Factors associated with functional loss among community-dwelling Mexican older adults
Abstract
Introduction: Functional status decline is related to many negative outcomes.
Objective: To explore the relationship of sociodemographic, medical, and psychological factors with the incidence of functional status decline in Mexican older adults.
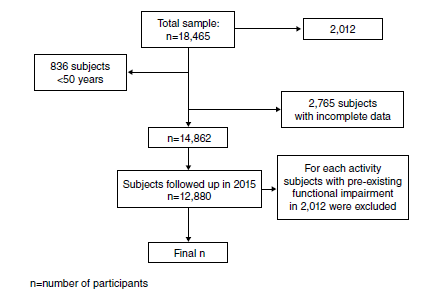
Materials and methods: Data from the 2012 and 2015 waves of the Mexican Health and Aging Study (MHAS) survey were analyzed. Participants with previous functional status decline at baseline were excluded. We assessed functional status decline individually with activities of daily living (ADL) and instrumental ADL (IADLs) in an individual way.
Results: Age was associated with functional limitations in ADL. Being male had an association with limitations for IADL. A poor financial situation and lower education related to higher limitations for ADL. Furthermore, pain, comorbidities, and depression were found to be independently associated with limitations in ADL. IADL limitation was associated with age, poor education, comorbidities, and depression, as well as cognitive impairment.
Conclusions: We found that factors such as age, financial status, educational level, pain, and the number of comorbidities were associated with the incidence of functional status decline. Pain had a greater association in the 3-year functional ADL decline incidence when compared with cognitive impairment. Studying functional decline by domains allowed us to find more detailed information to identify factors susceptible to intervention with the aim to reduce the incidence of functional status decline and dependence.
Downloads
References
Lee R. The demographic transition: Three centuries of fundamental change. J Econ Perspect 2003;17:167-90. https://doi.org/10.1257/089533003772034943
Wong R, Palloni A. Aging in Mexico and Latin America. International Handbook of Population Aging. Dordrecht: Springer Netherlands; 2009. p. 231-52.
Chatterji S, Byles J, Cutler D, Seeman T, Verdes E. Health, functioning, and disability in older adults - Present status and future implications. Lancet. 2015;385:563-75. https://doi.org/10.1016/S0140-6736(14)61462-84
Gómez F, Curcio C. Geriatrics In Latin America. En: Fillit HM, Rockwood K, Your J, editors. Brocklehurst’s Textbook of Geriatric Medicine and Gerontology. 8th edition. Philadelphia: Elsevier; 2017. p. 1017-22.
Gutiérrez-Robledo LM, García-Peña M del C, Arango-Lopera VE, Pérez-Zepeda MU. Geriatría para el médico familiar. Ciudad de México: Manual Moderno; 2012. p.1-20.
Stuck AE, Walthert JM, Nikolaus T, Büla CJ, Hohmann C, Beck JC. Risk factors for functional status decline in community-living elderly people: A systematic literature review. Soc Sci Med. 1999;48:445-69. https://doi.org/10.1002/art.20968
van Der Vorst A, Zijlstra GA, De Witte N, Duppen D, Stuck AE, Kempen GIJM, et al. Limitations in activities of daily living in community-dwelling people aged 75 and over: A systematic literature review of risk and protective factors. PLOS ONE. 2016;11:1-18. https://doi.org/10.1371/journal.pone.0165127
Storeng SH, Sund ER, Krokstad S. Factors associated with basic and instrumental activities of daily living in elderly participants of a population-based survey: The Nord-Trøndelag Health Study, Norway. BMJ Open. 2018;8:1-10. https://doi.org/10.1136/bmjopen-2017-018942
Spillman BC. Changes in elderly disability rates and the implications for health care utilization and cost. Milbank Q. 2004;82:157-94. https://doi.org/10.1111/j.0887-378x.2004.00305.x
World Health Organization. World report on disability. Geneva: World Health Organization; 2011. Accessed: October 27, 2019. Available at: http://www.who.int/disabilities/world_report/2011/report/en/
