10.5772/38632
Rebello KM, Menna-Barreto RF, Chagas-Moutinho VA, Mota EM, Perales J, Neves-Ferreira AG, et al. Morphological aspects of Angiostrongylus costaricensis by light and scanning electron microscopy. Acta Trop. 2013;127:191-8. https://doi.org/10.1016/j.actatropica.2013.05.002
Graeff-Teixeira C, Camillo-Coura L, Lenzi H. Abdominal angiostrongyliasis-an underdiagnosed disease. Mem Ins Oswaldo Cruz. 1987;82:353-4. https://doi.org/0.1590/s0074-02761987000800068
Morera P, Céspedes R. Angiostrongylus costaricensis n. sp. (Nematoda: Metastrongyloidea), a new lungworm occurring in man in Costa Rica. Rev Biol Trop. 1971;50:377-94.
Morera P, Amador J. Prevalencia de la angiostrongilosis abdominal y la distribución estacional de la precipitación. Revista Costarricense de Salud Pública. 1998;7:1-14.
Kaminsky R, Caballero R, Andrews K. Presencia de Angiostrongylus costaricensis en Honduras y sus relaciones agro-ecológicas y humanas. Parasitología al Día. 1995;19:81-90.
Romero-Alegría A, Belhassen-García M, Velasco-Tirado V, García-Mingo A, Alvela-Suárez L, Pardo-Lledias J, et al. Angiostrongylus costaricensis: Systematic review of case reports. Advances in Infectious Diseases. 2014;4:36-41. https://doi.org/10.4236/aid.2014.41007
Malek EA. Presence of Angiostrongylus costaricensis Morera and Céspedes 1971 in Colombia. Am J Trop Med Hyg. 1981;30:81-3. https://doi.org/10.4269/ajtmh.1981.30.81
Rodriguez R, Agostini AA, Porto SM, Olivaes AJ, Branco SL, Genro JP, et al. Dogs may be a reservoir host for Angiostrongylus costaricensis. Rev Inst Med Trop São Paulo. 2002;44:55-6. http://doi.org/10.1590/S0036-46652002000100010
Duarte Z, Morera P, Dávila P, Gantier JC. Angiostrongylus costaricensis natural infection in Vaginulus plebeius in Nicaragua. Ann Parasitol Hum Comp. 1992;67:94-6. https://doi.org/10.1051/parasite/199267394
Graeff-Teixeira C. Expansion of Achatina fulica in Brazil and potential increased risk for Angiostrongyliasis. Trans Royal Soc Trop Med Hyg. 2007;101:743-4. https://doi.org/10.1016/j.trstmh.2007.03.012
Rambo PR, Agostini AA, Graeff-Teixeira C. Abdominal angiostrongylosis in southern Brazil prevalence and parasitic burden in mollusk intermediate hosts from eighteen endemic foci. Mem Inst Oswaldo Cruz. 1997;92:9-14. https://doi.org/10.1590/S0074-02761997000100002
Thiengo SC, Fernandez MA, Torres EJ, Coelho PM, Lanfredi RM. First record of a nematode Metastrongyloidea (Aelurostrongylus abstrusus larvae) in Achatina (Lissachatina) Fulica (Mollusca, Achatinidae) in Brazil. J Invert Path. 2008;98:34-9. https://doi.org/10.1016/j.jip.2007.10.010
Neafie RC, Marty AM. Unusual infections in humans. Clin Microbiol Rev. 1993;6:34-56. https://doi.org/10.1128/cmr.6.1.34
Kramer MH, Greer GJ, Quiñónez JF, Padilla NR, Hernández B, Arana BA, et al. First reported outbreak of abdominal angiostrongyliasis. Clin Infect Dis. 1998;26:365-72. https://doi.org/10.1086/516325
Maurer RL, Graeff-Teixeira C, Thome JW, Chiaradia LA, Sugaya H, Yoshimura K. Natural infection of deroceras laeve (Mollusca: Gastropoda) with metastrongylid larvae in a transmission focus of abdominal angiostrongyliasis. Rev Inst Med Trop São Paulo. 2002;44:53-4. https://doi.org/10.1590/S0036-46652002000100009
Mojon M. Human angiostrongyliasis caused by Angiostrongylus costaricensis. Bull Acad Natl Med. 1994;178:625-31.
Zanini GM, Graeff-Teixeira C. Abdominal angiostrongyliasis: Its prevention by the destruction of infecting larvae in food treated with salt, vinegar or sodium hypochlorite. Rev Soc Bras Med Trop. 1995;28:389-92. https://doi.org/10.1590/s0037-86821995000400013
Magnaval JF. Parasitic dead-end: Update. Méd Trop (Mars). 2006;66:319-23.
Wu SS, French SW, Turner JA. Eosinophilic ileitis with perforation caused by Angiostrongylus (Parastrongylus) costaricensis. A case study and review. Arch Path Lab Med. 1997;121:989-91.
Vuong PN, Brama P, Bonète R, Houissa-Vuong S, Catanzano-Laroudie M, Baviera E. Necrotic eosinophilic angiitis with ileal perforation and peritonitis secondary to abdominal angiostrongyliasis. Presse Méd. 2002;31:1700-3.
