Candida auris: a global pathogen that has taken root in Colombia
Abstract
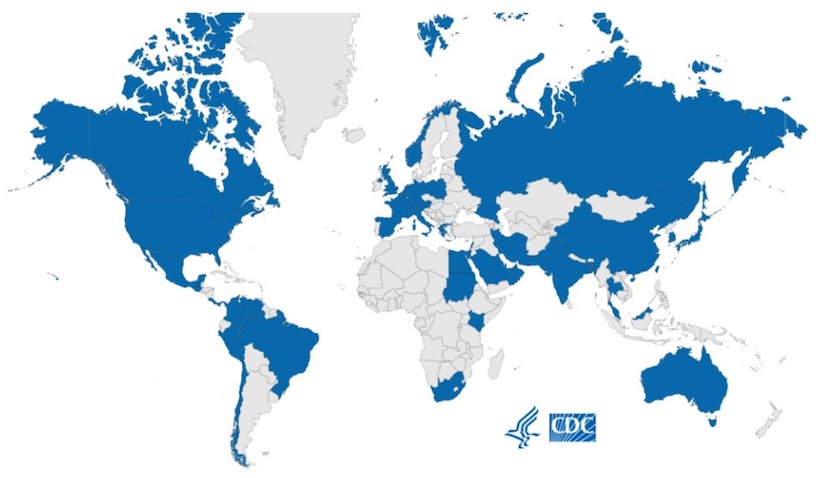
Candida auris has been recognized as an emerging multidrug-resistant pathogen with a significant public health burden, causing cases of invasive infection and colonization due to its persistence on inanimate surfaces, ability to colonize skin of some patients, and high transmissibility in healthcare settings.
The first sporadic report of the isolation of this species from the ear canal of a patient in Asia was in 2009 and reports from other regions of the world soon followed. However, it was not until 2015 that global epidemiological alerts were communicated as a result of an increasing number of reports of invasive infections caused by C. auris in several countries.
Colombia was soon added to this list in 2016 after an unusual increase in the number of C. haemulonii isolates was reported, later confirmed as C. auris. Since the issuing of a national alert by the Colombian National Institute of Health together with the Ministry of Health in 2016, the number of cases reported reached over 2,000 by 2022. Colombian isolates have not shown pan resistance to available antifungals, unlike C. auris strains reported in other regions of the world, which leaves patients in Colombia with therapeutic options for these infections. However, increasing fluconazole resistance is being observed. Whole-genome sequencing of Colombian C. auris isolates has enhanced molecular epidemiological data, grouping Colombian isolates in clade IV together with other South American isolates.
Downloads
References
Garcia-Bustos V, Cabanero-Navalon MD, Ruiz-Saurí A, Ruiz-Gaitán AC, Salavert M, Tormo MA, et al. What do we know about Candida auris? State of the art, knowledge gaps, and future directions. Microorganisms. 2021;9:2177. https://doi.org/10.3390/microorganisms9102177
Martinez-Parada I, Agudelo-Quintero E, Prado-Molina D, SernaTrejos J. Situación actual de Candida auris en Colombia, 2021. An Fac Med. 2021;82:242-3. https://doi.org/10.15381/anales.v82i3.21089
Alvárez C, Cortes J, Denning D. Burden of fungal infections in Colombia. J Fungi (Basel). 2018;4:41. https://doi.org/110.3390/jof4020041
Escandón P, Cáceres DH, Espinosa-Bode A, Rivera S, Armstrong P, Vallabhaneni S, et al. Notes from the Field: Surveillance for Candida auris - Colombia, September 2016–May 2017.MMWR Morb Mortal Wkly Rep. 2018;67:459-60. https://doi.org/10.15585/mmwr.mm6715a6
Escandón P, Cáceres D, Lizarazo D, Lockhart S, Megham L, Duarte C. Laboratory-based surveillance of Candida auris in Colombia, 2016-2020. Mycoses. 2022;65:222-5. https://doi.org/10.1111/myc.13390
Satoh K, Makimura K, Hasumi Y, Nishiyama Y, Uchida K, Yamaguchi H. Candida auris sp. nov., a novel ascomycetous yeast isolated from the external ear canal of an inpatient in a Japanese hospital. Microbiol Immunol. 2009;53:41-4. https://doi.org/10.1111/j.1348-0421.2008.00083.x
Chowdhary A, Sharma C, Duggal S, Agarwal K, Prakash A, Singh PK, et al. New clonal strain of Candida auris, Delhi, India. Emerg Infect Dis. 2013;19:1670-3. https://doi.org/10.3201/eid1910.130393
Magobo RE, Corcoran C, Seetharam S, Govender NP. Candida auris-associated candidemia, South Africa. Emerg Infect Dis. 2014; 20:1250-1. https://doi.org/10.3201/eid2007.131765
Calvo B, Melo ASA, Perozo-Mena A, Hernández M, Francisco EC, Hagen F, et al. First report of Candida auris in America: clinical and microbiological aspects of 18 episodes of candidemia. J Infect. 2016;73:369-74. https://doi.org/10.1016/j.jinf.2016.07.008
