Hyperthyroidism in children and adolescents: Experience in a university hospital in Colombia
Abstract
Introduction: Hyperthyroidism is a heterogeneous condition characterized by the excessive production of thyroid hormones. It represents a diagnostic and therapeutic challenge.
Objective: To describe the clinical and paraclinical characteristics and the evolution and differences between the main etiologies in patients with hyperthyroidism treated by the Pediatric Endocrinology Service at the Hospital Universitario San Vicente Fundación in Medellín, Colombia, between July 1st., 2015, and June 30th., 2020.
Materials and methods: We conducted a cross-sectional observational study with retrospective data collection.
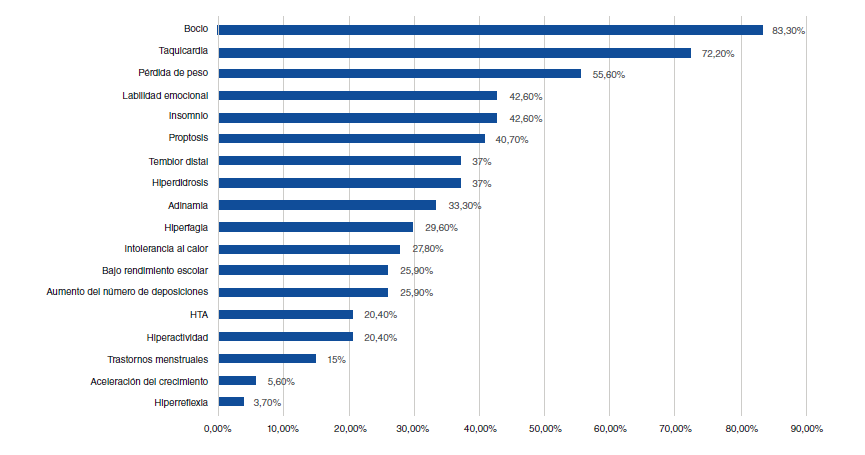
Results: We included 54 patients with a mean age of 11.9 years, 72.2% of whom were female; 85.2% had no history of comorbidities related to autoimmunity; 11.1% had a family history of Graves’ disease, and 29.6% of other thyroid diseases. Goiter was the most frequent clinical manifestation (83.3%) and 92.6% of the patients received treatment with methimazole, 79.6% required beta-blockers, and 11.2% additional drug therapy. Adverse drug reactions occurred in 16.7% of the patients and in 20.4% there was a resolution of hyperthyroidism (spontaneous: 9.3%; after radio-iodine ablation: 9.3%, and after surgery: 1.9%).
Conclusion: Hyperthyroidism is a disease with diverse clinical manifestations. Its most frequent cause is Graves’ disease followed by hashitoxicosis, which in this study had a higher frequency than that reported in the literature. The duration and side effects of pharmacological treatment were similar to those previously reported, but the higher frequency of agranulocytosis is noteworthy.
Downloads
References
Léger J, Carel JC. Hyperthyroidism in childhood: Causes, when and how to treat. J Clin Res Pediatr Endocrinol. 2013;5(Suppl.1):50-6. https://doi.org/10.4274/jcrpe.854
Mokhashi MH, Desai U, Desai MP. Hyperthyroidism in children. Indian J Pediatr. 2000;67:653-6. https://doi.org/10.1007/BF02762177
Srinivasan S. Hyperthyroidism in children. Pediatr Rev. 2015;36:239-48. https://doi.org/10.1542/pir.36-6-239
Marino M, Vitti P, Chiovato L. Graves’ disease. En: Jameson JL, De Groot LJ, de Kretser DM, Giudice LC, Grossman AB, Melmed S, et al., editors. Endocrinology: adult and pediatric. Seventh edition. Philadelphia: Saunders; 2015. p. 1437-64.e8 p. https://doi.org/10.1016/B978-0-323-18907-1.00082-2
Hanley P, Lord K, Bauer AJ. Thyroid disorders in children and adolescents: A review. JAMA Pediatr. 2016;170:1008-19. https://doi.org/10.1001/jamapediatrics.2016.0486
Alvira J, Galván G, Ordóñez J. Eficacia y seguridad del metimazol en el tratamiento del hipertiroidismo por enfermedad de Graves en menores de 18 años: Barranquilla, 2013-2015. Biociencias. 2016;11:41-7.
