In vitro sensitivity of Malassezia furfur isolates from HIV-positive and negative patients to antifungal agents
Abstract
Introduction. Malassezia is a lipophilic and lipid-dependent yeast genus belonging to the skin microbiota of humans and other animals. However, due to dysbiosis processes or other factors in the host, this yeast can cause different pathologies, ranging from skin diseases, such as seborrheic dermatitis, to fungemia. Isolation of Malassezia furfur has been reported in HIV-positive patients with or without skin lesions. Due to its opportunistic nature and its variable resistance to antifungal compounds, it is relevant to know the Malassezia sensitivity profiles.
Objective. To determine the sensitivity to different antifungal agents, of clinical isolates of M. furfur obtained from HIV-positive or negative patients, with or without seborrheic dermatitis.
Materials and methods. Assessment of isolates sensitivity to itraconazole, voriconazole, fluconazole, and amphotericin B was performed by two techniques: (1) Broth microdilution using Clinical and Laboratory Standards Institute (CLSI) protocol M27-A3 with modifications; and (2) agar tests using Etest®.
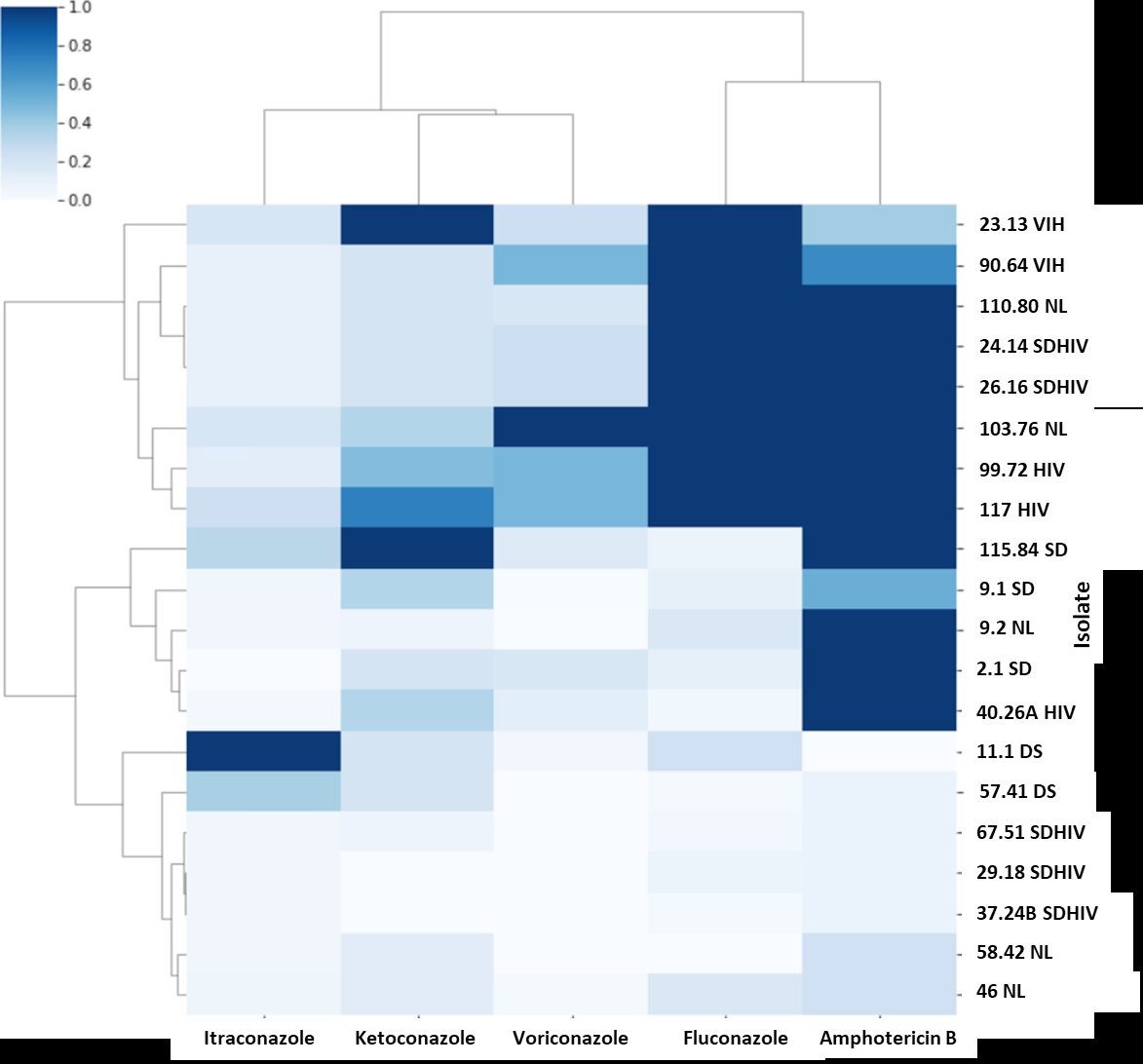
Results. Isolates obtained from HIV patients showed an increase in the minimum inhibitory concentration of fluconazole, voriconazole, and amphotericin B, compared with those of non-HIV patients. Itraconazole was the antifungal with the lowest minimum inhibitory concentration (MIC) in most isolates.