Lockhart SR, Etienne KA, Vallabhaneni S, Farooqi J, Chowdhary A, Govender, NP, et al. Simultaneous emergence of multidrug-resistant Candida auris on 3 continents confirmed by whole-genome sequencing and epidemiological analyses. Clin Infect Dis. 2017;64:134-40. https://doi.org/10.1093/cid/ciw691
Escandón P, Chow NA, Caceres DH, Gade L, Berkow EL, Armstrong P, et al. Molecular epidemiology of Candida auris in Colombia reveals a highly related, countrywide colonization with regional patterns in Amphotericin B resistance. Clin Infect Dis. 2019;68:15-21. https://doi.org/10.1093/cid/ciy411
Araúz AB, Cáceres DH, Santiago E, Armstrong P, Arosemena S, Ramos C, et al. Isolation of Candida auris from 9 patients in Central America: importance of accurate diagnosis and susceptibility testing. Mycoses. 2018;61:44-47. https://doi.org/10.1111/myc.12709
Schwartz IS, Hammond GW. First reported case of multidrug-resistant Candida auris in Canada. Can Commun Dis Rep. 2017;43:150-3. https://doi.org/10.14745/ccdr
Moreno MV, Simian ME, Villarroel J, Fuenzalida LM, Yarad MF, Soto A, et al. Primer aislamiento de Candida auris en Chile. Rev Chil Infectol. 2019;36:76773. https://doi.org/10.4067/S0716-10182019000600767
de Almeida JN, Francisco EC, Hagen F, Brandão IB, Pereira FM, Presta Dias PH, et al. Emergence of Candida auris in Brazil in a COVID-19 Intensive Care Unit. J Fungi. 2021;7:220. https://doi.org/10.3390/jof7030220
Villanueva-Lozano H, Treviño-Rangel R de J, González GM, Ramírez-Elizondo MT, Lara-Medrano R, Aleman-Bocanegra MC, et al. Outbreak of Candida auris infection in a COVID-19 Hospital in Mexico. Clin Microbiol Infect. 2021;27:813-6. https://doi.org/10.1016/j.cmi.2020.12.030
Lyman M, Forsberg K, Sexton DJ, Chow NA, Lockhart SR, Jackson BR, et al. Worsening spread of Candida auris in the United States, 2019 to 2021. Ann Intern Med. 2023;176:489-95. https://doi.org/10.7326/M22-3469
Morales-López SE, Parra-Giraldo CM, Ceballos-Garzón A, Martínez HP, Rodríguez GJ, Álvarez-Moreno CA, et al. Invasive infections with multidrug-resistant yeast Candida auris, Colombia. Emerg Infect Dis. 2017;23:162-4. https://doi.org/10.3201/eid2301.161497
Chakrabarti A, Sood P, Rudramurthy SM, Chen S, Kaur H, Capoor M, et al. Incidence, characteristics and outcome of ICU-acquired candidemia in India. Intensive Care Med. 2015;41:285-95. https://doi.org/10.1007/s00134-014-3603-2
Berrio I, Caceres DH, Coronell R W, Salcedo S, Mora L, Marin A, et al. Bloodstream infections with Candida auris among children in Colombia: clinical characteristics and outcomes of 34 cases. J Pediatric Infect Dis Soc. 2021; 10:151-4. https://doi.org/10.1093/jpids/piaa038.PMID: 32373928
Armstrong PA, Rivera SM, Escandon P, Caceres DH, Chow N, Stuckey MJ, et al. Hospital associated multicenter outbreak of emerging fungus Candida auris, Colombia, 2016. Emerg Infect Dis. 2019;25:1339-46. https://doi.org/10.3201/eid2507.180491
Parra-Giraldo CM, Valderrama SL, Cortes-Fraile G, Garzón JR, Ariza BE, Morio F, et al. First report of sporadic cases of Candida auris in Colombia.Int J Infect Dis. 2018;69:63-7. https://doi.org/10.1016/j.ijid.2018.01.034
Instituto Nacional de Salud. Alerta por emergencia global de infecciones invasivas causadas por la levadura multiresistente Candida auris. Accessed: May 12, 2023. Available from: https://www.ins.gov.co/BibliotecaDigital/alerta-global-de-infecciones-causadas-por-levaduramultirresistente-candida-auris.pdf
Kordalewska M, Zhao Y, Lockhart SR, Chowdhary A, Berrio I, Perlin DS. Rapid and accurate molecular identification of the emerging multidrug-resistant pathogen Candida auris. J Clin Microbiol. 2017;55:2445-52. https://doi.org/10.1128/JCM.00630-17
Instituto Nacional de Salud. Vigilancia por laboratorio de Candida auris, 2016-primer semestre 2018. Bogotá: Instituto Nacional de Salud; 2018.