Laboratory Corporation of America. Expected Values & S.I. Unit Conversion Tables. Esoterix. 2017. Fecha de consulta: 2 de junio de 2022. Disponible en: https://specialtytesting.labcorp.com/sites/default/files/2021-07/L5167-0421-18%20Endocrine%20Expected%20Values_0.pdf
Godoy CC, Acevedo MM, Barrera NA, Yismeyián MA, Ugarte PF. Hipertiroidismo en niños y adolescentes. Rev Chil Pediatr. 2009;80:21-9. https://doi.org/10.4067/S0370-41062009000100003
Simon M, Rigou A, Le Moal J, Zeghnoun A, Le Tertre A, De Crouy-Chanel P, et al. Epidemiology of childhood hyperthyroidism in France: A nationwide population-based study. J Clin Endocrinol Metab. 2018;103:2980-7. https://doi.org/10.1210/jc.2018-00273
Léger J, Oliver I, Rodrigue D, Lambert AS, Coutant R. Graves’ disease in children. Ann Endocrinol (Paris). 2018;79:647-55. https://doi.org/10.1016/j.ando.2018.08.001
Kyritsi EM, Kanaka-Gantenbein C. Autoimmune thyroid disease in specific genetic syndromes in childhood and adolescence. Front Endocrinol (Lausanne). 2020;11:543. https://doi.org/10.3389/fendo.2020.00543
Rodanaki M, Lodefalk M, Forssell K, Arvidsson CG, Forssberg M, Åman J. The incidence of childhood thyrotoxicosis is increasing in both girls and boys in Sweden. Horm Res Paediatr. 2019;91:195-202. https://doi.org/10.1159/000500265
Havgaard Kjær R, Smedegård Andersen M, Hansen D. Increasing incidence of juvenile thyrotoxicosis in Denmark: A nationwide study, 1998-2012. Horm Res Paediatr. 2015;84:102-7. https://doi.org/10.1159/000430985
Zanolli M, Araya A, Cattani A, Orellana P, Martínez-Aguayo A. Enfermedad de Basedow Graves en pacientes pediátricos. Rev Chil Pediatr. 2008;79:26-35. https://doi.org/10.4067/S0370-41062008000100004
Williamson S, Greene SA. Incidence of thyrotoxicosis in childhood: A national population based study in the UK and Ireland. Clin Endocrinol (Oxf). 2010;72:358-63. https://doi.org/10.1111/j.1365-2265.2009.03717.x
Tunç S, Köprülü Ö, Ortaç H, Nalbantoğlu Ö, Dizdarer C, Demir K, et al. Long-term monitoring of Graves’ disease in children and adolescents: A single-center experience. Turkish J Med Sci. 2019;49:464-71. https://doi.org/10.3906/sag-1804-177
Kourime M, McGowan S, Al Towati M, Ahmed SF, Stewart G, Williamson S, et al. Long-term outcome of thyrotoxicosis in childhood and adolescence in the west of Scotland: The case for long-term antithyroid treatment and the importance of initial counselling. Arch Dis Child. 2018;103:637-42. https://doi.org/10.1136/archdischild-2017-313454
Okawa ER, Grant FD, Smith JR. Pediatric Graves’ disease: Decisions regarding therapy. Curr Opin Pediatr. 2015;27:442-7. https://doi.org/10.1097/MOP.0000000000000241
Sims EK, Eugster EA, Nebesio TD. Detours on the road to diagnosis of graves disease. Clin Pediatr (Phila). 2012;51:160-4. https://doi.org/10.1177/0009922811418823
Goldstein SM, Katowitz WR, Moshang T, Katowitz JA. Pediatric thyroid-associated orbitopathy: The children’s hospital of philadelphia experience and literature review. Thyroid. 2008;18:997-9. https://doi.org/10.1089/thy.2008.0014