Conclusion. We observed differences in the sensitivity profiles of M. furfur isolates according to the context of the patient. High MIC of antifungals like fluconazole, commonly used for treating pathologies caused by Malassezia, were identified.
Downloads
References
Gaitanis G, Magiatis P, Hantschke M, Bassukas ID, Velegraki A. The Malassezia genus in skin and systemic diseases. Clin Microbiol Rev. 2012;25:106-41. https://doi.org/10.1128/CMR.00021-11
Velegraki A, Cafarchia C, Gaitanis G, Iatta R, Boekhout T. Malassezia infections in humans and animals: Pathophysiology, detection, and treatment. PLoS Pathog. 2015;11:e1004523. https://doi.org/10.1371/journal.ppat.1004523
Lorch JM, Palmer JM, Vanderwolf KJ, Schmidt KZ, Verant ML, Weller TJ, et al. Malassezia espertilionis sp. Nov.: A new cold-tolerant species of yeast isolated from bats. Persoonia. 018;41:56-70. https://doi.org/10.3767/persoonia.2018.41.04
Saheb-Kashaf S, Proctor DM, Deming C, Saary P, Hölzer M, Taylor ME, et al. Integrating ultivation and metagenomics for a multi-kingdom view of skin microbiome diversity and unctions. Nat Microbiol. 2022;7:169-79. https://doi.org/10.1038/s41564-021-01011-w
Jo JH, Deming C, Kennedy EA, Conlan S, Polley EC, Ng Wl, et al. Diverse human skin ungal communities in children converge in adulthood. J Invest Dermatol. 2016;136:2356-63. htts://doi.org/10.1016/j.jid.2016.05.130
Rhimi W, Theelen B, Boekhout T, Otranto D, Cafarchia C. Malassezia spp. yeasts of emerging concern in fungemia. Front Cell Infect Microbiol. 2020;10:370. https://doi.org/10.3389/fcimb.2020.00370
Saunte DML, Gaitanis G, Hay RJ. Malassezia-associated skin diseases, the use of diagnostics and treatment. Front Cell Infect Microbiol. 2020;10:112. https://doi.org/10.3389/fcimb.2020.00112
Limon JJ, Tang J, Li D, Wolf AJ, Michelsen KS, Funari V, et al. Malassezia is associated with Crohn’s disease and exacerbates colitis in mouse models. Cell Host Microbe. 2019;25:377-88. https://doi.org/10.1016/j.chom.2019.01.007
Aykut B, Pushalkar S, Chen R, Li Q, Abengozar R, Kim JI, et al. The fungal mycobiome promotes pancreatic oncogenesis via activation of MBL. Nature. 2019;574:264-7. https://doi.org/10.1038/s41586-019-1608-2
Pedrosa AF, Lisboa C, Branco J, Pellevoisin C, Miranda IM, Rodrigues AG. Malassezia interaction with a reconstructed human epidermis: Keratinocyte immune response. Mycoses. 2019;62:932-6. https://doi.org/10.1111/myc.12965
Sastoque A, Triana S, Ehemann K, Suárez L, Restrepo S, Wösten H, et al. New therapeutic candidates for the treatment of Malassezia pachydermatis-associated infections. Sci Rep. 2020;10:1-12. https://doi.org/10.1038/s41598-020-61729-1
Rhimi W, Theelen B, Boekhout T, Aneke CI, Otranto D, Cafarchia C. Conventional therapy and new antifungal drugs against Malassezia infections. Med Mycol. 2021;59:215-34. https://doi.org/10.1093/mmy/myaa087
Wang K, Cheng L, Li W, Jiang H, Zhang X, Liu S, et al. Susceptibilities of Malassezia strains from pityriasis versicolor, Malassezia folliculitis and seborrheic dermatitis to antifungal drugs. Heliyon. 2020;6:e04203. https://doi.org/10.1016/j.heliyon.2020.e04203
Ehemann K, Mantilla MJ, Mora-Restrepo F, Ríos-Navarro A, Torres, M, Celis-Ramírez AM. Many ways, one microorganism: Several approaches to study Malassezia in interactions with model hosts. PLoS Pathog. 2022;18:e1010784. https://doi.org/10.1371/journal.ppat.1010784
