Multidrug resistance and risk factors associated with community-acquired urinary tract infections caused by Escherichia coli in Venezuela
Abstract
Introduction: The treatment of urinary tract infections has become more challenging due to the increasing frequency of multidrug-resistant Escherichia coli in human populations.
Objective: To characterize multidrug-resistant E. coli isolates causing community-acquired urinary tract infections in Cumaná, Venezuela, and associate possible risk factors for infection by extended-spectrum beta-lactamases (ESBL)-producing isolates.
Materials and methods: We included all the patients with urinary tract infections attending the urology outpatient consultation and emergency unit in the Hospital de Cumaná, Estado Sucre, Venezuela, from January through June, 2014. blaTEM, blaSHV and blaCTX-M genes detection was carried out by PCR.
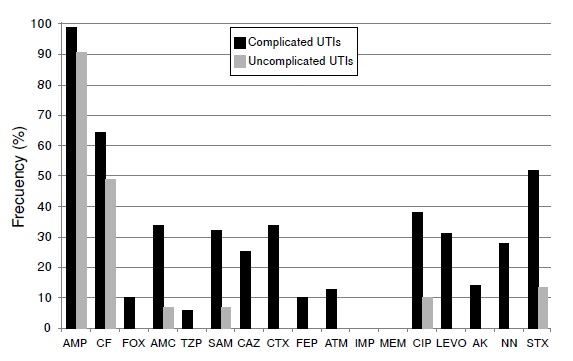
Results: We found a high prevalence of multidrug-resistant E. coli (25.2%) with 20.4% of the isolates producing ESBL. The ESBL-producing isolates showed a high frequency (66.7%) of simultaneous resistance to trimethoprim-sulphamethoxazole, fluoroquinolones and aminoglycosides compared to non-producing isolates (2.4%). Of the resistant isolates, 65.4% carried the blaTEM gene, 34.6% the blaCTX-M and 23.1% the blaSHV. The blaCTX-M genes detected belonged to the CTX-M-1 and CTX-M-2 groups. Plasmid transfer was demonstrated by in vitro conjugation in 17 of the 26 ESBL-producing isolates. All three genes detected were transferred to the transconjugants. Age over 60 years, complicated urinary tract infections and previous use of a catheter predisposed patients to infection by ESBL-producing E. coli.
Conclusions: The high frequency of multidrug-resistant ESBL-producing isolates should alert the regional health authorities to take measures to reduce the risk of outbreaks caused by these types of bacteria in the community.
Downloads
References
Laupland KB, Ross T, Pitout JD, Church DL, Gregson DB. Community-onset urinary tract infections: A population-based assessment. Infection. 2007;35:150. https://doi.org/10.1007/s15010-007-6180-2
Peirano G, Pitout JD. Molecular epidemiology of Escherichia coli producing CTX-M β-lactamases: The worldwide emergence of clone ST131 O25: H4. Int J Antimicrob Agents. 2010;35:316-21. https://doi.org/10.1016/j.ijantimicag.2009.11.003
Guzmán-Blanco M, Labarca JA, Villegas MV, Gotuzzo E. Extended spectrum β-lactamase producers among nosocomial Enterobacteriaceae in Latin America. Braz J Infect Dis. 2014;18:421-33. https://doi.org/10.1016/j.bjid.2013.10.005
Cantón R, González-Alba JM, Galán JC. CTX-M enzymes: Origin and diffusion. Front Microbiol. 2012;3:110. https://doi.org/10.3389/fmicb.2012.00110
Bonnet R. Growing group of extended-spectrum β-lactamases: The CTX-M enzymes. Antimicrob Agents Chemother. 2004;48:1-4. https://doi.org/10.1128/AAC.48.1.1-14.2004
Dhillon RH, Clark J. ESBLs: A clear and present danger? Crit Care Res Pract. 2012;2012:625170. https://doi.org/10.1155/2012/625170
Narváez P, Pedroza R, Alonso G, Rodríguez-Lemoine V. Caracterización de plásmidos de resistencia a antibióticos en aislados nosocomiales del Hospital Universitario de Caracas. Rev Soc Ven Microbiol. 2005;25:29-34.
Guzmán M, Alonso G. Caracterización de ß-lactamasas de espectro extendido (BLEE) en cepas nosocomiales de K. pneumoniae. Sucre-Venezuela. Invest Clin. 2009;50:419-31.
