Oxidative stress in endothelial cells induced by the serum of women with different clinical manifestations of the antiphospholipid syndrome
Abstract
Introduction: The antiphospholipid syndrome is characterized by the persistent presence of antiphospholipid antibodies and clinical manifestations of thrombosis or gestational morbidity that are associated with oxidative stress and endothelial dysfunction.
Objective: To evaluate markers of oxidative stress in endothelial cells induced by the serum from women with different clinical manifestations of the antiphospholipid syndrome, and to analyze the antioxidant capacity of the sera.
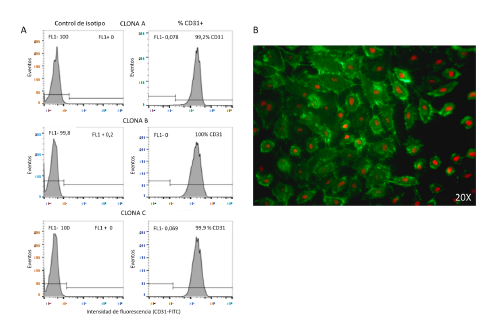
Materials and methods: We included 48 women who were classified as follows: presence of antiphospholipid antibodies and clinical criteria of gestational morbidity alone, vascular thrombosis only, and gestational morbidity/vascular thrombosis. Control groups included antiphospholipid antibodies negative women. In an in vitro model of endothelial cells stimulated with sera from women included in the groups, some markers of oxidative stress were determined by flow cytometry. The antioxidant capacity in the sera of these women was analyzed.
Results: The sera from the groups of women with antiphospholipid syndrome that presented thrombosis, with or without gestational morbidity, generated a significant increase (p<0.05 and p<0.001) in endothelial oxidative stress markers in contrast to the control of normal human serum. There were no differences in the effect of the sera from the different study groups on endothelial lipid peroxidation. Also, there was also no difference in the antioxidant activity of the sera.
Conclusion: Mitochondrial oxidative stress in the endothelium is associated with the presence of thrombosis; instead, its association with gestational morbidity generates intracellular oxidative stress.
Downloads
References
Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost. 2006;4:295-306. https://doi.org/10.1111/j.1538-7836.2006.01753.x
Esteve-Valverde E, Ferrer-Oliveras R, Alijotas-Reig J. Obstetric antiphospholipid syndrome. Rev Clin Esp. 2016;216:135-45. https://doi.org/10.1016/j.rce.2015.09.003
Cervera R, Serrano R, Pons-Estel GJ, Ceberio-Hualde L, Shoenfeld Y, de Ramon E, et al. Morbidity and mortality in the antiphospholipid syndrome during a 10-year period: A multicentre prospective study of 1000 patients. Ann Rheum Dis. 2015;74:1011-8. https://doi.org/10.1136/annrheumdis-2013-204838
Meroni PL, Borghi MO, Raschi E, Tedesco F. Pathogenesis of antiphospholipid syndrome: Understanding the antibodies. Nat Rev Rheumatol. 2011;7:330-9. https://doi.org/10.1038/nrrheum.2011.52
Chighizola CB, Raschi E, Borghi MO, Meroni PL. Update on the pathogenesis and treatment of the antiphospholipid syndrome. Curr Opin Rheumatol. 2015;27:476-82.
https://doi.org/10.1097/BOR.0000000000000200
Ripoll VM, Pregnolato F, Mazza S, Bodio C, Grossi C, McDonnell T, et al. Gene expression profiling identifies distinct molecular signatures in thrombotic and obstetric antiphospholipid syndrome. J Autoimmun. 2018;93:114-23. https://doi.org/10.1016/j.jaut.2018.07.002
Álvarez AM, Balcázar N, San Martín S, Markert UR, Cadavid AP. Modulation of antiphospholipid antibodies-induced trophoblast damage by different drugs used to prevent pregnancy morbidity associated with antiphospholipid syndrome. Am J Reprod Immunol. 2017;77:77(4):e12634. https://doi.org/10.1111/aji.12634
Velásquez M, Álvarez ÁM, Cadavid ÁP. Cuantificación sistematizada de la remodelación vascular in vitro en la morbilidad gestacional asociada al síndrome antifosfolípido. Rev Chil Obstet Ginecol. 2016;81:455-64 https://doi.org/10.4067/S0717-75262016000600002
Sacharidou A, Shaul PW, Mineo C. New insights in the pathophysiology of antiphospholipid syndrome. Semin Thromb Hemost. 2018;44:475-82. https://doi.org/10.1055/s-0036-1597286
López-Pedrera C, Barbarroja N, Jiménez-Gómez Y, Collantes-Estévez E, Aguirre MA, Cuadrado MJ. Oxidative stress in the pathogenesis of atherothrombosis associated with anti-phospholipid syndrome and systemic lupus erythematosus: New therapeutic approaches. Rheumatology (Oxford). 2016;55:2096-108.
