Sociodemographic determinants and mortality of premature newborns in a medium and low-income population in Colombia, 2017-2019
Abstract
Introduction. The birth of premature babies is a public health problem with a high impact on infant morbidity and mortality. About 40% of mortality in children under five years occurs in the first month of life.
Objective. To identify the association between maternal sociodemographic factors, premature birth, and mortality in newborns under 37 weeks in Santiago de Cali, 2017-2019.
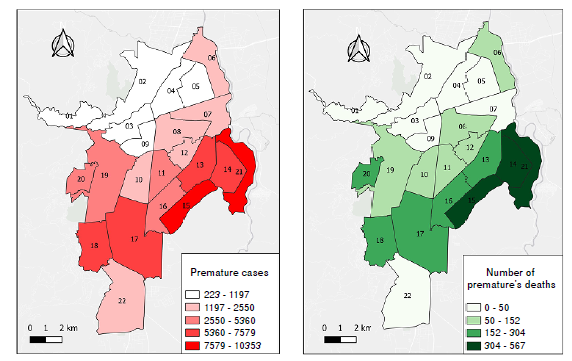
Materials and methods. We conducted a descriptive, cross-sectional study. We evaluated the records of Cali’s Municipal Public Health Office. We calculated the crude and adjusted odd ratios and confidence intervals (95%) using the logistic regression model, data processing in Stata 16, and georeferencing the cases in the QGIS software.
Results. From 2017 to 2019, premature babies in Cali corresponded to 11% of births. Poor prenatal care increased 3.13 times the risk of being born before 32 weeks (adjusted OR = 3.13; 95% CI = 2.75 - 3.56) and 1.27 times among mothers from outside the city (adjusted OR = 1.27; 95% CI = 1.15-1.41). Mortality was 4.29 per 1,000 live births. The mortality risk in newborns weighing less than 1,000 g increased 3.42 times (OR = 3.42; 95% CI = 2.85-4.12), delivery by cesarean section in 1.46 (OR = 1.46; CI 95% = 1.14-1.87) and an Apgar score – five minutes after birth– lower than seven in 1.55 times (OR = 1.55; CI 95% = 1.23-1.96).
Conclusions. We found that less than three prenatal controls, mothers living outside Cali, afro-ethnicity, and cesarean birth were associated with prematurity of less than 32 weeks. We obtained higher mortality in newborns weighing less than 1,000 g.
Downloads
References
Chawanpaiboon S, Vogel JP, Moller AB, Lumbiganon P, Petzold M, Hogan D, et al. Global, regional, and national estimates of levels of preterm birth in 2014: A systematic review and modelling analysis. Lancet Glob Health. 2019;7:e37-46. https://doi.org/10.1016/S2214-109X(18)30451-0
Wastnedge E, Waters D, Murray SR, McGowan B, Chipeta E, Nyondo-Mipando AL, et al. Interventions to reduce preterm birth and stillbirth, and improve outcomes for babies born preterm in low- and middle-income countries: A systematic review. J Glob Health. 2021;11:04050. https://doi.org/10.7189/jogh.11.04050
Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB, Narwal R, et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: A systematic analysis and implications. Lancet. 2012;379:2162-72. https://doi.org/10.1016/S0140-6736(12)60820-4
Martin RJ, Fanaroff AA, Walsh MC. Fanaroff and Martin’s Neonatal-Perinatal Medicine. 11th edition. Cleveland, OH: Elsevier; 2015. p.1856.
Markopoulou P, Papanikolaou E, Analytis A, Zoumakis E, Siahanidou T. Preterm birth as a risk factor for metabolic syndrome and cardiovascular disease in adult life: A systematic review and meta-analysis. J Pediatr. 2019;210:69-80. https://doi.org/10.1016/j.jpeds.2019.02.041
Crump C, Sundquist J, Winkleby MA, Sundquist K. Preterm birth and risk of chronic kidney disease from childhood into mid-adulthood: National cohort study. BMJ. 2019;365:1346. https://doi.org/10.1136/bmj.l1346
Ospino-Guzmán MP, Mercado-Reyes MM. Comportamiento de la prematuridad en Colombia durante los años 2007 a 2016. Bogotá; INS: 2007. Accessed: February 8, 2023. Available at: https://fundacioncanguro.co/wp-content/uploads/2018/11/Comportamiento-dela-prematuridad-en-Colombia-durante-los-a%C3%B1os-2007-a-2016.pdf
The Global Health Observatory. Estadísticas Sanitarias Mundiales. Ginebra: Organización Mundial de la Salud; 2022. Accessed: February 8, 2023. Available at: https://www.who.int/es/data/gho/publications/world-health-statistics
Oficina Sanitaria Panamericana, Organización Mundial de la Salud. CIE-10 Clasificación estadística internacional de enfermedades y problemas relacionados con la salud. Washington, D.C.: OPS-OMS; 1995. Accessed: February 8, 2023. Available at: https://iris.paho.org/bitstream/handle/10665.2/6282/Volume1.pdf