Guevara A, Machado S, Manrique E. Urinary infections acquired in community: Epidemiology, resistance to antibiotics and therapeutic options. Kasmera. 2011;39:87-97.
Hernández E, Araque M, Millán Y, Millán B, Vielma S. Prevalencia de β-lactamasa CTX-M-15 en grupos filogenéticos de Escherichia coli uropatógena aisladas en pacientes de la comunidad en Mérida, Venezuela. Invest Clin. 2014;55:32-43.
de Cueto M. La microbiología en el diagnóstico de la infección del tracto urinario. In: Pigrau C, editor. Infección del tracto urinario. Primera edición. Madrid: Salvat; 2013. p. 11-22.
Nicolle LE, Bradley S, Colgan R, Rice JC, Schaeffer A, Hooton TM. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis. 2005;40:643-54. https://doi.org/10.1086/427507
Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, et al. Health care associated bloodstream infections in adults: A reason to change the accepted definition of community-acquired infections. Ann Intern Med. 2002;137:791-7. https://doi.org/10.7326/0003-4819-137-10-200211190-00007
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; twenty-four informational supplement, M100-S24. Wayne, PA: CLSI; 2014. p. 226.
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrugresistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18:268-81. https://doi.org/10.1111/j.1469-0691.2011.03570.x
Eckert C, Gautier V, Saladin-Allard M, Hidri N, Verdet C, Ould-Hocine Z, et al. Dissemination of CTX-M- type beta-lactamases among clinical isolates of Enterobacteriaceae in Paris, France. Antimicrob Agents Chemother. 2004;48:1249-55. https://doi.org/10.1128/AAC.48.4.1249-1255.2004
Haeggman S, Löfdal S, Poauw A, Verhoef J, Brisse S. Diversity and evolution of the class A chromosomal beta-lactamase gene in Klebsiella pneumoniae. Antimicrob Agents Chemother. 2004;48:2400-8. https://doi.org/10.1128/AAC.48.7.2400-2408.2004
Eldestein M, Pimkin M, Palagin I, Eldestein I, Stratchounski L. Prevalence and molecular epidemiology of CTX-M extended spectrum β-lactamase-producing Escherichia coli and Klebsiella pneumoniae in Russian hospitals. Antimicrob Agents Chemother. 2003;47:3724-32. https://doi.org/10.1128/AAC.47.12.3724-3732.2003
Mahboobeh N, Forghanifard M, Moshrefi S. Prevalence and molecular characterization of plasmid-mediated extended-spectrum β-lactamase genes (blaTEM, blaCTX and blaSHV) among urinary Escherichia coli clinical isolates in Mashhad, Iran. Iran J Basic Med Sci. 2012;15:833-9.
Sánchez GV, Baird AM, Karlowsky JA, Master RN, Bordon JM. Nitrofurantoin retains antimicrobial activity against multidrug-resistant urinary Escherichia coli from US outpatients. J Antimicrob Chemother. 2014;69:3259-62. https://doi.org/10.1093/jac/dku282
Alos JI. Epidemiología y etiología de la infección urinaria comunitaria. Sensibilidad antimicrobiana de los principales patógenos y significado clínico de la resistencia. Enferm Infecc Microbiol Clin. 2005;23:3-8. https://doi.org/10.1157/13091442
Spellberg B, Talbot G, Brass E, Bradley J, Boucher H, Gilbert D, et al. Position paper: Recommended design features of future clinical trials of antibacterial agents for community cquired pneumonia. Clin Infect Dis. 2008;47(Suppl.3):S249-65. https://doi.org/10.1086/591411
Winokur PL, Canton R, Casellas JM, Legakis N. Variations in the prevalence of strains expressing an extended-spectrum beta-lactamase phenotype and characterization of isolates from Europe, the Americas, and the Western Pacific Region. Clin Inf Dis. 2001;32(Suppl.2):S94-103. https://doi.org/10.1086/320182
Canton R, Coque T. The CTX-M beta-lactamase pandemic. Curr Opin Microbiol. 2006;9:466-75. https://doi.org/10.1016/j.mib.2006.08.011
Hussain A, Ewers C, Nandanwar N, Guenther S, JadhavS, Wieler LH, et al. Multiresistant uropathogenic Escherichia coli from a region in India where urinary tract infections are endemic: Genotypic and phenotypic characteristics of sequence type 131 isolates of the CTX-M-15 extended-spectrum-beta-lactamase-producing lineage. Antimicrob Agents Chemother. 2012;56:6358. https://doi.org/10.1128/AAC.01099-12
Ben-Ami R, Rodríguez-Baño J, Arslan H, Pitout JD, Quentin C, Calbo ES, et al. A multinational survey of risk factors for infection with extended-spectrum beta-lactamase producing enterobacteriaceae in nonhospitalized patients. Clin Infect Dis. 2009;49:682-90. https://doi.org/10.1086/604713
Ahmed O, Alfadel O, Asghar H, Elhassan M. Prevalence of TEM, SHV and CTX-M genes in Escherichia coli and Klebsiella spp. urinary isolates from Sudan with confirmed ESBL phenotype. Life Sci J. 2013;10:191-5.
