Sociodemographic and clinical characteristics of gestational syphilis in Cali, 2018
Abstract
Introduction: Gestational syphilis is considered an event of public health interest given its impact on mother and child. In Colombia, despite having specific protocols for its notification, diagnosis, and management, there are still limitations in its control.
Objectives: To describe the sociodemographic and clinical characteristics, as well as the spatial distribution of gestational syphilis in Cali, Colombia, in 2018.
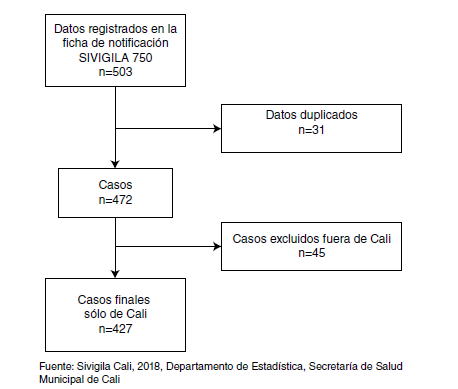
Materials and methods: We conducted a cross-sectional study of 427 gestational syphilis cases reported to the Colombian national epidemiological surveillance system (Sivigila). For the statistical processing, we used the R program, version 3.5.3. We expressed qualitative variables as proportions and quantitative ones through central tendency and dispersion measures, and to establish the spatial distribution we used the Qgis program, version 3.0.
Results: The prevalence of gestational syphilis was 17 cases per 1,000 live births (including stillbirths); 57.1% of patients belonged to the subsidized healthcare system and 16.6% had no health insurance; 90.4% of cases were diagnosed during pregnancy; 47.2% of the pregnant women received three doses of penicillin, yet only 57.6% of contacts were treated.
Conclusions: The prevalence of gestational syphilis in Cali during 2018 exceeded the national rate with a higher frequency among women in socioeconomic vulnerability
conditions consistent with the general spatial distribution. There was a lack of opportunity in the early detection and management of the infection both among pregnant women and their contacts, which hinders the control of the disease and reflects the inadequate application of the comprehensive maternal and perinatal health care route guidelines.
Downloads
References
Cruz-Aconcha AR. Situación de la sífilis gestacional y congénita en Colombia, un desafío al Sistema General de Seguridad Social en Salud. Rev Colomb Obstet Ginecol. 2012;63:304-7. https://doi.org/10.18597/rcog.133
Sabogal AL. Protocolo de vigilancia en salud pública: sífilis gestacional y congénita. Bogotá, D.C.: Instituto Nacional de Salud; 2017. p. 1-17. Fecha de consulta: 12 de febrero de 2020. Disponible en: https://www.ins.gov.co/buscador-eventos/Lineamientos/PRO%20Sifilis_.pdf
Korenromp EL, Rowley J, Alonso M, Mello MB, Wijesooriya NS, Mahiané SG, et al. Global burden of maternal and congenital syphilis and associated adverse birth outcomes—Estimates for 2016 and progress since 2012. PLoS ONE. 2019;14:1-17. https://doi.org/10.1371/journal.pone.0211720
Peeling RW, Hook III EW. The pathogenesis of syphilis: The Great Mimicker, revisited. J Pathol. 2006;208:224-32. https://doi.org/10.1002/path.1903
Carlson JA, Dabiri G, Cribier B, Sell S. The immunopathobiology of syphilis: The manifestations and course of syphilis are determined by the level of delayed-type hypersensitivity. Am J Dermatopathol. 2011;33:433-60. https://doi.org/10.1097/DAD.0b013e3181e8b587
Tsimis ME, Sheffield JS. Update on syphilis and pregnancy. Birth Defects Res. 2017;109:347-52. https://doi.org/10.1002/bdra.23562
De Santis M, De Luca C, Mappa I, Spagnuolo T, Licameli A, Straface G, et al. Syphilis infection during pregnancy: Fetal risks and clinical management. Infect Dis Obstet Gynecol. 2012;2012:1-5. https://doi.org/10.1155/2012/430585
Arnesen L, Martínez G, Mainero L, Serruya S, Durán P. Gestational syphilis and stillbirth in Latin America and the Caribbean. Int J Gynecol Obstet. 2015;128:241-5. https://doi.org/10.1016/j.ijgo.2014.09.017
Workowski KA, Bolan GA, Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Morb Mortal Wkly Rep. 2015;64:1-137.