World Health Organization. Born too soon: The global action report on preterm birth. Geneva: WHO; 2012. Accessed: February 8, 2023. Available at: http://apps.who.int/iris/bitstream/handle/10665/44864/9789241503433_eng.pdf;jsessionid=C45F9897754A467E67CED827537FD757?sequence=1
Beck S, Wojdyla D, Say L, Betran AP, Merialdi M, Requejo JH, et al. The worldwide incidence of preterm birth: A systematic review of maternal mortality and morbidity. Bull World Health Organ. 2010;88:31-8. https://doi.org/10.2471/BLT.08.062554
Lawn JE, Gravett MG, Nunes TM, Rubens CE, Stanton C. Global report on preterm birth and stillbirth (1 of 7): definitions, description of the burden and opportunities to improve data. BMC Pregnancy Childbirth. 2010;10(Suppl.1):1-22. https://doi.org/10.1186/1471-2393-10-S1-S1
Organización Panamericana de la Salud. Indicadores básicos 2018. Situación de salud en las Américas. Washington: PAHO; 2018. Accessed: February 8, 2023. Available at: https://iris.paho.org/handle/10665.2/49511
Alexa D, Motta F. Informe de evento mortalidad perinatal y neonatal tardía, Colombia, 2020. Bogotá: Instituto Nacional de Salud; 2020. Accessed: February 8, 2023. Available at: https://www.ins.gov.co/buscador-eventos/Informesdeevento/MORTALIDAD%20PERINATAL%20Y%20NEONATAL%20TARD%C3%8DA_2020.pdf
Pungiluppi Leyva J. Informe de Gestión ICBF 2019. Bogotá: ICBF; 2020. Accessed: February 8, 2023. Available at: https://www.icbf.gov.co/informe-de-gestion-icbf-2019
Pusdekar YV, Patel AB, Kurhe KG, Bhargav SR, Thorsten V, Garcés A, et al. Rates and risk factors for preterm birth and low birthweight in the global network sites in six low- and low middle-income countries. Reprod Health. 2020;17(Suppl.3):S187. https://doi.org/10.1186/s12978-020-01029-z
Cali cómo vamos. Informe anual de calidad de vida. Santiago de Cali; 2021. Accessed: February 8, 2023. Available at: https://www.calicomovamos.org.co/_files/ugd/ba6905_2a6681f601a5475ebffbfc95788a108e.pdf
Alcaldía de Cali. Observatorio de Hacienda Pública Distrital. Santiago de Cali; 2021. Accessed: February 8, 2023. Available at: https://www.cali.gov.co/observatorios/publicaciones/168676/observatorio-de-hacienda-publica-distrital/
Ratzon R, Sheiner E, Shoham-Vardi I. The role of prenatal care in recurrent preterm birth. Eur J Obstet Gynecol Reprod Biol. 2011;154:40-4. https://doi.org/10.1016/j.ejogrb.2010.08.011
Althabe F, Belizán JM, McClure EM, Hemingway-Foday J, Berrueta M, Mazzoni A, et al. A population-based, multifaceted strategy to implement antenatal corticosteroid treatment versus standard care for the reduction of neonatal mortality due to preterm birth in low-income and middle-income countries: the ACT cluster-randomised trial. Lancet. 2015;385:629-39. https://doi.org/10.1016/S0140-6736(14)61651-2
Torres-Muñoz J, Jiménez-Fernández CA, Ortega RR, Cuero DJM, Mendoza DM. Factors associated with late prematurity in the University Hospital of Valle, Cali, Colombia, during 2013-2014. Front Public Health. 2020;8. https://doi.org/10.3389/fpubh.2020.00200
Goldenberg RL, Cliver SP, Mulvihill FX, Hickey CA, Hoffman HJ, Klerman LV, et al. Medical, psychosocial, and behavioral risk factors do not explain the increased risk for low birth weight among black women. Am J Obstet Gynecol. 1996;175:1317-24. https://doi.org/10.1016/s0002-9378(96)70048-0
Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371:75-84. https://doi.org/10.1016/S0140-6736(08)60074-4
Schaaf JM, Liem SMS, Mol BWJ, Abu-Hanna A, Ravelli ACJ. Ethnic and racial disparities in the risk of preterm birth: A systematic review and meta-analysis. Am J Perinatol. 2013;30:433-50. https://doi.org/1010.1055/s-0032-1326988
Lansky S, Friche AA, Silva AA, Campos D, Bittencourt SD, Carvalho ML, et al. Birth in Brazil survey: Neonatal mortality, pregnancy and childbirth quality of care. Cad Saúde Pública. 2014;30(Suppl.1):S192-207. https://doi.org/10.1590/0102-311x00133213
Defilipo EC, Chagas PSC, Ribeiro LC, Drumond CM. Factors associated with premature birth: A case-control study. Rev Paul Pediatr. 2022;40:e2020486. https://doi.org/10.1590/1984-0462/2022/40/2020486IN
Ip M, Peyman E, Lohsoonthorn V, Williams MA. A case-control study of preterm delivery risk factors according to clinical subtypes and severity. J Obstet Gynaecol Res. 2010;36:34-44. https://doi.org/10.1111/j.1447-0756.2009.01087.x