https://doi.org/10.1093/rheumatology/kew054
Lum H, Roebuck KA. Oxidant stress and endothelial cell dysfunction. Am J Physiol Cell Physiol. 2001;280:C719-41. https://doi.org/10.1152/ajpcell.2001.280.4.C719
Simoncini S, Sapet C, Camoin-Jau L, Bardin N, Harle JR, Sampol J, et al. Role of reactive oxygen species and p38 MAPK in the induction of the pro-adhesive endothelial state mediated by IgG from patients with anti-phospholipid syndrome. Int Immunol. 2005;17:489-500. https://doi.org/10.1093/intimm/dxh229
Pierangeli SS, Espinola RG, Liu X, Harris EN. Thrombogenic effects of antiphospholipid antibodies are mediated by intercellular cell adhesion molecule-1, vascular cell adhesion molecule-1, and P-selectin. Circ Res. 2001;88:245-50
Kojda G, Harrison D. Interactions between NO and reactive oxygen species: Pathophysiological importance in atherosclerosis, hypertension, diabetes and heart failure. Cardiovasc Res. 1999;43:562-71.
Lubos E, Handy DE, Loscalzo J. Role of oxidative stress and nitric oxide in atherothrombosis. Front Biosci. 2008;13:5323-44.
Giannakopoulos B, Krilis SA. The pathogenesis of the antiphospholipid syndrome. N Engl J Med. 2013;368:1033-44. https://doi.org/10.1056/NEJMra1112830
Ioannou Y, Zhang JY, Qi M, Gao L, Qi JC, Yu DM, et al. Novel assays of thrombogenic pathogenicity in the antiphospholipid syndrome based on the detection of molecular oxidative modification of the major autoantigen beta2-glycoprotein I. Arthritis Rheum. 2011;63:2774-82. https://doi.org/10.1002/art.30383
Pérez-Sánchez C, Barbarroja N, Messineo S, Ruiz-Limón P, Rodríguez-Ariza A, Jiménez-Gómez Y, et al. Gene profiling reveals specific molecular pathways in the pathogenesis of atherosclerosis and cardiovascular disease in antiphospholipid syndrome, systemic lupus erythematosus and antiphospholipid syndrome with lupus. Ann Rheum Dis. 2015;74:1441-9. https://doi.org/10.1136/annrheumdis-2013-204600
Kwak JY, Gilman-Sachs A, Beaman KD, Beer AE. Autoantibodies in women with primary recurrent spontaneous abortion of unknown etiology. J Reprod Immunol. 1992;22:15-31. https://doi.org/10.1016/0165-0378(92)90003-M
Robinson KM, Janes MS, Beckman JS. The selective detection of mitochondrial superoxide by live cell imaging. Nat Protoc. 2008;3:941. https://doi.org/10.1038/nprot.2008.56
Drummen GP, Makkinje M, Verkleij AJ, den Kamp JAO, Post JA. Attenuation of lipid peroxidation by antioxidants in rat-1 fibroblasts: Comparison of the lipid peroxidation reporter molecules cis-parinaric acid and C11-BODIPY 581/591 in a biological setting. Biochim Biophys Acta. 2004;1636:136-50. https://doi.org/10.1016/j.bbalip.2003.10.013
Nicolescu AC, Li Q, Brown L, Thatcher GR. Nitroxidation, nitration, and oxidation of a BODIPY fluorophore by RNOS and ROS. Nitric Oxide. 2006;15:163-76. https://doi.org/10.1016/j.niox.2006.01.010
Mackness MI, Mackness B, Durrington PN, Connelly PW, Hegele RA. Paraoxonase: Biochemistry, genetics and relationship to plasma lipoproteins. Curr Opin Lipidol 1996;7:69-76.