United Nations, Department of Economic and Social Affairs. Ageing and disability. Accessed: October 27, 2019. Available at: https://www.un.org/development/desa/disabilities/disabilityand-ageing.html
Fried TR, Bradley EH, Williams CS, Tinetti ME. Functional disability and health care expenditures for older persons. Arch Intern Med. 2001;161:2602. https://doi.org/10.1001/archinte.161.21.2602
Saunders P. The costs of disability and the incidence of poverty. Aust J Soc Issues. 2007;42:461-80. https://doi.org/10.1002/j.1839-4655.2007.tb00072.x
Desforges JF, Applegate WB, Blass JP, Williams TF. Instruments for the functional assessment of older patients. N Engl J Med.1990;322:1207-14. https://doi.org/10.1056/NEJM199004263221707
Wang L, van Belle G, Kukull WB, Larson EB. Predictors of functional change: A longitudinal study of nondemented people aged 65 and older. J Am Geriatr Soc. 2002;50:1525-34. https://doi.org/10.1046/j.1532-5415.2002.50408.x
Reyes-Ortiz CA, Ostir G V, Peláez M, Ottenbacher KJ. Cross-national comparison of disability in Latin American and Caribbean persons aged 75 and older. Arch Gerontol Geriatr. 2006;42:21-33. https://doi.org/10.1016/j.archger.2005.06.006
Fuentes-García A, Sánchez H, Lera L, Cea X, Albala C. Desigualdades socioeconómicas en el proceso de discapacidad en una cohorte de adultos mayores de Santiago de Chile. Gac Sanit. 2013;27:226-32. https://doi.org/10.1016/j.gaceta.2012.11.005
Wong R, Michaels-Obregon A, Palloni A. Cohort profile: The Mexican Health and Aging Study (MHAS). Int J Epidemiol. 2017;46:e-2. https://doi.org/10.1093/ije/dyu263
Katz S, FORD AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. JAMA. 1963;185:914. https://doi.org/10.1001/jama.1963.03060120024016
Trigás-Ferrín M, Ferreira-González L. Escalas de valoración funcional en ancionos. Galicia Clin. 2011;72:11-6.
Lawton MP, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179-86.
Cigolle CT, Langa KM, Kabeto MU, Tian Z, Blaum CS. Geriatric conditions and disability: The health and retirement study. Ann Intern Med. 2007;147:156. https://doi.org/10.7326/0003-4819-147-3-200708070-00004
Glosser G, Wolfe N, Albert ML, Lavine L, Steele JC, Calne DB, et al. Cross-cultural cognitive examination: Validation of a dementia screening instrument for neuroepidemiological research. J Am Geriatr Soc. 1993;41:931-9. https://doi.org/10.1111/j.1532-5415.1993.tb06758.x
Mejía-Arango S, Wong R, Michaels-Obregón A. Normative and standardized data for cognitive measures in the Mexican Health and Aging Study. Salud Pública Mex. 2015;57:90-6. https://doi.org/10.21149/spm.v57s1.7594
Mejía-Arango S, Gutiérrez LM. Prevalence and incidence rates of dementia and cognitive impairment no dementia in the Mexican population. J Aging Health. 2011;23:1050-74. https://doi.org/10.1177/0898264311421199
Aguilar-Navarro SG, Fuentes-Cantú A, Ávila-Funes JA, García-Mayo EJ. Validity and reliability of the screening questionnaire for geriatric depression used in the Mexican Health and Age Study. Salud Pública Mex. 2007;49:256-62. https://doi.org/10.1590/s0036-36342007000400005
Cano-Gutiérrez C, Borda MG, Reyes-Ortiz C, Arciniegas AJ, Samper-Ternent R. Assessment of factors associated with functionality in older adults over 60 years in Bogotá, Colombia. Biomédica. 2016;37:57-65. https://doi.org/10.7705/biomedica.v37i1.3197
Laan W, Bleijenberg N, Drubbel I, Numans ME, de Wit NJ, Schuurmans MJ. Factors associated with increasing functional decline in multimorbid independently living older people. Maturitas. 2013;75:276-81. https://doi.org/10.1016/j.maturitas.2013.04.005
Brito KQ, Menezes TN de, Olinda RA de, Brito KQ, Menezes TN de, Olinda RA. Functional disability and socioeconomic and demographic factors in elderly. Rev Bras Enferm. 2015;68:633-41. https://doi.org/10.1590/0034-7167.2015680409i
Dunlop DD, Semanik P, Song J, Manheim LM, Shih V, Chang RW. Risk factors for functional decline in older adults with arthritis. Arthritis Rheum. 2005;52:1274-82. https://doi.org/10.1002/art.20968
