Stroke associated with primary membranous nephropathy in a young adult: Case report
Abstract
Introduction. Stroke in young individuals is becoming increasingly prevalent worldwide. Its causes can vary widely, so a thorough investigation by a multidisciplinary team is needed. Pinpointing the precise underlying pathology responsible for the stroke yields benefits for patients, particularly in recurrent events.
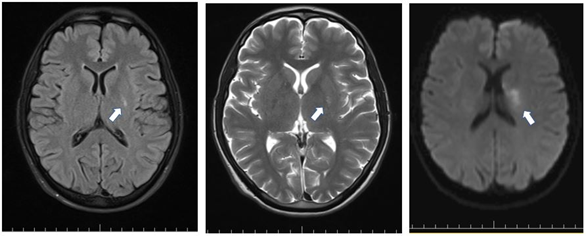
Case presentation. A 38-year-old man presented to the emergency department with symptoms suggestive of stroke, including right hemiparesis, dysarthria, ataxic gait, and right central facial palsy. The brain magnetic resonance image revealed an ischemic lesion located in the left basal ganglia and near the corona radiata. Following an extensive workup, a diagnosis of nephrotic was reached. Histopathology and the exclusion of secondary causes confirmed primary membranous nephropathy as the underlying condition.
The patient underwent treatment tailored to address the specific glomerulopathy, along with anticoagulation therapy and immunosuppression as per current guidelines. Subsequent assessments showed stabilization of renal function, resolution of the edema, and the absence of new thromboembolic events during follow-up.
Conclusion. The nephrotic syndrome should be recognized as a potential underlying cause of stroke in young patients and, therefore, it should be included in the differential diagnosis during the evaluation of patients with coagulopathies. Nephrotic syndrome screening may be done by conducting a simple urinalysis readily available in most healthcare facilities.
This underlines the importance of considering renal pathology in the assessment of stroke etiologies, especially when coagulation abnormalities are present.
Downloads
References
Ekker MS, Boot EM, Singhal AB, Tan KS, Debette S, Tuladhar AM, et al. Epidemiology, aetiology, and management of ischaemic stroke in young adults. Lancet Neurol. 2018;17:790-801. https://doi.org/10.1016/S1474-4422(18)30233-3
Boot E, Ekker MS, Putaala J, Kittner S, De Leeuw F-E, Tuladhar AM. Ischaemic stroke in young adults: A global perspective. J Neurol Neurosurg Psychiatry. 2020;91:411-7. https://doi.org/10.1136/jnnp-2019-322424
Stack CA, Cole JW. A diagnostic approach to stroke in young adults. Curr Treat Options Cardiovasc Med. 2017;19:1-19. https://doi.org/10.1007/s11936-017-0587-6
Adams Jr HP, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24:35-41. https://doi.org/10.1161/01.STR.24.1.35
Kerlin BA, Ayoob R, Smoyer WE. Epidemiology and pathophysiology of nephrotic syndrome –associated thromboembolic disease. Clin J Am Soc Nephrol. 2012;73:513-20. https://doi.org/10.2215/CJN.10131011
Zou H, Li Y, Xu G. Management of anticoagulation and antiplatelet therapy in patients with primary membranous nephropathy. BMC Nephrol. 2019;20:1-11. https://doi.org/10.1186/s12882-019-1637-y
Francis JM, Beck Jr LH, Salant DJ. Membranous nephropathy: A journey from bench to bedside. Am J Kidney Dis. 2016;68:138-47. https://doi.org/10.1053/j.ajkd.2016.01.030
Alsharhan L, Beck Jr LH. Membranous nephropathy: Core Curriculum 2021. Am J Kidney Dis. 2021. https://doi.org/10.1053/j.ajkd.2020.10.009
Beck Jr LH, Bonegio RG, Lambeau G, Beck DM, Powell DW, Cummins TD, et al. M-type phospholipase A2 receptor as target antigen in idiopathic membranous nephropathy. N Engl J Med. 2009;361:11-21. https://doi.org/10.1056/NEJMoa0810457
Fahal IH, McClelland P, Hay C, Bell G. Arterial thrombosis in the nephrotic syndrome. Postgrad Med J. 1994;70:905-9. https://doi.org/10.1136/pgmj.70.830.905
Lee T, Derebail VK, Kshirsagar AV, Chung Y, Fine JP, Mahoney S, et al. Patients with primary membranous nephropathy are at high risk of cardiovascular events. Kidney Int. 2016;89:1111-8. https://doi.org/10.1016/j.kint.2015.12.041
Roy C, Deschaintre Y, Sabbagh R, Roy D, Cardinal H, Bollée G. Ischemic stroke of possible embolic etiology associated with nephrotic syndrome. Kidney Int Rep. 2017;2:988-94. https://doi.org/10.1016/j.ekir.2017.04.004
Ponticelli C, Altieri P, Scolari F, Passerini P, Roccatello D, Cesana B, et al. A randomized study comparing methylprednisolone plus chlorambucil versus methylprednisolone plus cyclophosphamide in idiopathic membranous nephropathy. J Am Soc Nephrol. 1998;9:444-50. https://doi.org/10.1681/ASN.V93444
Fervenza FC, Appel GB, Barbour SJ, Rovin BH, Lafayette RA, Aslam N, et al. Rituximab or cyclosporine in the treatment of membranous nephropathy. N Engl J Med. 2019;381:36-46. https://doi.org/10.1056/NEJMoa1814427
Luzardo L, Ottati G, Cabrera J, Trujillo H, Garau M, Bedat CG, et al. Substitution of oral for intravenous cyclophosphamide in membranous nephropathy. Kidney360. 2020;1:943-9. https://doi.org/10.34067/KID.0002802020
Some similar items:
- Carlos Santiago Uribe, Paula Andrea Millán, María Isabel Montes, Dagoberto Cabrera, Alejandra Arboleda, Biopercular syndrome: report of two cases and literature review , Biomedica: Vol. 28 No. 2 (2008)
- Jorge de Jesús Cantillo, Rocío del Pilar López, Rafael Enrique Andrade, Glomerular deposition disease, regarding a case of fibrillary glomerulonephritis , Biomedica: Vol. 29 No. 4 (2009)
- Hernán Bayona , María Camila Valencia, Angélica Peña , Natalia Ramírez, Carlos Martínez , Fatal reversible cerebral vasoconstriction syndrome: An unusual presentation of a rare disease , Biomedica: Vol. 41 No. 2 (2021)
- Viviana Alexandra Martínez-Villota , Paulo Francisco Mera-Martínez, José Darío Portillo-Miño, Massive acute ischemic stroke after Bothrops spp. envenomation in southwestern Colombia: Case report and literature review , Biomedica: Vol. 42 No. 1 (2022)
- Ozge Altintas Kadirhan , Okkes Taha Kucukdagli , Bedia Gulen, The effectiveness of serum S100B, TRAIL, and adropin levels in predicting clinical outcome, final infarct core, and stroke subtypes of acute ischemic stroke patients , Biomedica: Vol. 42 No. Sp. 1 (2022): Mayo, Enfermedades crónicas en el trópico
- Catalina Cáceres , Álvaro José Lora , Silvia Juliana Villabona , María Catalina Rocha , Paul Anthony Camacho, Adherence to pharmacological treatment in non-communicable chronic diseases in the Colombian population: Systematic review and meta-analysis , Biomedica: Vol. 43 No. Sp. 3 (2023): Enfermedades crónicas no transmisibles
Copyright (c) 2024 Biomedica

This work is licensed under a Creative Commons Attribution 4.0 International License.
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