Furlong CE, Richter RJ, Seidel SL, Costa LG, Motulsky AG. Spectrophotometric assays for the enzymatic hydrolysis of the active metabolites of chlorpyrifos and parathion by plasma paraoxonase/arylesterase. Anal Biochem. 1989;180:242-7. https://doi.org/10.1016/0003-2697(89)90424-7
MacDonald-Wicks LK, Wood LG, Garg ML. Methodology for the determination of biological antioxidant capacity in vitro: A review. J Sci Food Agric. 2006;86:2046-56. https://doi.org/10.1002/jsfa.2603
Serafini M, Maiani G, Ferro-Luzzi A. Alcohol-free red wine enhances plasma antioxidant capacity in humans. J Nutr. 1998;128:1003-7. https://doi.org/10.1093/jn/128.6.1003
Bertolaccini ML, Amengual O, Atsumi T, Binder WL, de Laat B, Forastiero R, et al. 'Non-criteria' aPL tests: Report of a task force and preconference workshop at the 13th International Congress on Antiphospholipid Antibodies, Galveston, TX, USA, April 2010. Lupus. 2011;20:191-205. https://doi.org/10.1177/0961203310397082
Álvarez AM, Mulla MJ, Chamley LW, Cadavid AP, Abrahams VM. Aspirin-triggered lipoxin prevents antiphospholipid antibody effects on human trophoblast migration and endothelial cell interactions. Arthritis Rheumatol. 2015;67:488-97. https://doi.org/10.1002/art.38934
Redecha P, Franzke CW, Ruf W, Mackman N, Girardi G. Neutrophil activation by the tissue factor/Factor VIIa/PAR2 axis mediates fetal death in a mouse model of antiphospholipid syndrome. J Clin Invest. 2008;118:3453-61. https://doi.org/10.1172/JCI36089
Weiler H. Tracing the molecular pathogenesis of antiphospholipid syndrome. J Clin Invest. 2008;118:3276-8. https://doi.org/10.1172/JCI37243
Wu F, Tian FJ, Lin Y. Oxidative stress in placenta: Health and diseases. Biomed Res Int. 2015;2015:293271. https://doi.org/10.1155/2015/293271
Meroni PL, Borghi MO, Grossi C, Chighizola CB, Durigutto P, Tedesco F. Obstetric and vascular antiphospholipid syndrome: Same antibodies but different diseases? Nat Rev Rheumatol. 2018;14:433-40. https://doi.org/10.1038/s41584-018-0032-6
Prinz N, Clemens N, Canisius A, Lackner KJ. Endosomal NADPH-oxidase is critical for induction of the tissue factor gene in monocytes and endothelial cells. Lessons from the antiphospholipid syndrome. Thromb Haemost. 2013;109:525-31. https://doi.org/10.1160/TH12-06-0421
Dikalov SI, Nazarewicz RR, Bikineyeva A, Hilenski L, Lassegue B, Griendling KK, et al. Nox2-induced production of mitochondrial superoxide in angiotensin II-mediated endothelial oxidative stress and hypertension. Antioxid Redox Signal. 2014;20:281-94. https://doi.org/10.1089/ars.2012.4918
Roubey RA. Tissue factor pathway and the antiphospholipid syndrome. J Autoimmun. 2000;15:217-20. https://doi.org/10.1006/jaut.2000.0397
Benhamou Y, Miranda S, Armengol G, Harouki N, Drouot L, Zahr N, et al. Infliximab improves endothelial dysfunction in a mouse model of antiphospholipid syndrome: Role of reduced oxidative stress. Vascul Pharmacol. 2015;71:93-101. https://doi.org/10.1016/j.vph.2015.03.014
Sacharidou A, Chambliss KL, Ulrich V, Salmon JE, Shen YM, Herz J, et al. Antiphospholipid antibodies induce thrombosis by PP2A activation via apoER2-Dab2-SHC1 complex formation in endothelium. Blood. 2018;131:2097-110. https://doi.org/10.1182/blood-2017-11-814681
