The effectiveness of serum S100B, TRAIL, and adropin levels in predicting clinical outcome, final infarct core, and stroke subtypes of acute ischemic stroke patients
Abstract
Introduction: More than half of all worldwide deaths and disabilities were caused by stroke. Large artery atherosclerosis is identified as a high etiological risk factor because it accounts for 20% of ischemic stroke.
Objectives: To identify the significance of TRAIL and adropin release and the relative changes related to S100B levels, as well as the relationship between these biomarkers and the final infarct core, the clinical outcome, and the presence of large artery atherosclerosis in acute stroke patients.
Materials and methods: Over a one-year period, demographic, clinical, and neuroimaging findings of 90 consecutive patients with acute ischemic stroke were evaluated.
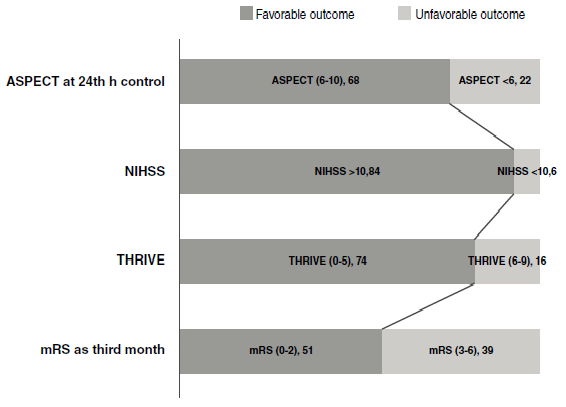
Results: The mean age of participants was 69.28 ± 10 and 39 patients were female. The increased level of S100B and the decreased levels of sTRAIL with adropin were significantly associated with moderate to severe neurologic presentation (p=0.0001, p=0.002, p=0.002, respectively). On the control CT, a large infarct core was significantly associated with decreased serum levels of sTRAIL and adropin (p=0.001 and p=0.000, respectively); however, the levels of S100B were not significantly associated with good ASPECTS score (p=0.684). Disability and an unfavorable outcome were significantly related to the decreased level of sTRAIL and adropin (p=0.001 and p=0.000 for THRIVE score>5, respectively). Decreased sTRAIL and adropin levels and an increased S100B level were correlated with the presence of large artery atherosclerotic etiologic factors (p=0.000, p=0.000, p=0.036, respectively).
Conclusion: TRAIL and adropin serum levels were associated with poor clinical outcomes and greater infarcted area in acute ischemic stroke patients.
Downloads
References
Goldstein LB, Bushnell CD, Adams RJ, Appel LJ, Braun LT, Chaturvedi S, et al. Guidelines for the primary prevention of stroke: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;42:517-84. https://doi.org/10.1161/STR.0000000000000046
Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. 2015 American Heart Association/American Stroke association focused update of the 2013 guidelines for the early management of patients with acute ıschemic stroke regarding endovascular treatment. Stroke. 2015;46:3020-35. https://doi.org/10.1161/STR.0000000000000074
Campbell BCV, De Silva DA, Macleod MR, Coutts SB, Schwamm LH, Davis SM, et al. Ischaemic stroke. Nat Rev Dis Primers. 2019;5:70. https://doi.org/10.1038/s41572-019-0118-8
Hewitt J, Castilla-Guerra L, Fernández-Moreno M del C, Sierra C. Diabetes and stroke prevention: A review. Stroke Res Treat. 2012;673187. https://doi.org/10.1155/2012/673187
Prakash R, Li W, Qu Z, Johnson MA, Fagan SC, Ergul A. Vascularization pattern after ischemic stroke is different in control versus diabetic rats: Relevance to stroke recovery. Stroke. 2013;44:2875-82. https://doi.org/10.1161/STROKEAHA.113.001660
Verma S, Buchanan MR, Anderson TJ. Endothelial function testing as a biomarker of vascular disease. Circulation. 2003;108:2054-9. https://doi.org/10.1161/01.CIR.0000089191.72957.ED
Tisato V, Gonelli A, Voltan R, Secchiero P, Zauli G. Clinical perspectives of TRAIL: Insights into central nervous system disorders. Cell Mol Life Sci. 2016;73:2017-27. https://doi.org/10.1007/s00018-016-2164-7
Secchiero P, Zauli G. TRAIL, a new weapon against neointimal hyperplasia. Cardiology. 2012;123:94-6. https://doi.org/10.1159/000342983
Marczuk N, Cecerska-Heryć E, Jesionowska A, Dołęgowska B. Adropin - physiological and pathophysiological role. Postepy Hig Med Dosw (Online). 2016;70:981-8. https://doi.org/10.5604/17322693.1220082
Wu L, Fang J, Chen L, Zhao Z, Luo Y, Lin C, et al. Low serum adropin is associated with coronary atherosclerosis in type 2 diabetic and non-diabetic patients. Clin Chem Lab Med. 2013;52:751-8. https://doi.org/10.1515/cclm-2013-0844
Weglewski A, Ryglewicz D, Mular A, Juryńczyk J. Changes of protein S100B serum concentration during ischemic and hemorrhagic stroke in relation to the volume of stroke lesion. Neurologia i Neurochirurgia Polska. 2005;39:310-7.