Ladd JM, Sabsabi B, von Oettingen JE. Thyroid storm in a toddler presenting as a febrile seizure. Pediatrics. 2020;145:e20191920. https://doi.org/10.1542/peds.2019-1920
Esen İ, Bayramoğlu E, Yildiz M, Aydin M, Özturhan EK, Aycan Z, et al. Management of thyrotoxicosis in children and adolescents: A Turkish multi-center experience. J Clin Res Pediatr Endocrinol. 2019;11:164-72. https://doi.org/10.4274/jcrpe.galenos.2018.2018.0210
Yap PS, Ali O, Truran P, Aspinall S. Thyrotoxicosis and thyroiditis. Surgery. 2020;38:794-800. https://doi.org/10.1016/j.mpsur.2020.10.002
Léger J, Carel JC. Diagnosis and management of hyperthyroidism from prenatal life to adolescence. Best Pract Res Clin Endocrinol Metab. 2018;32:373-86. https://doi.org/10.1016/j.beem.2018.03.014
Fröhlich E, Wahl R. Thyroid autoimmunity: Role of anti-thyroid antibodies in thyroid and extrathyroidal diseases. Front Immunol. 2017;8:521. https://doi.org/10.3389/fimmu.2017.00521
Comité Nacional de Endocrinología. Alteraciones tiroideas en la infancia y en la adolescencia. Parte 2: hipotiroidismo. Arch Argent Pediatr. 2021;119:S8-16.
Malik SA. Comparison between peak systolic velocity of the inferior thyroid artery and technetium-99m pertechnetate thyroid uptake in differentiating Graves’ disease from thyroiditis. Arch Endocrinol Metab. 2019;63:495-500. https://doi.org/10.20945/2359-3997000000165
Perdomo CM, García-Goñi M, Sancho L, JJ Paricio, Lozano MD, de la Higuera M, et al. Evaluation of the role of thyroid scintigraphy in the differential diagnosis of thyrotoxicosis. Clin Endocrinol (Oxf). 2021;94:466-72. https://doi.org/10.1111/cen.14308
Marques O, Antunes A, Oliveira MJ. Treatment of Graves’ disease in children: The Portuguese experience. Endocrinol Diabetes y Nutr. 2018;65:143-9. https://doi.org/10.1016/j.endinu.2017.11.014
Azizi F, Takyar M, Madreseh E, Amouzegar A. Long-term methimazole therapy in Juvenile Graves’ Disease: A randomized trial. Pediatrics. 2019;143:e20183034. https://doi.org/10.1542/peds.2018-3034
Rivkees SA, Stephenson K, Dinauer C. Adverse events associated with methimazole therapy of Graves’ disease in children. Int J Pediatr Endocrinol. 2010;2010:1-4. https://doi.org/10.1155/2010/176970
Ohye H, Minagawa A, Noh JY, Mukasa K, Kunii Y, Watanabe N, et al. Antithyroid drug treatment for Graves’ disease in children: A long-term retrospective study at a single institution. Thyroid. 2014;24:200-7. https://doi.org/10.1089/thy.2012.0612
Yasuda K, Miyoshi Y, Tachibana M, Namba N, Miki K, Nakata Y, et al. Relationship between dose of antithyroid drugs and adverse events in pediatric patients with graves’ disease. Clin Pediatr Endocrinol. 2017;26:1-7. https://doi.org/10.1297/cpe.26.1
Léger J, Gelwane G, Kaguelidou F, Benmerad M, Alberti C, Coutant R, et al. Positive impact of long-term antithyroid drug treatment on the outcome of children with Graves’ disease: National long-term cohort study. J Clin Endocrinol Metab. 2012;97:110-9. https://doi.org/10.1210/jc.2011-1944