Delgado-Alves J, Ames P, Donohue S, Stanyer L, Noorouz-Zadeh J, Ravirajan C, et al. Antibodies to high-density lipoprotein and β2-glycoprotein I are inversely correlated with paraoxonase activity in systemic lupus erythematosus and primary antiphospholipid syndrome. Arthritis Rheum. 2002;46:2686-94. https://doi.org/10.1002/art.10542
Delgado- Alves J, Mason L, Ames P, Chen P, Rauch J, Levine J, et al. Antiphospholipid antibodies are associated with enhanced oxidative stress, decreased plasma nitric oxide and paraoxonase activity in an experimental mouse model. Rheumatology (Oxford). 2005;44:1238-44. https://doi.org/10.1093/rheumatology/keh722
Fenzl V, Flegar-Mestric Z, Perkov S, Andrisic L, Tatzber F, Zarkovic N, et al. Trace elements and oxidative stress in hypertensive disorders of pregnancy. Arch Gynecol Obstet. 2013;287:19-24. https://doi.org/10.1007/s00404-012-2502-4
Some similar items:
- Edisson Rodríguez, Aura María Gil-Villa, Daniel Camilo Aguirre-Acevedo, Walter Cardona-Maya, Ángela P. Cadavid, Evaluation of atypical semen parameters in individuals whose couples had a history of early recurrent embryo death: in search for a reference value , Biomedica: Vol. 31 No. 1 (2011)
- Luis Miguel Sosa, Luz Libia Cala, Julio César Mantilla, Congenital tuberculosis associated with maternal disseminated miliary tuberculosis , Biomedica: Vol. 27 No. 4 (2007)
- Claudia Ayala, Reggie García, Edith Cruz, Karol Prieto, Marta Bermúdez, Homocysteine levels and polymorphisms of MTHFR and CBS genes in Colombian patients with superficial and deep venous thrombosis , Biomedica: Vol. 30 No. 2 (2010)
- Germán González, Marta Lía Valencia, Nelson Armando Agudelo, Liliana Acevedo, Isabel Cristina Vallejo, Perceived urgency of medical condition and use of health care services in Medellín, Colombia, 2005-2006 , Biomedica: Vol. 27 No. 2 (2007)
- Jairo Lizarazo, Melva Linares, Catalina de Bedout, Ángela Restrepo, Clara Inés Agudelo, Elizabeth Castañeda, Grupo Colombiano para el Estudio de la Criptococosis, Results of nine years of the clinical and epidemiological survey on cryptococcosis in Colombia, 1997-2005 , Biomedica: Vol. 27 No. 1 (2007)
- Berta Nelly Restrepo, María Teresa Restrepo, Juan Camilo Beltrán, Mónica Rodríguez, Ruth Emilia Ramírez, Nutritional status of indigenous children aged up to six years in the Embera-Katio Indian , Biomedica: Vol. 26 No. 4 (2006)
- Helena Hernández-Cuervo, Solangy Usme, Juan José Yunis, Frequently associated genotypes to thrombophilia , Biomedica: Vol. 34 No. 1 (2014)
- Stella Carrasco Rodríguez, Myriam Sanchez Gómez, Serum IGF-I and IGFBP-3 levels in pregnant adolescents in an economically depressed community , Biomedica: Vol. 21 No. 4 (2001)
- Diana Carolina Cáceres, Vilma Fabiola Izquierdo, Leonardo Mantilla, Jorge Jara, Martha Velandia, Epidemiologic profile of the population displaced by the internal armed conflict of the country in a neighborhood of Cartagena, Colombia, 2000. , Biomedica: Vol. 22 (2002): Suplemento 2
- Berta N. Restrepo, Diana M. Isaza, Clara L. Salazar, José L. Ramírez, Gloria E. Upegui, Marta Ospina, Ruth Ramírez, Prenatal and postnatal effects of dengue infection during pregnancy. , Biomedica: Vol. 23 No. 4 (2003)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