Instituto Nacional de Salud. Vigilancia por laboratorio de Candida auris en Colombia 2018-2020. Bogotá: INS; 2020.
Instituto Nacional de Salud. Vigilancia por laboratorio de Candida auris en Colombia 2018-2021. Bogotá: INS; 2021
Caceres DH, Rivera SM, Armstrong PA, Escandón P, Chow NA, Ovalle MV, et al. Case-case comparison of Candida auris versus other Candida species bloodstream infections: results of an outbreak investigation in Colombia. Mycopathologia. 2020;185:917-923. https://doi.org/10.1007/s11046-020-00478-1
Alvarez-Moreno CA, Morales-López S, Rodriguez GJ, Rodriguez JY, Robert E, Picot C, et al. The mortality attributable to Candidemia in C. auris is higher than that in other Candida pecies: myth or reality? J Fungi (Basel). 2023;9:430. https://doi.org/10.3390/jof9040430
Roberts SC, Zembower TR, Ozer EA, Qi C. Genetic evaluation of nosocomial Candida auris transmission. J Clin Microbiol. 2021;59:e02252-20. https://doi.org/10.1128/JCM.02252-20
Safari F, Madani M, Badali H, Kargoshaie AA, Fakhim H, Kheirollahi M, et al. A chronic autochthonous fifth clade case of Candida auris otomycosis in Iran. Mycopathologia. 2022:187;121-7. https://doi.org/10.1007/s11046-021-00605-6
Chow NA, de Groot T, Badali H, Abastabar M, Chiller T, Meis JF. Potential fifth clade of Candida auris, Iran, 2018. Emerg Infect Dis. 2019:25:1780. https://doi.org/10.3201/eid2509.190686
Chow NA, Gade L, Tsay SV, Forsberg K, Greenko JA, Southwick KL, et al. Multiple introductions and subsequent transmission of multidrug-resistant Candida auris in the USA: a molecular epidemiological survey. Lancet Infect Dis. 2018:18;137784. https://doi.org/10.1016/S1473-3099(18)30597-8
Chow NA, Muñoz JF, Gade L, Berkow EL, Li X, Welsh RM, et al. Tracing the evolutionary history and global expansion of Candida auris using population genomic analyses. mBio. 2020;11:e03364-19. https://doi.org/10.1128/mBio.03364-19
De Luca DG, Alexander DC, Dingle TC, Dufresne PJ, Hoang LM, Kus JV, et al. Four genomic clades of Candida auris identified in Canada, 2012-2019. Med Mycol. 2022:60. https://doi.org/10.1093/mmy/myab079
González-Duran E, Contreras-Pérez CU, Cáceres D, Ríos-Rosas C, Pinon-Ortega J, Téllez-Saucedo MD, et al. The use of readily available laboratory tests for the identification of the emerging yeast Candida auris in Mexico. Arch Microbiol. 2022:204;592. https://doi.org/10.1007/s00203-022-03159-3
Naicker SD, Maphanga TG, Chow N, Allam M, Kwenda S, Ismail A, et al. Clade distribution of Candida auris in South Africa using whole genome sequencing of clinical and environmental isolates. Emerg Microbes Infect. 2021:10;1300-8. https://doi.org/10.1080/22221751.2021.1944323
Rudramurthy SM, Chakrabarti A, Paul RA, Sood P, Kaur H, Capoor MR, et al. Candida auris candidaemia in Indian ICUs: analysis of risk factors. J Antimicrob Chemother. 2017:72;1794-801. https://doi.org/10.1093/jac/dkx034
Sharma C, Kumar N, Pandey R, Meis JF, Chowdhary A. Whole genome sequencing of emerging multidrug resistant Candida auris isolates in India demonstrates low genetic variation. New Microbes New Infect. 2016;13;77-82. https://doi.org/10.1016/j.nmni.2016.07.003
Misas E, Escandón P, McEwen JG, Clay OK. The LUFS domain, its transcriptional regulator proteins, and drug resistance in the fungal pathogen Candida auris. Protein Sci. 2019;28:2024-9. https://doi.org/10.1002/pro.3727
Healey KR, Kordalewska M, Jiménez Ortigosa C, Singh A, Berrío I, Chowdhary A, et al. Limited ERG11 mutations identified in isolates of Candida auris directly contribute to reduced azole susceptibility. Antimicrob Agents Chemother. 2018;62:e01427-18. https://doi.org/10.1128/AAC.01427-18
Organización Mundial de la Salud. WHO fungal priority pathogens list to guide research, development and public health action. Geneva: WHO; 2022.
