Post-transplant lymphoproliferative disorders in a cohort of adult patients with a liver transplant from a reference hospital in Bogotá, Colombia
Abstract
Introduction: The post-transplant lymphoproliferative disorders (PTLD) are characterized by an uncontrolled pathological lymphoid proliferation as a consequence of transplant immunosuppression therapy.
Objective: To characterize the clinical and pathological characteristics of PTLD in a cohort of adult patients with liver transplant during a 15 year period at the Hospital Universitario Fundación Santa Fe de Bogota.
Materials and methods: We conducted an observational retrospective study by searching for the PTLD cases diagnosed during the study period in the databases of the Liver Transplantation Unit and the Pathology Department. We collected the epidemiological, clinical, and pathological information and performed the corresponding statistics analyses.
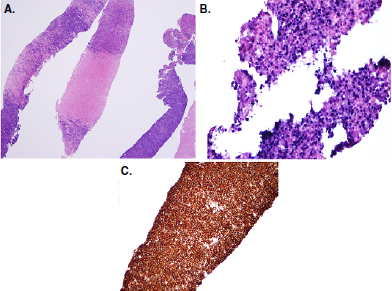
Results: During the research period, 572 patients were transplanted; the incidence of PTDL was 2.44%; 79% of them were man and the average age at the time of diagnosis was 62.5 years; 71% of the cases were diagnosed during the first year after the transplant and the same percentage EBV-seropositive patients. The most frequent pathological phenotype was monomorphic and the majority of tumors was detected in the hepatic hilum. The one-year survival was 50%.
Conclusion: The high proportion of early cases and the high frequency of Epstein-Barr virus seropositivity both in donors and receptors drewour attention. More studies are necessary to have a better understanding of this condition in Colombia. This is the first PTLD clinical and pathological analysis in liver-transplant patients from Colombia to date.
Downloads
References
Dierickx D, Cardinaels N. Posttransplant lymphoproliferative disorders following liver transplantation: Where are we now? World J Gastroenterol. 2015;21:11034-43. https://doi.org/10.3748%2Fwjg.v21.i39.11034
Doak PB, Montgomerie JZ, North JD, Smith F. Reticulum cell sarcoma after renal homotransplantation and azathioprine and prednisone therapy. Br Med J.1968;4:746-8. https://doi.org/10.1136%2Fbmj.4.5633.746
Starzl TE, Nalesnik MA, Porter KA, Ho M, Iwatsuki S, Griffith BP, et al. Reversibility of lymphomas and lymphoproliferative lesions developing under cyclosporin-steroid therapy. Lancet. 1984;1:583-7. https://doi.org/10.1016/s0140-6736(84)90994-2
Singavi AK, Harrington AM, Fenske TS. Post-transplant lymphoproliferative disorders. Cancer Treat Res. 2015;165:305-7. https://doi.org/10.1007/978-3-319-13150-4_13
Dharnidharka VR, Webster AC, Martínez OM, Preiksaitis JK, Leblond V, Choquet S. Posttransplant lymphoproliferative disorders. Nat Rev Dis Prim. 2016;2:1-20. https://doi.org/10.1038/nrdp.2015.88
Dharnidharka VR, Lamb KE, Gregg JA, Meier-Kriesche HU. Associations between EBV serostatus and organ transplant type in PTLD risk: An analysis of the SRTR National Registry Data in the United States. Am J Transplant. 2012;12:976-83. https://doi.org/10.1111/j.1600-6143.2011.03893.x
Luskin, MR, Heil DS, Tan KS, Choi S, Stadtmauer EA, Schuster SJ, et al. The impact of EBV status on characteristics and outcomes of post-transplantation lymphoproliferative disorder. Am J Transplant. 2015;15:2665-73. https://doi.org/10.1111/ajt.13324
Lee TC, Savoldo B, Rooney CM, Heslop HE, Gee AP, Caldwell Y, et al. Quantitative EBV viral loads and immunosuppression alterations can decrease PTLD incidence in pediatric liver transplant recipients. Am J Transplant. 2005;5:2222-8. https://doi.org/10.1111/j.1600-6143.2005.01002.x
Opelz G, Dohler B. Lymphomas after solid organ transplantation: A collaborative transplant study report. Am J Transplant. 2004;4:222-30 https://doi.org/10.1046/j.1600-6143.2003.00325.x
Jiang Y, Villeneuve PJ, Fenton SS, Schaubel DE, Lilly L, Mao Y. Liver transplantation and subsequent risk of cancer: Findings from a Canadian cohort study. Liver Transpl. 2008;14:1588-97. https://doi.org/10.1002/lt.21554
Benítez C, Londoño MC, Miquel R, Manzia TM, Abraldes JG, Lozano JJ, et al. Prospective multicenter clinical trial of immunosuppressive drug withdrawal in stable adult liver transplant recipients. Hepatology. 2013;58:1824-35. https://doi.org/10.1002/hep.26426
de la Garza RG, Sarobe P, Merino J, Lasarte JJ, D’Avola D, Belsue V, et al. Trial of complete weaning from immunosuppression for liver transplant recipients: Factors predictive of tolerance. Liver Transpl. 2013;19:937-44. https://doi.org/10.1002/lt.23686
Lu BR, Park KT, Hurwitz M, Cox KL, Berquist WE. Impact of immunosuppression on the development of Epstein-Barr virus (EBV) viremia after pediatric liver transplantation. Transplant Proc. 2013;45:301-4 https://doi.org/10.1016/j.transproceed.2012.04.035
Jain A, Nalesnik M, Reyes J, Pokharna R, Mazariegos G, Green M, et al. Post-transplant lymphoproliferative disorders in liver transplantation: A 20-year experience. Ann Surg. 2002;236:429-36. https://doi.org/10.1097/00000658-200210000-00005
Swerdlow SH, Campo E, Pileri SA, Harris NL, SteinH, Siebert R, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375-90. https://doi.org/10.1182/blood-2016-01-643569
Mendizábal M, Marciano S, dos Santos Schraiber L, Zapata R, Quiros R, Zanotelli ML, et al. Post-transplant lymphoproliferative disorder in adult liver transplant recipients: A South American multicenter experience. Clin Transplant. 2013:27:E469-77. https://doi.org/10.1111/ctr.12152
Mumtaz K, Faisal N, Márquez M, Healey A, Lilly LB, Renner EL. Post-transplant lymphoproliferative disorder in liver transplant recipients: Characteristics, management and outcome from a single-centre experience with >1000 liver transplantations. Can J Gastroenterol Hepatol. 2015;29:417-22. https://doi.org/10.1155/2015/517359
Kremers WK, Devarbhavi HC, Wiesner RH, Krom RA, Macon WR, Habermann TM. Posttransplant lymphoproliferative disorders following liver transplantation: Incidence, risk factors and survival. Am J Transplant. 2006;6:1017-24.