Graeff-Teixeira C, Goulart AH, Brum CO, Laitano AC, Sievers-Tostes C, Zanini GM, et al. Longitudinal clinical and serological survey of abdominal angiostrongyliasis in Guaporé, Southern Brazil, from 1995 to 1999. Rev Soc Brasil Med Trop. 2005;38:310-5. https://doi.org/10.1590/S0037-86822005000400006
Rodriguez R, Dequi RM, Peruzzo L, Mesquita PM, Garcia E, Fornari F. Abdominal angiostrongyliasis: Report of two cases with different clinical presentations. Rev Inst Med Trop São Paulo. 2008;50:339-41. http://doi.org/10.1590/S0036-46652008000600005
Rodríguez G. Hematoquecia letal por angiostrongilosis abdominal. Biomédica. 2000;20:120-30. https://doi.org/10.7705/biomedica.v20i2.1055
Zúñiga SR, Cardona-López V, Alvarado D. Angiostrongilosis abdominal. Rev Med Hondur. 1983;51:184-92.
Loría-Cortés R, Lobo-Sanahuja JF. Clinical abdominal angiostrongylosis. Am J Trop Med Hyg. 1980;29:538-44. https://doi.org/10.4269/ajtmh.1980.29.538
Morera P, Bontempo I. Acción de algunos antihelmínticos sobre Angiostrongylus costaricensis. Rev Med Hosp Nac Niños Costa Rica. 1985;20:165-74.
Instituto Nacional de Salud. Concepto científico - consumo de caracol gigante africano y su implicación en salud. Bogotá: Minsalud, Instituto Nacional de Salud; 2017. 7-26.
Jurado LF, Palacios DM, López R, Baldión M, Matijasevic E. Cutaneous gnathostomiasis, first confirmed case in Colombia. Biomédica. 2015;35:462-70. https://doi.org/10.7705/biomedica.v35i4.2547
Linares E, Avendaño J, Martínez A, Rojas A. El caracol gigante africano, un visitante indeseado. Miniguías de campo del Instituto de Ciencias Naturales. No. 16. Bogotá: Universidad Nacional de Colombia; 2013. 5-12.
Some similar items:
- Ángela Londoño, Camila Pérez, Rodrigo Restrepo, Nathalie Morales, Miguel Martínez, Daniela Morales, Exogenous pigmentation by silver nitrate: Dermatological and toxicological aspects, case report , Biomedica: Vol. 41 No. 2 (2021)
- Juan Pablo Orozco-Hernández , Juan José Montoya-Martínez, Manuel Conrado Pacheco-Gallego, Mauricio Céspedes-Roncancio , Gloria Liliana Porras-Hurtado, SARS-CoV-2 and rhinovirus/enterovirus co-infection in a critically ill young adult patient in Colombia , Biomedica: Vol. 40 No. Supl. 2 (2020): SARS-CoV-2 y COVID-19
- José Y. Rodríguez, Carlos A. Álvarez-Moreno, Jorge A. Cortés, Gerson J. Rodríguez, Kelin Esquea, Heidy Pinzón, María J. Mendoza, Yiceth Acosta, Melioidosis in Colombia, description of a clinical case and epidemiological considerations , Biomedica: Vol. 39 No. Sp. 1 (2019): Suplemento 1, Microbiología médica, mayo
- Jaime E. Bernal, Martha Lucía Tamayo , Ignacio Briceño , Escilda Benavides , Newborn screening in Colombia: The experience of a private program in Bogotá , Biomedica: Vol. 44 No. 1 (2024)
- Raúl Murillo, Ricardo Cendales, Carolina Wiesner, Marion Piñeros, Sandra Tovar, Effectiveness of cytology-based cervical cancer screening in the Colombian health system , Biomedica: Vol. 29 No. 3 (2009)
- Sandra Lorena Girón, Julio César Mateus, Fabián Méndez, Impact of an open waste disposal site on the occurrence of respiratory symptoms and on health care costs of children , Biomedica: Vol. 29 No. 3 (2009)
- José Joaquín Carvajal, Ligia Inés Moncada, Mauricio Humberto Rodríguez, Ligia del Pilar Pérez, Víctor Alberto Olano, Characterization of Aedes albopictus (Skuse, 1894) (Diptera:Culicidae) larval habitats near the Amazon River in Colombia , Biomedica: Vol. 29 No. 3 (2009)
- Andrés Páez, Gloria Rey, Carlos Agudelo, Alvaro Dulce, Edgar Parra, Hernando Díaz-Granados, Damaris Heredia, Luis Polo, Outbreak of urban rabies transmitted by dogs in Santa Marta, northern Colombia , Biomedica: Vol. 29 No. 3 (2009)
- Patricia Escobar, Katherine Paola Luna, Indira Paola Hernández, César Mauricio Rueda, María Magdalena Zorro, Simon L. Croft, In vitro susceptibility of Trypanosoma cruzi strains from Santander, Colombia, to hexadecylphosphocholine (miltefosine), nifurtimox and benznidazole , Biomedica: Vol. 29 No. 3 (2009)
- Mauricio Beltrán, María Cristina Navas, María Patricia Arbeláez, Jorge Donado, Sergio Jaramillo, Fernando De la Hoz, Cecilia Estrada, Lucía del Pilar Cortés, Amalia de Maldonado, Gloria Rey, Seroprevalence of hepatitis B virus and human immunodeficiency virus infection in a population of multiply-transfused patients in Colombia , Biomedica: Vol. 29 No. 2 (2009)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