Radice M, Power P, Di Conza J, Gutkind G. Early dissemination of CTX-M-derived enzymes in South America. Antimicrob Agents Chemother. 2002;46:602-4. https://doi.org/10.1128/AAC.46.2.602-604.2002
Wang H, Kelkar S, Wu W, Chen M, Quinn J. Clinical isolates of Enterobacteriaceae producing extended-spectrum b-lactamases: Prevalence of CTX-M-3 at a hospital in China. Antimicrob Agents Chemother 2003;47:790-3. https://doi.org/10.1128/AAC.47.2.790-793.2003
Yamasaki K, Komatsu M, Yamashita T, Shimakawa K, Ura T, Nishio H, et al. Production of CTX-M-3 extended-spectrum beta-lactamase and IMP-1 metallo beta-lactamase by five Gramnegative bacilli: Survey of clinical isolates from seven laboratories collected in 1998 and 2000, in the Kinki region of Japan. J Antimicrob Chemother. 2003;51:631-8. https://doi.org/10.1093/jac/dkg103
Kung CH, Ku WW, Lee CH, Fung CP, Kuo SC, Chen TL, et al. Epidemiology and risk factors of community-onset urinary tract infection caused by extended-spectrum β-lactamase producing Enterobacteriaceae in a medical center in Taiwan: A prospective cohort study. J Microbiol Immunol Infect. 2015;48:168-74. https://doi.org/10.1016/j.jmii.2013.08.006
Araque M, Millán B, Mendoza E, Salas M. CTX-M-32 beta-lactamase-producing uropathogenic Escherichia coli isolated in Latin America. J Infect Dev Ctries. 2013;7:432-5. https://doi.org/10.3855/jidc.3488
Coque T, Baquero F, Cantón R. Increasing prevalence of ESBL-producing enterobacteriaceae in Europe. Eurosurveillance. 2008;47:19-29. https://doi.org/10.2807/ese.13.47.19044-en
Rossolini G, D’Andrea M, Mugnaioli C. The spread of CTX-M-type extended-spectrum betalactamases. Clin Microbiol Infect. 2008;14:33-41. https://doi.org/10.1111/j.1469-0691.2007.01867.x
Banerjee R, Strahilevitz J, Johnson JR, Nagwekar PP, Schora DM, Shevrin I, et al. Predictors and molecular epidemiology of community-onset extended-spectrum β-lactamase-producing Escherichia coli infection in a Midwestern community. Infect Control Hosp Epidemiol. 2013;34:947-53. https://doi.org/10.1086/671725
Blanco VM, Maya JJ, Correa A, Perenguez M, Muñoz JS, Motoa G, et al. Prevalencia y factores de riesgo para infecciones del tracto urinario de inicio en la comunidad causadas por Escherichia coli productor de betalactamasas de espectro extendido en Colombia. Enferm Infecc Microbiol Clin. 2016;34:559-65. https://doi.org/10.1016/j.eimc.2015.11.017
Kronenberg A, Hilty M, Endimiani A, Muhlemann K. Temporal trends of extended-spectrum cephalosporin-resistant Escherichia coli and Klebsiella pneumoniae isolates in in- and outpatients in Switzerland, 2004 to 2011. Euro Surveill. 2013;18:20484. https://doi.org/10.2807/ese.18.21.20484-en
Anesi JA, Lautenbach E, Nachamkin I, Garrigan C, Bilker WB, Wheeler M, et al. Clinical and molecular characterization of community-onset urinary tract infections due to extendedspectrum cephalosporin-resistant Enterobacteriaceae. Infect Control Hosp Epidemiol. 2016;37:1433-9. https://doi.org/10.1017/ice.2016.225
Bours PH, Polak R, Hoepelman AI, Delgado E, Jarquin A, Matute AJ. Increasing resistance in community-acquired urinary tract infections in Latin America, five years after the implementation of national therapeutic guidelines. Int J Infect Dis. 2010;14:e770-4. https://doi.org/10.1016/j.ijid.2010.02.2264