Some similar items:
- Constanza Pardo, Ricardo Cendales, Survival analysis of cervical cancer patients , Biomedica: Vol. 29 No. 3 (2009)
- Raúl Murillo, Ricardo Cendales, Carolina Wiesner, Marion Piñeros, Sandra Tovar, Effectiveness of cytology-based cervical cancer screening in the Colombian health system , Biomedica: Vol. 29 No. 3 (2009)
- Sandra Lorena Girón, Julio César Mateus, Fabián Méndez, Impact of an open waste disposal site on the occurrence of respiratory symptoms and on health care costs of children , Biomedica: Vol. 29 No. 3 (2009)
- José Joaquín Carvajal, Ligia Inés Moncada, Mauricio Humberto Rodríguez, Ligia del Pilar Pérez, Víctor Alberto Olano, Characterization of Aedes albopictus (Skuse, 1894) (Diptera:Culicidae) larval habitats near the Amazon River in Colombia , Biomedica: Vol. 29 No. 3 (2009)
- Andrés Páez, Gloria Rey, Carlos Agudelo, Alvaro Dulce, Edgar Parra, Hernando Díaz-Granados, Damaris Heredia, Luis Polo, Outbreak of urban rabies transmitted by dogs in Santa Marta, northern Colombia , Biomedica: Vol. 29 No. 3 (2009)
- Patricia Escobar, Katherine Paola Luna, Indira Paola Hernández, César Mauricio Rueda, María Magdalena Zorro, Simon L. Croft, In vitro susceptibility of Trypanosoma cruzi strains from Santander, Colombia, to hexadecylphosphocholine (miltefosine), nifurtimox and benznidazole , Biomedica: Vol. 29 No. 3 (2009)
- Gustavo Pradilla, Julio César Mantilla, Reynaldo Badillo, Human rabies encephalitis by a vampire bat bite in an urban area of Colombia , Biomedica: Vol. 29 No. 2 (2009)
- Mauricio Beltrán, María Cristina Navas, María Patricia Arbeláez, Jorge Donado, Sergio Jaramillo, Fernando De la Hoz, Cecilia Estrada, Lucía del Pilar Cortés, Amalia de Maldonado, Gloria Rey, Seroprevalence of hepatitis B virus and human immunodeficiency virus infection in a population of multiply-transfused patients in Colombia , Biomedica: Vol. 29 No. 2 (2009)
- Rosa Magdalena Uscátegui, Adriana M. Correa, Jaime Carmona-Fonseca, Changes in retinol, hemoglobin and ferritin concentrations in Colombian children with malaria , Biomedica: Vol. 29 No. 2 (2009)
- Claudia M.E. Romero-Vivas, Luis Eduardo Castro, Lila Visbal, Ana María Santos, Esther Díaz, Cutaneous myiasis by Cochliomyia hominivorax (Coquerel) (Díptera Calliphoridae) in Hospital Universidad del Norte, Soledad, Atlántico , Biomedica: Vol. 29 No. 1 (2009)
Copyright (c) 2023 Biomedica

This work is licensed under a Creative Commons Attribution 4.0 International License.
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