Galvis-Marín JC, Rodríguez-Bocanegra MX, Pulido-Villamarín A del P, Castañeda-Salazar R, Celis-Ramírez AM, Linares-Linares MY. Actividad antifúngica in vitro de azoles y anfotericina B frente a Malassezia furfur por el método de microdilución M27-A3 del CLSI y Etest®®. Rev Iberoam Micol. 2017;34:89-93. https://doi.org/10.1016/j.riam.2016.05.004
Park M, Cho YJ, Lee YW, Jung WH. Genomic multiplication and drug efflux influence ketoconazole resistance in Malassezia restricta. Front Cell Infect Microbiol. 2020;10:191. https://doi.org/10.3389/fcimb.2020.00191
Kim M, Cho YJ, Park M, Choi Y, Hwang SY, Jung WH. Genomic tandem quadruplication is associated with ketoconazole resistance in Malassezia pachydermatis. J Microbiol Biotechnol. 2018;28:1937-45. https://doi.org/10.4014/jmb.1810.10019
Leong C, Kit JCW, Lee SM, Lam YI, Goh JPZ, Ianiri G, et al. Azole resistance mechanisms in pathogenic M. furfur. Antimicrob Agents Chemother. 2021;65:e01975-20. https://doi.org/10.1128/AAC.01975-20
Huang CY, Peng CC, Hsu CH, Chang JH, Chiu NC, Chi H. Systemic infection caused by Malassezia pachydermatis in infants: Case series and review of the literature. Pediatr Infect Dis J. 2020;39:444-8. https://doi.org/10.1097/INF.0000000000002591
Chen IT, Chen CC, Huang HC, Kuo KC. Malassezia furfur emergence and candidemia trends in a neonatal intensive care unit during 10 years: the experience of fluconazole prophylaxis in a single hospital. Adv Neonatal Care. 2020;20:e3-8. https://doi.org/10.1097/ANC.0000000000000640
Galvis-Marín JC, Giraldo-Ospina B, Martínez-Ríos JB, EcheverriPeláez S. Fungemia por Malassezia sympodialis en una unidad de cuidados intensivos neonatal de Colombia. Infectio. 2021;25:130-4. https://doi.org/10.22354/in.v25i2.931
Pedrosa AF, Lisboa C, Rodrigues AG. Malassezia infections with systemic involvement: Figures and facts. J Dermatol. 2018;45:1278-82. https://doi.org/10.1111/1346-8138.14653
Chen SCA, Perfect J, Colombo AL, Cornely OA, Groll AH, Seidel D, et al. Global guideline for the diagnosis and management of rare yeast infections: An initiative of the ECMM in cooperation with ISHAM and ASM. Lancet Infect Dis. 2021;21:375-86. https://doi.org/10.1016/s1473-3099(21)00203-6
Moreno-Coutiño G, Sánchez-Cárdenas CD, Arroyo-Escalante S, Arenas R. Isolation of Malassezia spp. in HIV-positive patients with and without seborrheic dermatitis. An Bras Dermatol. 2019;94:527-31. https://doi.org/10.1016/j.abd.2019.09.012
Krzyściak P, Bakuła Z, Gniadek A, Garlicki A, Tarnowski M, Wichowski M, et al. Prevalence of Malassezia species on the skin of HIVseropositive patients. Sci Rep. 2020;10:1-13. https://doi.org/10.1038/s41598-020-74133-6
Amado Y, Patiño-Uzcátegui A, Cepero De García MC, Tabima J, Motta A, Cárdenas M, et al. Seborrheic dermatitis: Predisposing factors and ITS2 secondary structure for Malassezia phylogenic analysis. Med Mycol. 2013;51:86875. https://doi.org/10.3109/13693786.2013.820001
Cafarchia C, Iatta R, Immediato D, Puttilli MR, Otranto D. Azole susceptibility of Malassezia pachydermatis and Malassezia furfur and tentative epidemiological cut-off values. Med Mycology. 2015;53:743-8. https://doi.org/10.1093/mmy/myv049
