In vitro activity of tedizolid and other comparator drugs in methicillin-resistant Staphylococcus aureus isolates in skin and soft tissue infections in seven Colombian hospitals
Abstract
Introduction: Methicillin-resistant Staphylococcus aureus (MRSA) causes severe skin and soft tissue infections in hospitals and, more recently, in the community. Tedizolid is a new second-generation oxazolidinone derivative having greater in vitro potency than linezolid against this type of microorganism.
Objectives: To evaluate the antimicrobial activity of tedizolid and other comparator antibiotics in MRSA isolates causing skin and soft tissue infections in Colombian hospitals.
Materials and methods: We conducted a prospective, multi-center descriptive study in seven tertiary-level hospitals in Colombia along a 12-month period. MRSA isolates were collected from adult patients with skin and soft tissue infections. Tedizolid, linezolid, vancomycin, daptomycin, trimethoprim-sulfamethoxazole, and clindamycin minimum inhibitory concentration (MIC) was determined by ETEST® (bioMérieux).
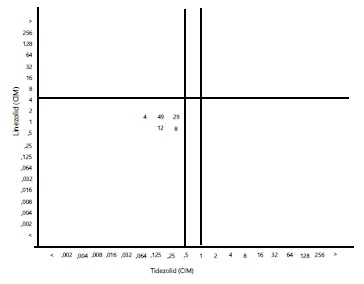
Results: MRSA isolates were obtained from 102 patients with an average age of 46.8 years of whom 56 (54.9%) were men. Infection was community-acquired in 77 cases (75.4%). Abscess-related samples predominated (69 patients: 67.6%). All isolates were susceptible to tedizolid, linezolid, daptomycin, trimethoprim-sulfamethoxazole, and vancomycin. Tedizolid had greater in vitro activity than linezolid. Tedizolid MIC intervals ranged from 0.125 μg/mL to 0.5 μg/mL while those of linezolid ranged from 1μg/mL to 2μg/mL.
Conclusions: MRSA strains circulating in Colombia are highly susceptible to tedizolid and can be considered a therapeutic alternative for hospitals and/or community-acquired skin and soft tissue infections.
Downloads
References
Gould IM, David MZ, Esposito S, Garau J, Lina G, Mazzei T, et al. New insights into meticillin-resistant Staphylococcus aureus (MRSA) pathogenesis, treatment and resistance. Int J Antimicrob Agents. 2012;39:96-104. https://doi.org/10.1016/j.ijantimicag.2011.09.028
Naimi TS, LeDell KH, Como-Sabetti K, Borchardt SM, Boxrud DJ, Etienne J, et al. Comparison of community and health care-associated methicillin-resistant Staphylococcus aureus infection. JAMA. 2003;290:2976-84. https://doi.org/10.1001/jama.290.22.2976
Fridkin SK, Hageman JC, Morrison M, Sanza LT, Como-Sabetti K, Jernigan JA, et al. Methicillin-resistant Staphylococcus aureus disease in three communities. N Engl J Med. 2005;352:1436-44. https://doi.org/10.1056/NEJMoa043252
Ortiz-Covarrubiasa A, Fang E, Prokocimer PG, Flanaganb SD, Zhu X. Surveillance of tedizolid activity and resistance: In vitro susceptibility of Gram-positive pathogens collected over 5 years from the United States and Europe. Braz J Infect Dis. 2016;20:184-92. https://doi.org/10.1016/j.bjid.2015.12.007
Ochoa V, Guzmán AR, Caicedo Y. Infección por Staphylococcus aureus meticilino resistente adquirido en la comunidad. Gastrohnup. 2012;2:S46-57.
Fala L. Sivextro (tedizolid phosphate) approved for the treatment of adults with acute bacterial skin and skins tructure infections. Am Health Drug Benefits. 2015;8:111-5.