Castellanos LG, Ghidinelli M, Kurtis H, Mello MB, Pérez F, Ropero AM, et al. ETMI-PLUS: marco para la eliminación de la transmisión maternoinfantil del VIH, la sífilis, la hepatitis y la enfermedad de Chagas. Washington, D.C.: Organización Panamericana de la Salud; 2017.
p. 1-30. Fecha de consulta: 9 de diciembre de 2019. Disponible en: https://www.paho.org/hq/dmdocuments/2017/2017-cha-etmi-plus-marco-vih-hep-chagas.pdf
Sabogal AL. Informe de sífilis gestacional periodo epidemiológico XIII - 2018. Bogotá, D.C.: Instituto Nacional de Salud; 2018. Fecha de consulta: 1 de abril de 2019. Disponible en: https://www.ins.gov.co/buscador-eventos/Informesdeevento/SIF%C3%8DLIS%20GESTACIONAL%20Y%20CONG%C3%89NITA_2018.pdf
Ministerio de Salud y Protección Social. Lineamiento técnico y operativo de la Ruta Integral de Atención en Salud Materno Perinatal. Bogotá, D.C.: Minsalud; 2017.
ONUSIDA. Avanzando hacia las metas 2020: Progreso en América Latina y el Caribe. 2019. Fecha de consulta: 13 de junio de 2021. Disponible en: https://reliefweb.int/sites/reliefweb.int/files/resources/73659-1.pdf
Mora CP, Duque S, Perlaza G, Faride M, Martínez G, Holguín J. Análisis de Situación Integrado de Salud (ASIS) de Santiago de Cali - Año 2017. Cali: Secretaría de Salud Pública Municipal de Cali; 2017. p. 1-134.
Secretaría de Salud Pública Municipal de Cali. Estadísticas Vitales. Cali: Secretaría de Salud Pública Municipal de Cali; 2018. Fecha de consulta: 17 de septiembre de 2019.
Galeano CL, García WD, Congote LM, Vélez MA, Martínez DM. Prevalencia de sífilis gestacional e incidencia de sífilis congénita, Cali, Colombia, 2010. Rev Colomb Obstet Ginecol. 2012;63:321-6. https://doi.org/https://doi.org/10.18597/rcog.136
Agudelo RD, Medina MC, Cardona D. Caracterización de la sífilis congénita y gestacional en Caldas, Colombia. Arch Med (Manizales). 2016;16:326-34. https://doi.org/10.30554/archmed.16.2.1736.2016
Ochoa MT, Gaitán HG, Caicedo S, Gómez B, Pérez F. Introducción de pruebas rápidas para sífilis y VIH en el control prenatal en Colombia: análisis cualitativo. Rev Panam Salud Pública. 2016;40:462-7.
Alonso M, Mello M. Elimination of mother-to-child transmission of HIV and syphilis in the Americas: Update 2016. Washington, D.C.; PAHO: 2017. p. 1-62. Fecha de consulta: 8 de diciembre de 2019. Disponible en: http://iris.paho.org/xmlui/bitstream/handle/123456789/34072/9789275119556-eng.pdf?sequence=4&isAllowed=y
Gramazio L, Zarpellon B, Gramazio L, Baratieri T, Lentsck MH, de Azevedo V. Gestational and congenital syphilis: Maternal, neonatal characteristics and outcome of cases. Rev Bras Saúde Matern Infant. 2017;17:781-9. https://doi.org/10.1590/1806-93042017000400010
Padovani C, Rosseto de Oliveira R, Pelloso SM. Syphilis during pregnancy: Association of maternal and perinatal characteristics in a region of southern Brazil. Rev Latino-Am Enfermagem. 2018;26:1-10. https://doi.org/10.1590/1518-8345.2305.3019
Amador C, Lavalle MH, Chamorro MV. Sífilis gestacional: enfermedad de interés en salud pública, Córdoba-Colombia, 2015. Rev Cuid. 2017;8:1449-58. https://doi.org/10.15649/cuidarte.v8i1.350
Silva AM, Bois F, Duro E. Factores asociados con falla en el diagnóstico y tratamiento de sífilis materna. Medicina Infantil. 2016;XXIII:293-8.