Seija V, Fratchez V, Ventura V, Pintos M, González M. Factores asociados al desarrollo de infección urinaria de origen comunitario causada por Escherichia coli resistente a fluoroquinolonas. Rev Chilena Infectol. 2014;31:400-5. https://doi.org/10.4067/S0716-10182014000400004
Some similar items:
- Edna Catering Rodríguez, Sandra Yamile Saavedra, Lucy Angeline Montaño, Diana Patricia Sossa, Francia Patricia Correa, Jireh Alejandra Vaca, Carolina Duarte, Characterization of extended spectrum β-lactamases in Colombian clinical isolates of non-typhoidal Salmonella enterica between 1997 and 2022 , Biomedica: Vol. 43 No. 3 (2023)
- Ana María Perilla, Camilo González, Sandra Liliana Valderrama, Natasha Vanegas, Bibiana Chavarro, Luis Carlos Triana, José Roberto Támara, Carlos Arturo Álvarez, Necrotizing pneumonia by community-acquired, methicillin-resistant Staphylococcus aureus in Colombia , Biomedica: Vol. 29 No. 4 (2009)
- Nadia Yadira Castañeda, Jacqueline Chaparro-Olaya, Jaime E. Castellanos, Production and characterization of a polyclonal antibody against rabies virus phosphoprotein , Biomedica: Vol. 27 No. 2 (2007)
- Ingrid Yamile Pulido, José Ramón Mantilla, Emilia María Valenzuela, María Teresa Reguero, Elsa Beatriz González, Distribution of extended spectrum β-lactamases-codifying genes in Klebsiella pneumoniae isolates from hospitals of Bogota, D.C., Colombia , Biomedica: Vol. 31 No. 1 (2011)
- José Ramón Mantilla, María Teresa Reguero, Elsa Beatriz González, Ibonne Ayde García, Aura Lucía Leal, Paula Andrea Espinal, Celia Alpuche, Ismael Alberto Valderrama, Martha Isabel Garzón, Narda María Olarte, Molecular characterization of an outbreak caused by CTX-M-12-producing Klebsiella pneumoniae in a Colombian hospital´s neonatal intensive care unit , Biomedica: Vol. 26 No. 3 (2006)
- Javier Antonio Escobar, Ingrid Tatiana Gómez, Martha Johanna Murillo, Betsy Esperanza Castro, Bibiana Chavarro, Ricaurte Alejandro Márquez, Natasha Vanegas, Design of two molecular methodologies for the rapid identification of Colombian community-acquired methicillin-resistant Staphylococcus aureus isolates , Biomedica: Vol. 32 No. 2 (2012)
- Andrés F. Henao-Martínez, Guido R. González-Fontal, Steven Johnson, A case of community-acquired Acinetobacter junii-johnsonii cellulitis , Biomedica: Vol. 32 No. 2 (2012)
- Beatriz Millan, David Castro, Maria Araque, Bárbara Ghiglione, Gabriel Gutkind, ISCR1 associated with blaCTX-M-1 y blaCTX-M-2 genes in IncN and IncFIIA plasmids isolated from Klebsiella pneumoniae of nosocomial origin in Mérida, Venezuela , Biomedica: Vol. 33 No. 2 (2013)
- Sonia Isabel Cuervo, Ricardo Sánchez, Julio César Gómez-Rincón, Cielo Almenares, Juan Pablo Osorio, María José Vargas, Behavior of carbapenemase-producing Klebsiella pneumoniae cases in cancer patients at a third level hospital in Bogotá, D.C. , Biomedica: Vol. 34 (2014): Abril, Suplemento 1, Resistencia bacteriana
- Alfonso Benítez-Páez, Sonia Cárdenas-Brito, Mauricio Corredor, Magda Villarroya, María Eugenia Armengod, Impairing methylations at ribosome RNA, a point mutation-dependent strategy for aminoglycoside resistance: The rsmG case , Biomedica: Vol. 34 (2014): Abril, Suplemento 1, Resistencia bacteriana
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