Barber PA, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. Lancet. 2000;355:1670-4. https://doi.org/10.1016/s0140-6736(00)02237-6
Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019-30. https://doi.org/10.1056/NEJMoa1414905
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24:35-41. https://doi.org/10.1161/01.str.24.1.35
Flint AC, Cullen SP, Rao VA, Faigeles BS, Pereira VM, Levy EI, et al. The THRIVE score strongly predicts outcomes in patients treated with the Solitaire device in the SWIFT and STAR trials. Int J Stroke. 2014;9:698-704. https://doi.org/10.1111/ijs.12292
Aydin S. Three new players in energy regulation: Preptin, adropin and irisin. Peptides. 2014;56:94-110. https://doi.org/10.1016/j.peptides.2014.03.021
Dassan P, Keir G, Brown M. Criteria for a clinically informative serum biomarker in acute ischaemic stroke: A review of S100B. Cerebrovasc Dis. 2009;27:295-302. https://doi.org/ 10.1159/000199468
Wunderlich MT, Wallesch CW, Goertler M. Release of neurobiochemical markers of brain damage is related to the neurovascular status on admission and the site of arterial occlusion in acute ischemic stroke. J Neurol Sci. 2004;227:49-53. https://doi.org/10.1016/j.jns.2004.08.005
Park SY, Kim MH, Kim OJ, Ahn HJ, Song JY, Jeong, JY, et al. Plasma heart-type fatty acid binding protein level in acute ischemic stroke: Comparative analysis with plasma S100B level for diagnosis of stroke and prediction of long-term clinical outcome. Clin Neurol Neurosurg. 2013;115:405-10. https://doi.org/10.1016/j.clineuro.2012.06.004
Watt V, Chamberlain J, Steiner T, Francis S, Crossman D. TRAIL attenuates the development of atherosclerosis in apolipoprotein E deficient mice. Atherosclerosis. 2011;215:348-54. https://doi.org/10.1016/j.atherosclerosis.2011.01.010
Tufekci KU, Vurgun U, Yigitaslan O, Keskinoglu P, Yaka E, Kutluk K, et al. Follow-up analysis of serum TNF-related apoptosis-inducing ligand protein and mRNA expression in peripheral blood mononuclear cells from patients with ischemic stroke. Front Neurol. 2018;9:102. https://doi.org/10.3389/fneur.2018.00102
Kang YH, Park MG, Noh KH, Park HR, Lee HW, Son SM, et al. Low serum TNF-related apoptosis-inducing ligand (TRAIL) levels are associated with acute ischemic stroke severity. Atherosclerosis. 2015;240:228-33. https://doi.org/ 10.1016/j.atherosclerosis.2015.03.028
Wu L, Fang J, Chen L, Zhao Z, Luo Y, Lin C, et al. Low serum adropin is associated with coronary atherosclerosis in type 2 diabetic and non-diabetic patients. Clin Chem Lab Med. 2014;52:751-8. https://doi.org/ 10.1515/cclm-2013-0844
Sato K, Yamashita T, Shirai R, Shibata K, Okano T, Yamaguchi M, et al. Adropin contributes to anti-atherosclerosis by suppressing monocyte-endothelial cell adhesion and smooth muscle cell proliferation. Int J Mol Sci. 2018;19:1293. https://doi.org/10.3390/ijms19051293
Li L, Xie W, Zheng XL, Yin WD, Tang CK. A novel peptide adropin in cardiovascular diseases. Clin Chim Acta. 2016;453:107-13. https://doi.org/10.1016/j.cca.2015.12.010
Celik A, Balin M, Kobat K, Erdem MA, Baydas A, Bulut M, et al. Deficiency of a new protein associated with cardiac syndrome X, called adropin. Cardiovasc Ther. 2013;31:174-8. https://doi.org/ 10.1111/1755-5922.12025
Altamimi TR, Gao S, Karwi QG, Fukushima A, Rawat S, Wagg CS, et al. Adropin regulates cardiac energy metabolism and improves cardiac function and efficiency. Metabolism. 2019;98:37-48. https://doi.org/10.1016/j.metabol.2019.06.005
Secchiero P, Corallini F, Ceconi C, Parrinello G, Volpato S, Ferrari R, et al. Potential prognostic significance of decreased serum levels of TRAIL after acute myocardial infarction. PLoS ONE. 2009;4:e4442. https://doi.org/10.1371/journal.pone.0004442
Cartland SP, Genner SW, Martínez GJ, Robertson S, Kockx M, Lin RC, et al. TRAILexpressing monocyte/macrophages are critical for reducing inflammation and atherosclerosis. iScience. 2019;12:41-52. https://doi.org/10.1016/j.isci.2018.12.037
Butler AA, St-Onge MP, Siebert EA, Medici V, Stanhope KL, Havel PJ. Differential responses of plasma adropin concentrations to dietary glucose or fructose consumption in humans. Sci Rep. 2015;5:14691. https://doi.org/10.1038/srep14691
Some similar items:
- Hernán Bayona , María Camila Valencia, Angélica Peña , Natalia Ramírez, Carlos Martínez , Fatal reversible cerebral vasoconstriction syndrome: An unusual presentation of a rare disease , Biomedica: Vol. 41 No. 2 (2021)
- Viviana Alexandra Martínez-Villota , Paulo Francisco Mera-Martínez, José Darío Portillo-Miño, Massive acute ischemic stroke after Bothrops spp. envenomation in southwestern Colombia: Case report and literature review , Biomedica: Vol. 42 No. 1 (2022)
- Catalina Cáceres , Álvaro José Lora , Silvia Juliana Villabona , María Catalina Rocha , Paul Anthony Camacho, Adherence to pharmacological treatment in non-communicable chronic diseases in the Colombian population: Systematic review and meta-analysis , Biomedica: Vol. 43 No. Sp. 3 (2023): Enfermedades crónicas no transmisibles
- Juan Pablo Morales, Stroke in a young adult associated with primary membranous nephropathy: case report. , Biomedica: Vol. 44 No. Sp. 1 (2024): Publicación anticipada, Enfermedades crónicas no transmisibles
Funding data
-
Bezmialem Vakıf Üniversitesi
Grant numbers Decision No: 06.2015/19
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