Léger J, Oliver I, Rodrigue D, Lambert AS, Coutant R. Graves’ disease in children. Ann Endocrinol (Paris). 2018;79:647-55. https://doi.org/10.1016/j.ando.2018.08.001
De Luca F, Valenzise M. Controversies in the pharmacological treatment of Graves’ disease in children. Expert Rev Clin Pharmacol. 2018;11:1113-21. https://doi.org/10.1080/17512433.2018.1546576
Some similar items:
- Nelsy Loango, Martha Lucía Gallego, Beatriz Restrepo, Patricia Landázuri, Gender, age and plasma lipids differences associated with apolipoprotein E polymorphism in school children , Biomedica: Vol. 29 No. 3 (2009)
- Dr., Diana Benavides-Arias, Luz Amparo Pérez, Jennifer Ruiz, Deidamia García, Iván Osejo, Edwin Ussa, Camilo Pino, Fernando Pío de La Hoz, Incidence of acute respiratory symptoms and COVID-19 infection in children in public schools in Bogotá, Colombia, from July to November, 2020 , Biomedica: Vol. 42 No. Sp. 2 (2022): Covid-19
- José Guillermo Ortega-Ávila, Mildrey Mosquera, Isabella Echeverry-Jiménez, Lorena Jiménez-Bastidas, Milton Fabián Suárez-Ortegón, Alberto Pradilla, Luis Eduardo Bravo, Cecilia Aguilar-de Plata, Early atherosclerotic lesions and post-mortem serum cholesterol level in a group of Colombian children , Biomedica: Vol. 33 No. 3 (2013)
- Andrés Leonardo González, Ruth Aralí Martínez, Luis Ángel Villar, Clinical evolution of dengue in hospitalized patients , Biomedica: Vol. 28 No. 4 (2008)
- Sandra Piñeros-Ortiz, Jaime Moreno-Chaparro, Nathaly Garzón-Orjuela, Zulma Urrego-Mendoza, Daniel Samacá-Samacá, Javier Eslava-Schmalbach, Mental health consequences of armed conflicts in children and adolescents: An overview of literature reviews , Biomedica: Vol. 41 No. 3 (2021)
- Ana Lucía Lópe, Juan David Vélez , Angélica María García , Elkin Fernando Arango, Concurrent validity of five prediction equations to evaluate fat percentage in a sports group expected to yield high performance from Medellín, Colombia , Biomedica: Vol. 41 No. 1 (2021)
- Ana Cecilia Aguilar, Alberto Pradilla, Mildrey Mosquera, Ana Beatriz Gracia, José Guillermo Ortega, Jaime Humberto Leiva, Robinson Ramírez-Vélez, Percentile values for physical condition for Cali, Colombian children and adolescents , Biomedica: Vol. 31 No. 2 (2011)
- Elpidia Poveda, Ney E. Callas, César M. Baracaldo, Carlina Castillo, Patricia Hernández, Leptin levels in school age children associated with anthropometric measurements and lipid profiles , Biomedica: Vol. 27 No. 4 (2007)
- Elpidia Poveda, Ney Callas, César Baracaldo, Carlina Castillo, Patricia Hernández, Martha Guerra, Lipid and apoprotein A-I and B-100 levels in school children school from five central-eastern provinces of Colombia , Biomedica: Vol. 27 No. 3 (2007)
- Ney Callas, Elpidia Poveda, César Baracaldo, Patricia Hernández, Carlina Castillo, Martha Guerra, Genetic polymorphism of the E apolipoprotein in school age children: comparison with levels of plasma lipids and apolipoproteins , Biomedica: Vol. 27 No. 4 (2007)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