Instituto Nacional de Salud. Resultados del programa de vigilancia por laboratorio de resistencia antimicrobiana en infecciones asociadas a la atención en salud (IAAS) 2015. Fecha de consulta: 10 de marzo de 2017. Disponible en: http://www.ins.gov.co/tramites-y-servicios/examenes-de-inter%C3%A9sen-salud-publica/Microbiologa/Resultados%20del%20Programa%20de%20Vigilancia%20por%20Laboratorio%20de%20Resistencia%20antimicrobiana%20en%20%20IAAS%20%202015.pdf
Grupo para el Estudio de la Resistencia de los Antimicrobianos en Medellín, Grupo Gérmen. Microorganismos. Fecha de consulta: 10 de marzo de 2017. Disponible en: http://www.grupogermen.org/pdf/staphylococcus_aureus_12_14.pdf
Grupo para el Control de Resistencia Bacteriana de Bogotá (Grebo). Boletín informativo, años 2012-2014. Fecha de consulta: 20 de marzo de 2017. Disponible en:
http://www.grebo.org/grebo_site/jgrebo/documentos/Boletin_Grebo_2015.pdf
Zhanel GG, Love R, Adam H, Golden A, Zelenitsky S, Schweizer F, et al. Tedizolid: A novel oxazolidinone with potent activity against multidrug-resistant gram-positive pathogens. Drugs. 2015;75:253-70. https://doi.org/10.1007/s40265-015-0352-7
Bouza E, Muñoz P, Burillo A. The role of tedizolid in skin and soft tissue infections. Curr Opin Infect Dis. 2018;31:131-40. https://doi.org/10.1097/QCO.0000000000000439
Riedel S, Neoh KM, Eisinger S, Dam L, Tekle T, Carroll KC. Comparison of commercial antimicrobial susceptibility test methods for testing of Staphylococcus aureus and Enterococci against vancomycina, daptomacyne and linezolid. J Clin Microbiol. 2014;52:2216-22. https://doi.org/10.1128/JCM.00957-14
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; approved standard. Twenty third information supplement. Document M100-S26. Wayne: CLSI; 2016.
Purrello SM, Garau J, Giamarellos E, Mazzei T, Pea F, Soriano A, et al. Methicillin-resistant Staphylococcus aureus infections: A review of the currently available treatment options. J Glob Antimicrob Resist. 2016;7:178-86. https://doi.org/10.1016/j.jgar.2016.07.010
Cortés JA, Gómez CA, Cuervo SI, Leal AL. Community acquired methicillin-resistant Staphylococcus aureus in Bogotá, Colombia: Public Health implications. Rev Salud Pública. 2007;9:448-54. https://doi.org/10.1590/S0124-00642007000300013
Portillo BC, Moreno JE, Yomayusa N, Álvarez CA, Cardozo BE, Escobar JA, et al. Molecular epidemiology and characterization of virulence genes of community acquired and hospital-acquired methicillin-resistant Staphylococcus aureus isolates in Colombia. Int J Infect Dis. 2013;17:744-9. http://dx.doi.org/10.1016/j.ijid.2013.02.029
Jiménez JN, Ocampo AM, Vanegas JM, Rodríguez EA, Mediavilla JR, Chen L, et al. A comparison of methicillin resistant and methicillin-susceptible Staphylococcus aureus reveals no clinical and epidemiological but molecular differences. Int J Med Microbiol. 2013;303:76-83. https://doi.org/10.1016/j.ijmm.2012.12.003
Bensaci M, Sahm D. Surveillance of tedizolid activity and resistance: In vitro susceptibility of Gram-positive pathogens collected over 5 years from the United States and Europe. Diagn Microbiol Infect Dis. 2017;87:133-8. https://doi.org/10.1016/j.diagmicrobio.2016.10.009
Biedenbach DJ, Bouchillon SK, Johnson B, Alder J, Sahm DF. In vitro activity of tedizolid against Staphylococcus aureus and Streptococcus pneumoniae colleted in 2013 and 2014 from sites in Latin America, Australia, New Zealand and China. Eur J Clin Microbiol Infect Dis. 2016;35:1933-9.