Cafarchia C, Figueredo LA, Iatta R, Colao V, Montagna MT, Otranto D. In vitro evaluation of Malassezia pachydermatis susceptibility to azole compounds using Etest® and CLSI microdilution methods. Med Mycol. 2012;87:795801. https://doi.org/10.3109/13693786.2012.674219
Álvarez-Pérez S, Blanco JL, Peláez T, Cutuli M, García ME. In vitro amphotericin B susceptibility of Malassezia pachydermatis determined by the CLSI broth microdilution method and etest using lipid-enriched media. Antimicrob Agents Chemother. 2014;58:4203-6. https://doi.org/10.1128/aac.00091-14
Rhimi W, Aneke CI, Mosca A, Otranto D, Cafarchia C. In vitro azole and amphotericin B susceptibilities of Malassezia furfur from bloodstream infections using e-test and CLSI broth microdilution methods. Antibiotics (Basel). 2020;9:361. https://doi.org/10.3390/antibiotics9060361
Rojas FD, Sosa MDLA, Fernández MS, Cattana ME, Córdoba SB, Giusiano GE. Antifungal susceptibility of Malassezia furfur, Malassezia sympodialis, and Malassezia globosa to azole drugs and amphotericin B evaluated using a broth microdilution method. Med Mycol. 2014;52:641-6. https://doi.org/10.1093/mmy/myu010
Pedrosa AF, Carmen L, Faria-Ramos I, Silva R, Ricardo E, Teixeira-Santos R, et al. Epidemiology and susceptibility profile to classic antifungals and over-the-counter products of Malassezia clinical isolates from a Portuguese University Hospital: A prospective study. J Med Microbiol. 2019;68:77884. https://doi.org/10.1099/jmm.0.000966
Iatta R, Figueredo LA, Montagna MT, Otranto D, Cafarchia C. In vitro antifungal susceptibility of Malassezia furfur from bloodstream infections. J Med Microbiol. 2014;63:1467-73. https://doi.org/10.1099/jmm.0.078709-0
Clinical and Laboratory Standards Institute. Reference method for broth dilution antifungal susceptibility testing of yeasts. 3rd edition. Wayne, PA: Clinical and Laboratory Standards Institute; 2008.
Patel JB, Sharp S, Novak-Weekley S. Verification of antimicrobial susceptibility testing methods: A practical approach. Clin Microbiol Newsl. 2013;35:103-9. https://doi.org/10.1016/j.clinmicnews.2013.06.001
Iatta R, Immediato D, Montagna MT, Otranto D, Cafarchia C. In vitro activity of two amphotericin B formulations against Malassezia furfur strains recovered from patients with bloodstream infections. Med Mycol. 2015;53:269-74. https://doi.org/10.1093/mmy/my089
Ford N, Meintjes G, Calmy A, Bygrave H, Migone C, Vitoria M, et al. Managing advanced HIV disease in a public health approach. Clin Infect Dis. 2018;66:106-10. https://doi.org/10.1093/cid/cix1139
Velegraki A, Alexopoulos EC, Kritikou S, Gaitanis G. Use of fatty acid RPMI 1640 media for testing susceptibilities of eight Malassezia species to the new triazoosaconazoleole and to six established antifungal agents by a modified NCCLS M27-A2 microdilution method and Etest®. J Clin Microbiol. 2004;42:3589-93. https://doi.org/10.1128/jcm.42.8.3589-3593.2004
Rojas FD, Córdoba SB, Sosa MDLA, Zalazar LC, Fernández MS, Cattana ME, et al. Antifungal susceptibility testing of Malassezia yeast: comparison of two different methodologies. Mycoses. 2017;60:104-11. https://doi.org/10.1111/myc.12556