Instituto Nacional de Salud. Comportamiento epidemiológico del bajo peso al nacer a término, Colombia, semana epidemiológica 27 de 2020. Bogotá: Instituto Nacional de Salud; 2020. Accessed: February 8, 2023. Available at: https://www.ins.gov.co/buscadoreventos/BoletinEpidemiologico/2020_Boletin_epidemiologico_semana_28.pdf
Koullali B, Oudijk MA, Nijman TAJ, Mol BWJ, Pajkrt E. Risk assessment and management to prevent preterm birth. Semin Fetal Neonatal Med. 2016;21:80-8. https://doi.org/10.1016/j.siny.2016.01.005
Xu H, Dai Q, Xu Y, Gong Z, Dai G, Ding M, et al. Time trends and risk factor associated with premature birth and infants’ deaths due to prematurity in Hubei Province, China from 2001 to 2012. BMC Pregnancy Childbirth. 2015;15:1-9. https://doi.org/10.1186/s12884-015-0767-x
Grandi C, González A, Zubizarreta J. Factores perinatales asociados a la mortalidad neonatal en recién nacidos de muy bajo peso: estudio multicéntrico. Arch Argent Pediatr. 2016;5:426-33. https://doi.org/10.5546/aap.2016.426
Walani SR. Global burden of preterm birth. Int J Gynaecol Obstet. 2020;150:31-3. https://doi.org/10.1002/ijgo.13195
Cao G, Liu J, Liu M. Global, regional, and national incidence and mortality of neonatal preterm birth, 1990-2019. JAMA Pediatr. 2022;176:787-96. https://doi.org/10.1001/jamapediatrics.2022.1622
Cnattingius S, Johansson S, Razaz N. Apgar score and risk of neonatal death among preterm infants. N Engl J Med. 2020;383:49-57. https://doi.org/10.1056/NEJMoa1915075
Some similar items:
- Constanza Pardo, Ricardo Cendales, Survival analysis of cervical cancer patients , Biomedica: Vol. 29 No. 3 (2009)
- Raúl Murillo, Ricardo Cendales, Carolina Wiesner, Marion Piñeros, Sandra Tovar, Effectiveness of cytology-based cervical cancer screening in the Colombian health system , Biomedica: Vol. 29 No. 3 (2009)
- Sandra Lorena Girón, Julio César Mateus, Fabián Méndez, Impact of an open waste disposal site on the occurrence of respiratory symptoms and on health care costs of children , Biomedica: Vol. 29 No. 3 (2009)
- José Joaquín Carvajal, Ligia Inés Moncada, Mauricio Humberto Rodríguez, Ligia del Pilar Pérez, Víctor Alberto Olano, Characterization of Aedes albopictus (Skuse, 1894) (Diptera:Culicidae) larval habitats near the Amazon River in Colombia , Biomedica: Vol. 29 No. 3 (2009)
- Andrés Páez, Gloria Rey, Carlos Agudelo, Alvaro Dulce, Edgar Parra, Hernando Díaz-Granados, Damaris Heredia, Luis Polo, Outbreak of urban rabies transmitted by dogs in Santa Marta, northern Colombia , Biomedica: Vol. 29 No. 3 (2009)
- Patricia Escobar, Katherine Paola Luna, Indira Paola Hernández, César Mauricio Rueda, María Magdalena Zorro, Simon L. Croft, In vitro susceptibility of Trypanosoma cruzi strains from Santander, Colombia, to hexadecylphosphocholine (miltefosine), nifurtimox and benznidazole , Biomedica: Vol. 29 No. 3 (2009)
- Gustavo Pradilla, Julio César Mantilla, Reynaldo Badillo, Human rabies encephalitis by a vampire bat bite in an urban area of Colombia , Biomedica: Vol. 29 No. 2 (2009)
- Mauricio Beltrán, María Cristina Navas, María Patricia Arbeláez, Jorge Donado, Sergio Jaramillo, Fernando De la Hoz, Cecilia Estrada, Lucía del Pilar Cortés, Amalia de Maldonado, Gloria Rey, Seroprevalence of hepatitis B virus and human immunodeficiency virus infection in a population of multiply-transfused patients in Colombia , Biomedica: Vol. 29 No. 2 (2009)
- Rosa Magdalena Uscátegui, Adriana M. Correa, Jaime Carmona-Fonseca, Changes in retinol, hemoglobin and ferritin concentrations in Colombian children with malaria , Biomedica: Vol. 29 No. 2 (2009)
- Claudia M.E. Romero-Vivas, Luis Eduardo Castro, Lila Visbal, Ana María Santos, Esther Díaz, Cutaneous myiasis by Cochliomyia hominivorax (Coquerel) (Díptera Calliphoridae) in Hospital Universidad del Norte, Soledad, Atlántico , Biomedica: Vol. 29 No. 1 (2009)
Copyright (c) 2023 Biomedica

This work is licensed under a Creative Commons Attribution 4.0 International License.
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