https://doi.org/10.1007/s10096-016-2744-3
Jiménez A, Fajardo C. Identificación de Staphylococcus aureus meticilino resistente con concentración inhibitoria mínima elevada a la vancomicina mediante los métodos de E-test y automatizados. Infectio. 2013;17:39-42. https://doi.org/10.1016/S0123-9392(13)70047-X
Holmes NE, Turnidge JD, Munckhof WJ, Robinson JO, Korman TM, O’Sullivan MV, et al. Vancomycin AUC/MIC ratio and 30-day mortality in patients with Staphylococcus aureus bacteremia. Antimicrob Agents Chemother. 2013;57:1654-63. https://doi.org/10.1128/AAC.01485-12
McCool R, Gould IM, Eales J, Barata T, Arber M. Systematic review and network meta-analysis of tedizolid for the treatment of acute bacterial skin and skin structure infections caused by MRSA. BMC Infect Dis. 2017;17:39. http://doi.org/10.1016/j.jval.2015.03.1341
Burdette SD, Trotman R. Tedizolid: The first once-daily oxazolidinone class antibiotic. Clin Infect Dis 2015;61:1315-21. https://doi.org/10.1093/cid/civ501
Long KS, Vester B. Resistance to linezolid caused by modifications at its binding site on the ribosome. Antimicrob Agents Chemother. 2012;56:603-12. https://doi.org/10.1128/AAC.05702-11
Some similar items:
- Natalie Nader, Ramón Iván Medina, Luz Ángela Pescador, Barbarita María Mantilla, Juan Sebastián Bravo, Carlos Hernando Gómez, Characterization of patients with bacteremia by methicillin-resistant Staphylococcus aureus in a high-complexity military hospital , Biomedica: Vol. 39 No. Sp. 1 (2019): Suplemento 1, Microbiología médica, mayo
- Narda María Olarte, Ismael Alberto Valderrama, Karlo Roberto Reyes, Martha Isabel Garzón, Javier Antonio Escobar, Betsy Esperanza Castro, Natasha Vanegas, Methicillin-resistant Staphylococcus aureus colonization in a Colombian hospital intensive care unit: phenotypic and molecular characterization , Biomedica: Vol. 30 No. 3 (2010)
- Constanza Pardo, Ricardo Cendales, Survival analysis of cervical cancer patients , Biomedica: Vol. 29 No. 3 (2009)
- Raúl Murillo, Ricardo Cendales, Carolina Wiesner, Marion Piñeros, Sandra Tovar, Effectiveness of cytology-based cervical cancer screening in the Colombian health system , Biomedica: Vol. 29 No. 3 (2009)
- Sandra Lorena Girón, Julio César Mateus, Fabián Méndez, Impact of an open waste disposal site on the occurrence of respiratory symptoms and on health care costs of children , Biomedica: Vol. 29 No. 3 (2009)
- José Joaquín Carvajal, Ligia Inés Moncada, Mauricio Humberto Rodríguez, Ligia del Pilar Pérez, Víctor Alberto Olano, Characterization of Aedes albopictus (Skuse, 1894) (Diptera:Culicidae) larval habitats near the Amazon River in Colombia , Biomedica: Vol. 29 No. 3 (2009)
- Andrés Páez, Gloria Rey, Carlos Agudelo, Alvaro Dulce, Edgar Parra, Hernando Díaz-Granados, Damaris Heredia, Luis Polo, Outbreak of urban rabies transmitted by dogs in Santa Marta, northern Colombia , Biomedica: Vol. 29 No. 3 (2009)
- Patricia Escobar, Katherine Paola Luna, Indira Paola Hernández, César Mauricio Rueda, María Magdalena Zorro, Simon L. Croft, In vitro susceptibility of Trypanosoma cruzi strains from Santander, Colombia, to hexadecylphosphocholine (miltefosine), nifurtimox and benznidazole , Biomedica: Vol. 29 No. 3 (2009)
- Jaime E. Bernal, Martha Lucía Tamayo , Ignacio Briceño , Escilda Benavides , Newborn screening in Colombia: The experience of a private program in Bogotá , Biomedica: Vol. 44 No. 1 (2024)
- Mauricio Beltrán, María Cristina Navas, María Patricia Arbeláez, Jorge Donado, Sergio Jaramillo, Fernando De la Hoz, Cecilia Estrada, Lucía del Pilar Cortés, Amalia de Maldonado, Gloria Rey, Seroprevalence of hepatitis B virus and human immunodeficiency virus infection in a population of multiply-transfused patients in Colombia , Biomedica: Vol. 29 No. 2 (2009)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