Hoogerduijn JG, Buurman BM, Korevaar JC, Grobbee DE, de Rooij SE, Schuurmans MJ. The prediction of functional decline in older hospitalised patients. Age Ageing. 2012;41:381-7. https://doi.org/10.1093/ageing/afs015
Gomes C dos S, Maciel ÁCC, Freire A do NF, Moreira M de A, Ribeiro M De O, Guerra RO. Depressive symptoms and functional decline in an elderly sample of urban center in northeastern Brazil. Arch Gerontol Geriatr. 2014;58:214-8. https://doi.org/10.1016/j.archger.2013.10.009
Landi F, Russo A, Liperoti R, Danese P, Maiorana E, Pahor M, et al. Daily pain and functional decline among old-old adults living in the community: Results from the ilSIRENTE Study. J Pain Symptom Manage. 2009;38:350-7. https://doi.org/10.1016/j.jpainsymman.2008.10.005
Astudillo CI. Depresión como predictor de discapacidad en adultos mayores. Salud UIS. 2007;49:438-49. https://doi.org/10.18273/revsal.v49n3-2017002
Barry LC, Murphy TE, Gill TM. Depressive symptoms and functional transitions over time in older persons. Am J Geriatr Psychiatry. 2011;19:783-91. https://doi.org/10.1097/JGP.0b013e3181ff6669
Liu-Seifert H, Siemers E, Sundell K, Price K, Han B, Selzler K, et al. Cognitive and functional decline and their relationship in patients with mild Alzheimer’s dementia. J Alzheimers Dis. 2014;43:949-55. https://doi.org/10.3233/JAD-140792
Díaz-Venegas C, De La Vega S, Wong R. Transitions in activities of daily living in Mexico, 2001-2012. Salud Pública Mex. 2015;57(Suppl.1):S54-61. https://doi.org/10.21149/spm.v57s1.7590
Díaz-Venegas C, Reistetter TA, Wang C-Y, Wong R. The progression of disability among older adults in Mexico. Disabil Rehabil. 2016;38:2016-27. https://doi.org/10.3109/09638288.2015.1111435
Some similar items:
- Erika Santamaría, Olga Lucía Cabrera, Yaneth Zipa, Cristina Ferro, Martha Liliana Ahumada, Raúl Hernando Pardo, Preliminary evaluation of the Culicoides biting nuisance (Diptera: Ceratopogonidae) in the province of Boyacá, Colombia , Biomedica: Vol. 28 No. 4 (2008)
- Helena Luisa Brochero, Martha L. Quiñones, Challenges of the medical entomology for the surveillance in public health in Colombia: reflections on the state of malaria , Biomedica: Vol. 28 No. 1 (2008)
- Carlos Humberto Torres, Marcela E. Varona, Angélica Lancheros, Rosa Isabel Patiño, Helena Groot, DNA damage assessment and biological monitoring of occupational exposure to organic solvents, 2006 , Biomedica: Vol. 28 No. 1 (2008)
- Juan José Alava, Pedro J. Jiménez, Gnathostoma (Spirurida: Gnathostomatidae) infection in the tigerfish Hoplias microlepis: prevalence, correlation with fish size, hosts, and public health implications , Biomedica: Vol. 29 No. 4 (2009)
- Oscar Fernando Herrán, María F. Ardila, Categories of alcohol consumers and the criteria for classification , Biomedica: Vol. 29 No. 4 (2009)
- Claudia Marcela Castro, Gloria Puerto, Luz Mary García, Dora Leticia Orjuela, Claudia Llerena, María Consuelo Garzón, Wellman Ribón, Molecular Identification of non-tuberculous mycobacteria , Biomedica: Vol. 27 No. 3 (2007)
- Elizabeth Silva, Jaime Eduardo Ortiz, Carmenza Murillo, Gerardo Nava, Omayda Cárdenas, Alejandro Peralta, Marta Paredez, Karina Piñeros, Andrés Otálora, Microbiological and chemical quality of water used in Colombian food industries , Biomedica: Vol. 30 No. 3 (2010)
- Germán A. Díaz-Palacios, Javier H. Eslava-Schmalbach, Perirectal block for out-patient anorectal surgery: A new technique , Biomedica: Vol. 31 No. 2 (2011)
- Jefferson Antonio Buendía, Attitudes, knowledge and beliefs of patient about anti-hypertensive drugs , Biomedica: Vol. 32 No. 4 (2012)
- Silvia Blair, Challenges for the elimination of malaria in Colombia: A problem of knowledge or of power , Biomedica: Vol. 32 (2012): Suplemento 1, Malaria
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