Ramesh N, Priyadharsini M, Sumathi CS, Balasubramanian V, Hemapriya J, Kannan R. Virulence factors and antifungal sensitivity pattern of Candida sp. isolated from HIV and TB patients. Indian J Microbiol. 2011;51:273-8. https://doi.org/10.1007/s12088-011-0177-3
Law D, Moore CB, Wardle HM, Ganguli LA, Keaney MGL, Denning DW. High prevalence of antifungal resistance in Candida spp. from patients with AIDS. J Antimicrob Chemother. 1994;34:659-68. https://doi.org/10.1093/jac/34.5.659
Osaigbovo II, Lofor PV, Oladele RO. Fluconazole resistance among oral Candida isolates from people living with HIV/AIDS in a Nigerian tertiary hospital. J Fungi (Basel). 2017;3:69. https://doi.org/10.3390/jof3040069
Some similar items:
- Sandra Rincón, Adriana Celis, Leticia Sopó, Adriana Motta, María Caridad Cepero de García, Malassezia yeast species isolated from patients with dermatologic lesions. , Biomedica: Vol. 25 No. 2 (2005)
- Adriana M. Celis, María Caridad Cepero de García, Genetic polymorphism of Malassezia spp. yeast isolates from individuals with and without dermatological lesions. , Biomedica: Vol. 25 No. 4 (2005)
- Mauricio Beltrán, María Cristina Navas, María Patricia Arbeláez, Jorge Donado, Sergio Jaramillo, Fernando De la Hoz, Cecilia Estrada, Lucía del Pilar Cortés, Amalia de Maldonado, Gloria Rey, Seroprevalence of hepatitis B virus and human immunodeficiency virus infection in a population of multiply-transfused patients in Colombia , Biomedica: Vol. 29 No. 2 (2009)
- María Patricia Arbeláez, Alexánder Arbeláez, Rubén Darío Gómez, Carlos Rojas, Lázaro Vélez, Sonia Luz Arias, Jorge Nagles, Luz Marina Peláez, Gloria Betancourt, Gloria Velásquez, Effectiveness of prophylaxis against tuberculosis in patients infected with HIV , Biomedica: Vol. 27 No. 4 (2007)
- Marcela López, Claudia Álvarez, Utility of nitrate reductase assay for detection of multidrug-resistant Mycobacterium tuberculosis in a low resource setting , Biomedica: Vol. 31 No. 2 (2011)
- María Teresa Rugeles, Paula A. Velilla, Carlos J. Montoya, Mechanisms of human natural resistance to HIV: A summary of ten years of research in the Colombian population , Biomedica: Vol. 31 No. 2 (2011)
- Carmelo José Espinosa, Jorge Alberto Cortés, Juan Sebastián Castillo, Aura Lucía Leal, Systematic review of antimicrobial resistance among Gram positive cocci in hospitals in Colombia , Biomedica: Vol. 31 No. 1 (2011)
- Jaiberth Cardona-Arias, Luz Peláez-Vanegas, Juan López-Saldarriaga, Marcela Duque-Molina, Oscar Leal-Álvarez, Health related quality of life in adults with HIV/AIDS in Colombia , Biomedica: Vol. 31 No. 4 (2011)
- Zulbey Rivero-Rodríguez, Amparo Hernández, Ángela Bracho, Solneumar Salazar, Rafael Villalobos, Prevalence of intestinal microsporidia and other intestinal parasites in HIV positive patients of Maracaibo, Venezuela , Biomedica: Vol. 33 No. 4 (2013)
- Alfredo Prado, Nhora L. Arias, Mónica Chávez, Cristina E. Cabrera, Rómel F. Gómez, Phenotypic characterization of Acinetobacter baumannii isolates in a high-complexity healthcare institution in the city of Cali , Biomedica: Vol. 34 (2014): Abril, Suplemento 1, Resistencia bacteriana
Copyright (c) 2023 Biomedica

This work is licensed under a Creative Commons Attribution 4.0 International License.
Funding data
-
Universidad de los Andes
Grant numbers INV-2021-117-2216
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