Lo RC, Chan SC, Chan KL, Chiang AK, Lo CM, Ng I. Post-transplant lymphoproliferative disorders in liver transplant recipients: A clinicopathological study. J Clin Pathol. 2013;66:392-8. https://doi.org/10.1136/jclinpath-2012-201139
Trofe J, Buell JF, Beebe TM, Hanaway MJ, First MR, Alloway RR, et al. Analysis of factors that influence survival with post-transplant lymphoproliferative disorder in renal transplant recipients: The Israel Penn International Transplant Tumor Registry experience. Am J Transplant. 2005;5:775-80. https://doi.org/10.1111/j.1600-6143.2005.00776.x
Caillard S, Lelong C, Pessione F, Moulin B. Post-transplant lymphoproliferative disorders occurring after renal transplantation in adults: Report of 230 cases from the French Registry. Am J Transplant. 2006;6:2735-42. https://doi.org/10.1111/j.1600-6143.2006.01540.x
Kinch A, Cavelier L, Bengtsson M, Baecklund E, Enblad G, Backlin C, et al. Donor or recipient origin of post-transplant lymphoproliferative disorders following solid organ transplantation. Am J Transplant. 2014;14:2838-45. https://doi.org/10.1111/ajt.12990
Sanz J, Arango M, Senent L, Jarque I, Montesinos P, Sempere A, et al. EBV-associated posttransplant lymphoproliferative disorder after umbilical cord blood transplantation in adults with hematological diseases. Bone Marrow Transplant. 2014;49:397-402. https://doi.org/10.1038/bmt.2013.190
Some similar items:
- María Adoración Martín-Gómez, Mercedes Caba-Molina, María José Viciana-Martínez-Lage, Rosa Ortega-Salas, Alicia Sánchez-Crespo, Manuel Jesús Soriano-Pérez, Mercedes Gómez-Morales, Collapsing glomerulonephritis with podocyte markers in hemophagocytic syndrome secondary to hepatosplenic T-cell lymphoma , Biomedica: Vol. 38 No. 4 (2018)
- Constanza Pardo, Ricardo Cendales, Survival analysis of cervical cancer patients , Biomedica: Vol. 29 No. 3 (2009)
- Raúl Murillo, Ricardo Cendales, Carolina Wiesner, Marion Piñeros, Sandra Tovar, Effectiveness of cytology-based cervical cancer screening in the Colombian health system , Biomedica: Vol. 29 No. 3 (2009)
- Sandra Lorena Girón, Julio César Mateus, Fabián Méndez, Impact of an open waste disposal site on the occurrence of respiratory symptoms and on health care costs of children , Biomedica: Vol. 29 No. 3 (2009)
- José Joaquín Carvajal, Ligia Inés Moncada, Mauricio Humberto Rodríguez, Ligia del Pilar Pérez, Víctor Alberto Olano, Characterization of Aedes albopictus (Skuse, 1894) (Diptera:Culicidae) larval habitats near the Amazon River in Colombia , Biomedica: Vol. 29 No. 3 (2009)
- Andrés Páez, Gloria Rey, Carlos Agudelo, Alvaro Dulce, Edgar Parra, Hernando Díaz-Granados, Damaris Heredia, Luis Polo, Outbreak of urban rabies transmitted by dogs in Santa Marta, northern Colombia , Biomedica: Vol. 29 No. 3 (2009)
- Patricia Escobar, Katherine Paola Luna, Indira Paola Hernández, César Mauricio Rueda, María Magdalena Zorro, Simon L. Croft, In vitro susceptibility of Trypanosoma cruzi strains from Santander, Colombia, to hexadecylphosphocholine (miltefosine), nifurtimox and benznidazole , Biomedica: Vol. 29 No. 3 (2009)
- Gustavo Pradilla, Julio César Mantilla, Reynaldo Badillo, Human rabies encephalitis by a vampire bat bite in an urban area of Colombia , Biomedica: Vol. 29 No. 2 (2009)
- Mauricio Beltrán, María Cristina Navas, María Patricia Arbeláez, Jorge Donado, Sergio Jaramillo, Fernando De la Hoz, Cecilia Estrada, Lucía del Pilar Cortés, Amalia de Maldonado, Gloria Rey, Seroprevalence of hepatitis B virus and human immunodeficiency virus infection in a population of multiply-transfused patients in Colombia , Biomedica: Vol. 29 No. 2 (2009)
- Rosa Magdalena Uscátegui, Adriana M. Correa, Jaime Carmona-Fonseca, Changes in retinol, hemoglobin and ferritin concentrations in Colombian children with malaria , Biomedica: Vol. 29 No. 2 (2009)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