Panosso de Freitas E, Dell Agnolo CM, Borges L, Pelloso SM, Bercini LO, Harumi I. Percepção de adolescentes sobre a prática sexual na adolescência. Revista de Psicologia da Criança e do Adolescente. 2014;5:139-49.
Escobar G, Perilla DM. Cali en cifras 2018-2019. Cali: Departamento Administrativo de Planeación, Alcaldía de Santiago de Cali; 2019.
Páez GN, Jaramillo LF, Franco C, Arregoces L, Bardey D, Ortiz JL, et al. Estudio sobre el modo de gestionar la salud en Colombia. Bogotá, D.C.: Ministerio de Salud y Protección Social; 2015. Fecha de consulta: 5 de noviembre de 2019. Disponible en: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/AS/gestionar%20la%20salud%20en%20Colombia.pdf
Garcés JP, Rubiano LC, Orobio Y, Castaño M, Benavides E, Cruz A. La educación del personal de salud: clave para la eliminación de la sífilis congénita en Colombia. Biomédica. 2017;37:416-24. https://doi.org/10.7705/biomedica.v37i3.3397
Some similar items:
- Mónica Marcela Jiménez, Jesús Arias, Gabriel Carrasquilla, Seroprevalence of dengue infection in the municipalities of Armenia, Calarcá, La Tebaida and Montenegro in Quindío, 2014 , Biomedica: Vol. 37 No. 1 (2017)
- Jorge Arturo Martínez, Walter Amaya, Horacio Alfredo Campillo, Adalberto Campo, Luis Alfonso Díaz, Social factors associated with the daily cigarette smoking among middle-school student adolescents in Bucaramanga, Colombia. , Biomedica: Vol. 25 No. 4 (2005)
- Erika Santamaría, Olga Lucía Cabrera, Yaneth Zipa, Cristina Ferro, Martha Liliana Ahumada, Raúl Hernando Pardo, Preliminary evaluation of the Culicoides biting nuisance (Diptera: Ceratopogonidae) in the province of Boyacá, Colombia , Biomedica: Vol. 28 No. 4 (2008)
- Ligia Inés Moncada, Sandra Milena Rios, Julián Alfredo Fernández, Fabio Rivas, María Luz Sáenz, Pediculosis prevalence and associated risk factors in a nursery school, Bogotá, Colombia , Biomedica: Vol. 28 No. 2 (2008)
- Helena Luisa Brochero, Martha L. Quiñones, Challenges of the medical entomology for the surveillance in public health in Colombia: reflections on the state of malaria , Biomedica: Vol. 28 No. 1 (2008)
- Carlos Humberto Torres, Marcela E. Varona, Angélica Lancheros, Rosa Isabel Patiño, Helena Groot, DNA damage assessment and biological monitoring of occupational exposure to organic solvents, 2006 , Biomedica: Vol. 28 No. 1 (2008)
- Guillermo Mora, María Clara Echeverry, Gustavo Enrique Rey, Myriam Consuelo López, Luisa Fernanda Posada, Fabio Aurelio Rivas, Frequency of Trypanosoma cruzi infection in patients with implanted pacemaker , Biomedica: Vol. 27 No. 4 (2007)
- Juan José Alava, Pedro J. Jiménez, Gnathostoma (Spirurida: Gnathostomatidae) infection in the tigerfish Hoplias microlepis: prevalence, correlation with fish size, hosts, and public health implications , Biomedica: Vol. 29 No. 4 (2009)
- Adriana Valdelamar , Fernando De La Hoz , Ricardo Sánchez , Loneliness as a predictor of mortality in cancer patients. A cohort study. Soledad y mortalidad en cáncer , Biomedica: Vol. 44 No. Sp. 1 (2024): Publicación anticipada, Enfermedades crónicas no transmisibles
- Francisca Monsalve, Leonor Chacín Bonilla, Ricardo José Atencio, Leticia Denys Porto, Luciana Ana Costa León, Jesús Enrique Estévez, Diana Estela Callejas Valero, Low prevalence of hepatitis C virus infection in a prisoner population from Maracaibo, Venezuela , Biomedica: Vol. 29 No. 4 (2009)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























